Every year, over 350,000 preventable medication errors happen in nursing homes alone - and most of them occur right in the home. Seniors are more likely to take multiple medications, have slower metabolism, and face memory challenges. That’s why medication safety isn’t just a good idea - it’s a necessity.
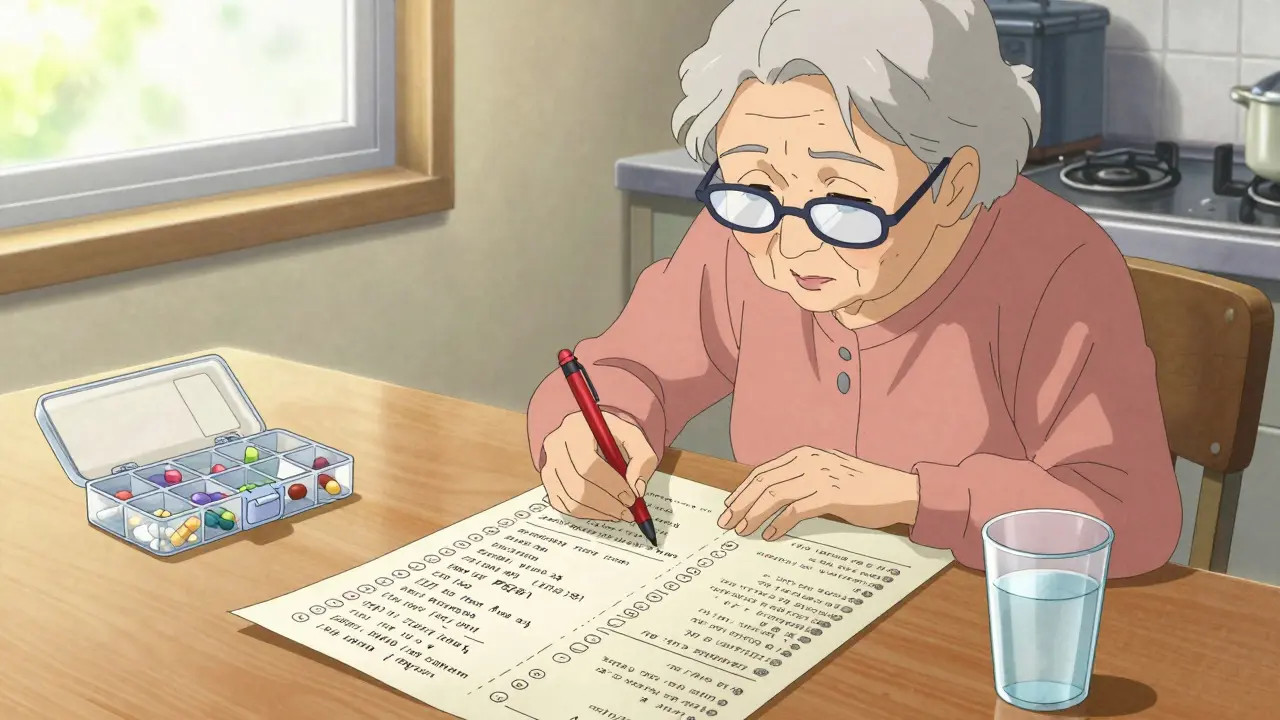
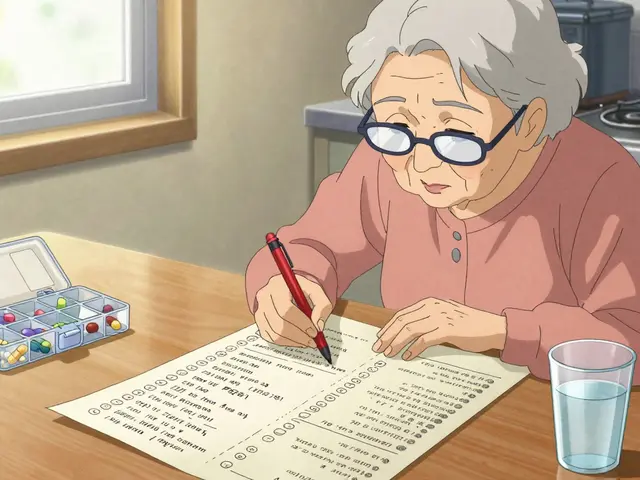
Keep a Real-Time Medication List
A simple piece of paper can save a life. But it has to be accurate and up to date. Don’t just write down what your doctor prescribed. Include every pill, vitamin, supplement, and over-the-counter drug. That means aspirin, calcium, fish oil, melatonin, and even herbal teas with medicinal effects.The Health in Aging Foundation says a complete list needs 10 details: medication name, dosage, how often to take it, why it was prescribed, when you started, who prescribed it, the pharmacy’s phone number, special instructions (like "take with food"), known side effects, and expiration dates.
Update this list within 24 hours of any change - whether it’s a new prescription, a dose adjustment, or stopping something. Bring it to every appointment, even if the doctor says they already have it. A 2022 survey found that 92% of pharmacists say this habit stops dangerous drug interactions before they happen.
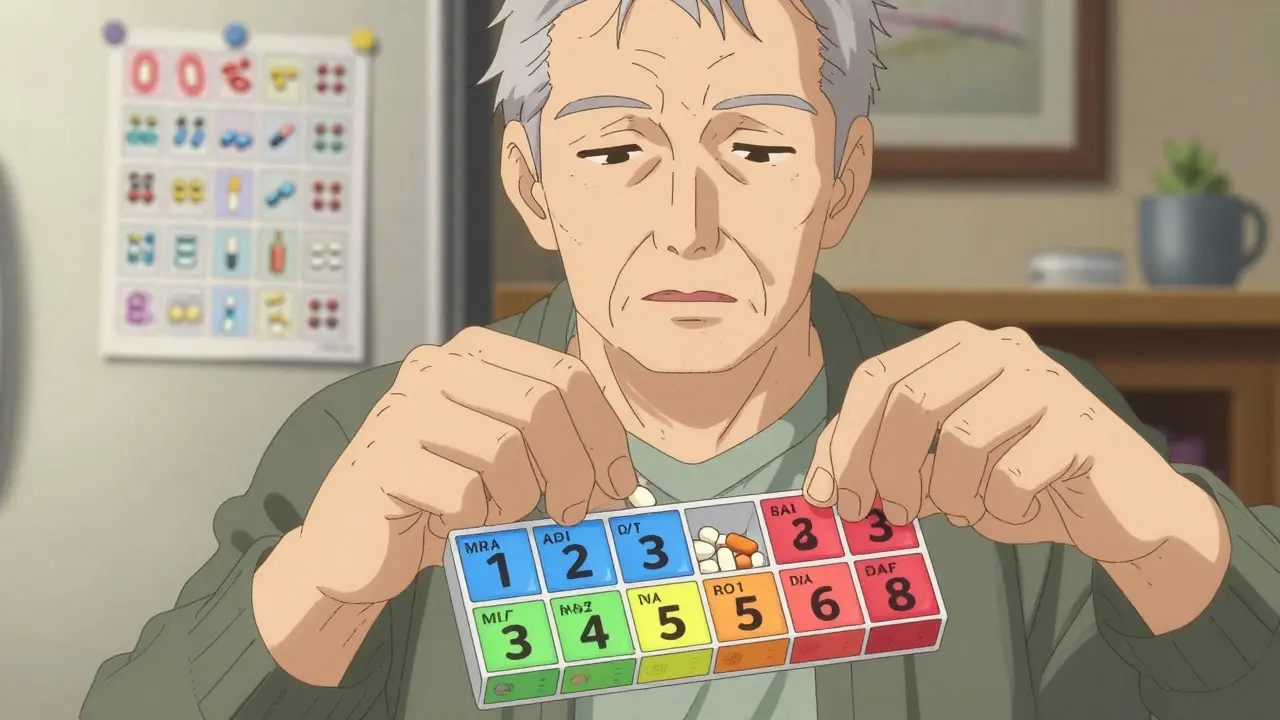
Use a Pill Organizer - But Choose the Right One
Pill organizers aren’t just for seniors with memory problems. They help anyone who takes more than three medications a day. The key is matching the organizer to the person’s needs.Start simple. A single-compartment daily organizer works for someone who takes pills once a day. For those on multiple doses, go for a 7-day AM/PM model. Color-coded compartments (blue for morning, red for evening) help people with mild cognitive issues stay on track. A 2021 NIA study showed color-coded systems improved adherence by 47% in seniors with early memory loss.
But don’t just buy any organizer. Look for ones with large print, easy-open lids, and locking features. Some caregivers report their loved ones accidentally double-dosing because they forgot they already took a pill. A locked organizer solved that for one family - their mother’s missed doses dropped from 40% to 5% per month.
Some seniors prefer low-tech solutions. One man’s daughter made a laminated chart with photos of each pill next to its name and purpose. His anxiety about taking unfamiliar meds dropped by 80%. AARP’s 2023 survey found 55% of seniors over 75 trust written schedules more than apps.
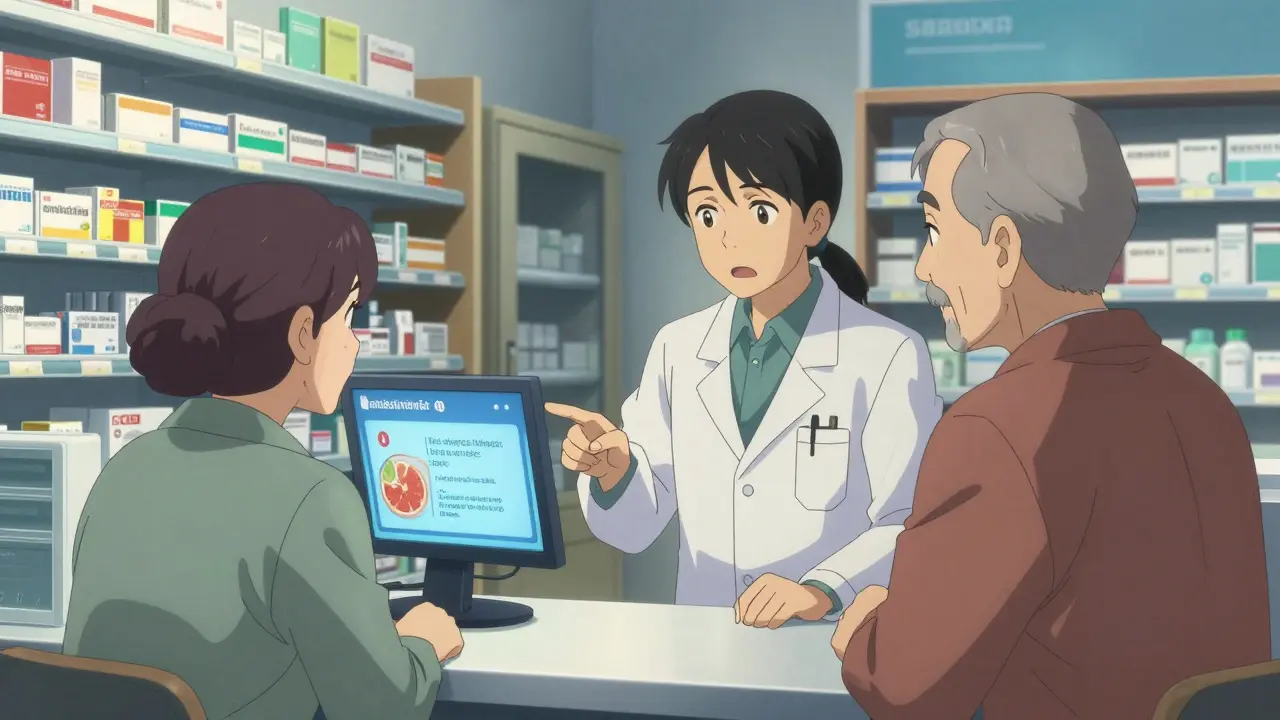
Check for Dangerous Interactions
It’s not just about what’s in the pill - it’s what’s in your glass, your plate, or your other meds.Grapefruit juice interacts with 85 commonly prescribed drugs, including statins for cholesterol and blood pressure medications. One glass can cause dangerous spikes in drug levels. Alcohol is even more dangerous - it interacts with over 150 medications, including sleep aids, antidepressants, and diabetes pills. Even a single drink can cause dizziness, low blood sugar, or fainting.
The American Geriatrics Society updates the Beers Criteria every two years. The 2023 version lists 138 medications that are risky for seniors, including benzodiazepines (like Xanax), anticholinergics (like Benadryl), and long-term NSAIDs (like ibuprofen). These drugs can cause confusion, falls, and kidney damage.
Before starting any new medication - even something bought without a prescription - ask: "Does this interact with anything I’m already taking?" Pharmacists can run these checks in seconds. Use the free Medscape or Drugs.com interaction checker if you’re unsure.
Store Medications Properly - Not in the Bathroom
Most seniors keep their meds in the bathroom cabinet. It’s convenient. But it’s also the worst place.Steam from showers and sinks raises humidity and temperature. A 2022 University of Florida study found that 37% of common medications degrade faster in bathroom conditions. Pills can crumble, liquids can separate, and patches can lose stickiness.
The FDA recommends storing all medications between 68°F and 77°F (20-25°C), away from moisture and direct sunlight. A kitchen cabinet away from the stove or a bedroom drawer works better.
And if you have grandchildren visiting - lock it up. The Poison Control Center reports 60,000 accidental poisonings in children each year from unlocked medicine cabinets. Even if your grandkids don’t live with you, a weekend visit is enough for disaster.
Also, clean out your medicine cabinet every six months. The average senior home holds $317 worth of expired or unused pills. Flushing them isn’t safe. Take them to a pharmacy drop box or a local take-back event.
Ask the Right Questions at Every Appointment
Doctors don’t always know what you’re taking. Nurses forget. Pharmacies don’t always connect the dots. You have to speak up.Prepare four questions before every visit:
- Is this medication still necessary?
- What interactions should I watch for?
- Are there lower-cost alternatives?
- What are the signs of dangerous side effects?
These aren’t just polite questions - they’re life-saving. The Alzheimer’s Association found that structured communication reduces medication errors by 63% in dementia patients.
Also, ask about deprescribing. Many seniors take medications they no longer need - like blood pressure pills after a heart attack has stabilized, or statins when cholesterol is normal. The American Geriatrics Society recommends reviewing all meds annually to remove unnecessary ones. One study showed that simplifying a regimen from four doses a day to one dose increased adherence from 50% to 90%.
Don’t be afraid to say: "I’m taking too many pills. Can we cut some?"
What Works in Real Life
Real caregivers share real solutions. One woman created a daily checklist taped to the fridge: "8 AM - Blood pressure pill. 12 PM - Diabetic pill. 6 PM - Pain pill." She used sticky notes with her mom’s handwriting. Her mom could read it even when confused.Another family used a Hero smart dispenser - it beeps, lights up, and texts the caregiver if a dose is missed. But one user on Reddit said their $100 app didn’t work because their mom kept dismissing alerts without taking pills. The app didn’t notify the caregiver until she had a low blood sugar episode.
Technology helps - but only if it fits the person. A pill organizer with big labels and a locked lid worked better for one 88-year-old than any app.
Establishing a routine takes 21 to 30 days. Do it at the same time every day - after breakfast, before bed. Pair medication with a daily habit like brushing teeth or drinking coffee. Visual cues like a marked calendar or a daily alarm help more than memory.
The Medicare Part D program now offers free Medication Therapy Management for people on 8 or more medications. Ask your pharmacist if you qualify. And starting in 2026, Medicare Advantage plans will be scored partly on how well they prevent medication errors - so they’ll be pushing these practices harder than ever.
What should I do if my senior parent skips a dose?
Don’t double the next dose unless a doctor says to. Call the prescribing doctor or pharmacist immediately. Most medications have specific instructions for missed doses - some can be taken later that day, others should be skipped. Keep a log of missed doses to show at the next appointment.
Can I crush pills to make them easier to swallow?
Only if the label or pharmacist says it’s safe. Many pills - especially extended-release or enteric-coated ones - lose their effectiveness or become dangerous if crushed. A 2022 University of Michigan study found 22% of home caregivers crushed pills without knowing the risks. Always check before crushing.
Are there free tools to help manage medications?
Yes. The National Institute on Aging offers a free Medication Management Toolkit with printable forms and checklists. Many pharmacies provide free large-print labels and medication schedules. The FDA’s Safe Use Initiative partners with over 7,200 pharmacies nationwide to offer these services at no cost.
How do I know if a medication is no longer needed?
Ask your doctor to do a "medication review" at least once a year. Look for pills prescribed for short-term issues (like pain after surgery) that are still being taken months later. Also, watch for side effects that started after a new drug was added. The American Geriatrics Society’s deprescribing guidelines help doctors safely reduce unnecessary meds - especially those linked to falls, confusion, or kidney problems.
What’s the biggest mistake caregivers make?
Assuming the senior understands everything. Many seniors don’t tell you they’re confused, scared, or having side effects. They don’t want to be a burden. The biggest mistake is not asking open-ended questions like, "What’s been hard about taking your pills?" instead of "Are you taking your meds?"
If you’re managing medications for a senior, you’re doing critical work. These five tips - a real-time list, the right organizer, checking interactions, proper storage, and asking questions - aren’t just best practices. They’re the difference between staying independent and ending up in the hospital. Start with one. Then add another. Progress, not perfection, keeps seniors safe.







Kuldipsinh Rathod
December 26, 2025 AT 09:01I’ve been helping my 82-year-old uncle manage his meds for three years now. The pill organizer with the locked lid? Game changer. He used to take two doses by accident-now it’s zero. No apps, no fancy tech. Just a simple plastic box with big labels and a key. Sometimes the old ways are the best ways.
Matthew Ingersoll
December 27, 2025 AT 08:47That bathroom storage point is so true. My grandmother kept her insulin in the cabinet above the sink. One winter, the humidity made the vials cloudy. We didn’t realize until her blood sugar spiked. Now everything’s in a sealed container in her bedroom drawer. Simple fix. Big difference.
Jody Kennedy
December 28, 2025 AT 00:53Just started using the free NIA toolkit last week. Printed the checklist, laminated it, and taped it to the fridge next to the milk. My mom can’t read small print anymore, but she can see the big words. She even started checking off the boxes herself. Small win, but it feels huge.
christian ebongue
December 29, 2025 AT 02:24Crushing pills without asking? Yeah, that’s a thing. My cousin did it with her dad’s blood thinner. He ended up in ER. Don’t be that person. Ask the pharmacist. Seriously. It’s free.
Joanne Smith
December 29, 2025 AT 12:37Let’s be real-half the time, the doctor doesn’t even know what the patient’s taking. I had to hand my mom’s entire med list to her cardiologist, and he said, ‘Huh. I didn’t know she was on that.’ So yeah, bring the damn list. Even if they say they have it. They don’t.
Ryan Cheng
December 30, 2025 AT 02:29The ‘ask four questions’ thing? Brilliant. I started doing this with my dad’s annual checkup. Turned out he was still on a blood thinner he didn’t need anymore. Got it dropped. Saved him from a bleeding risk. Also saved $400 a year. Win-win.
carissa projo
December 31, 2025 AT 15:01There’s something sacred about a handwritten sticky note on the fridge. It’s not just a reminder-it’s a love letter from one generation to another. My aunt used to write her meds in her own looping cursive, with little hearts next to the ones she hated taking. ‘For my heart,’ she’d scribble. And when she forgot, she’d just look up and see that heart. That’s not tech. That’s humanity.
And the silence? The quiet way elders don’t say they’re confused? That’s the real crisis. We ask, ‘Are you taking your meds?’ like it’s a checkbox. But what we should ask is, ‘What’s the hardest part about this?’ And then shut up and listen. Really listen. The answer isn’t always in the pills-it’s in the fear, the pride, the loneliness.
Deprescribing isn’t about cutting pills. It’s about restoring dignity. It’s saying, ‘You don’t have to carry this anymore.’ And sometimes, the most powerful medicine is the one you stop.
SHAKTI BHARDWAJ
January 2, 2026 AT 06:47Ugh. So much of this is just corporate wellness fluff. Who even has time to update a 10-point list? My grandma’s meds are on a napkin taped to the fridge with duct tape. And guess what? She’s fine. The system is broken, not the seniors. Stop blaming the elderly for a healthcare industry that doesn’t care.
And ‘lock your meds’? My cousin’s kid got into the cabinet and ate two Tylenol. Big deal. Took him to the ER. They gave him charcoal and sent him home. Kids are resilient. Stop treating your family like fragile china.
Also-why are we still using ‘pill organizers’? That’s a 1980s solution. We have smart fridges that order groceries. Why aren’t we automating this? Because Big Pharma doesn’t want you to be independent. They want you dependent. On them. On pills. On confusion.
david jackson
January 3, 2026 AT 08:41Let me tell you about the time my dad took his blood pressure pill at 6 a.m., then again at 8 a.m. because he couldn’t remember if he’d already taken it. He was shaking. He thought he was having a stroke. We rushed him to the hospital. Turned out he’d taken it twice. The doctor said, ‘This happens every single week.’ And then he handed us a $120 smart pill dispenser. It beeped. It flashed. It texted me. And my dad? He hated it. Called it ‘the robot that yells at me.’ So we threw it in the closet. Bought a $15 pill box with a lid that clicks. Now he takes it with his coffee. No beeping. No texts. Just coffee. And peace.
Technology doesn’t fix human problems. It just adds noise. The real solution? Routine. Repetition. Ritual. A cup of tea. A calendar. A voice saying, ‘Here, Dad. Your pill. I’m right here.’ That’s what keeps people safe. Not apps. Not lists. Presence.
And the bathroom? Oh my god, the bathroom. I found my mom’s expired Xanax in the shower caddy. It was moldy. I threw it out. She didn’t even notice. She just kept reaching for it. That’s not forgetfulness. That’s grief. She’s still trying to hold onto the person she was before all the pills.
We’re not managing medications. We’re managing loss. And sometimes, the most important thing isn’t the pill-it’s the hand that holds it.
jesse chen
January 4, 2026 AT 06:37I’ve been using the free Medscape checker for months now. It’s saved me twice-once when my aunt was prescribed a new antibiotic that clashed with her blood thinner, and again when she started taking a new herbal tea for sleep. Turns out it had kava, which is a no-go with her liver meds. Pharmacists are amazing. Use them. They’re not just there to hand out pills.
Also-don’t forget to check expiration dates. I found a bottle of gabapentin from 2018 in my uncle’s drawer. It looked fine. But it wasn’t. He’d been taking it for nerve pain. We tossed it. He’s fine. No side effects. But still. Better safe than sorry.
Angela Spagnolo
January 5, 2026 AT 12:59...i just... i wrote down all the meds on a piece of paper... and then i lost it... and then i cried... and then i rewrote it... and then i laminated it... and then i put it in a ziplock... and then i made a copy... and then i gave one to my sister... and then i gave one to the pharmacy... and then i gave one to my mom's neighbor... and then i still worry every night that she'll take the wrong one... and i know i'm overdoing it... but what if... what if... what if...?
Sarah Holmes
January 6, 2026 AT 01:12How dare you suggest that seniors are responsible for their own safety? This entire article is a grotesque misdirection. The real issue is the systemic abandonment of elder care in this country. We outsource responsibility to pill organizers and checklists while ignoring the fact that no one is paid to sit with the elderly, to watch them, to hold their hand as they forget which pill is which. This isn’t about medication management-it’s about moral failure. And you, dear author, are complicit in the lie that a laminated chart can replace dignity.
Prasanthi Kontemukkala
January 6, 2026 AT 15:49My grandmother is 87 and lives alone. We use a simple system: every morning, I call her at 8 a.m. She answers, I say, ‘Did you take your pills?’ She says, ‘Yes.’ I say, ‘Good. Now drink your water.’ She says, ‘I did.’ And we hang up. No app. No organizer. Just a 30-second call. She feels seen. And I feel like I’m doing something real. Sometimes, the most powerful tool is just a voice on the other end of the line.
christian ebongue
January 8, 2026 AT 13:32That 30-second call? Genius. I’m stealing that.