When you’re diagnosed with osteoporosis, your doctor’s main goal is simple: stop your bones from breaking. Osteoporosis weakens bone structure, making even a minor fall or sneeze potentially dangerous. For millions of people, especially women over 65, bisphosphonates like alendronate (Fosamax), risedronate (Actonel), and zoledronic acid (Reclast) have been the go-to solution for over 25 years. They work by slowing down the cells that break down bone, giving your skeleton a chance to rebuild. The results are clear: alendronate cuts hip fracture risk by more than half over just a few years. But there’s a quiet, rarely talked-about risk that keeps some patients up at night - jaw necrosis.
What Exactly Is Jaw Necrosis?
Jaw necrosis, officially called medication-related osteonecrosis of the jaw (MRONJ), happens when the bone in your jaw dies and becomes exposed. It doesn’t show up overnight. It usually starts with a small patch of bone sticking out in your gums - often after a tooth extraction, deep cleaning, or even a poorly fitted denture. The area doesn’t heal. It might hurt, get infected, or just sit there, unchanged, for months. The diagnosis is straightforward: exposed bone in the mouth that lasts longer than eight weeks, with no history of radiation therapy.
It’s rare. Really rare. For someone taking oral bisphosphonates for osteoporosis, the chance is about 0.7 out of every 100,000 people per year. That’s less than one in a million. Compare that to the risk of breaking a hip - which for someone with osteoporosis can be as high as 20% over five years - and the numbers shift dramatically. But rarity doesn’t mean insignificance. When MRONJ happens, it’s serious. Treatment can involve months of antibiotics, surgical removal of dead bone, and long-term dental care. Some people never fully recover.
Why the Jaw? It’s Not Just Any Bone
Why does this happen in the jaw and not the hip or spine? It comes down to biology. The jawbone turns over 10 times faster than the bones in your legs or spine. It’s constantly being remodeled because of chewing, talking, and the constant presence of bacteria in your mouth. Bisphosphonates stick to bone tissue, especially where remodeling is active. The jawbone ends up with a higher concentration of the drug than other areas.
On top of that, your mouth is a dirty place. Even with good hygiene, bacteria live in your gums. If you have gum disease or an infected tooth, that’s a constant source of inflammation. Bisphosphonates don’t just slow bone loss - they also reduce blood flow to bone and block healing. So when an injury happens - like pulling a tooth - the jaw can’t repair itself. The bone dies. The infection takes hold. And it won’t go away without help.
Oral vs. IV: The Risk Difference Is Huge
Not all bisphosphonates are the same. The biggest risk isn’t from the pills you swallow - it’s from the IV infusions. People with cancer who get zoledronic acid every few weeks are at much higher risk. One 2024 study of breast cancer patients found 12% developed jaw necrosis when using denosumab (Prolia), and 16% when switching from bisphosphonates to denosumab.
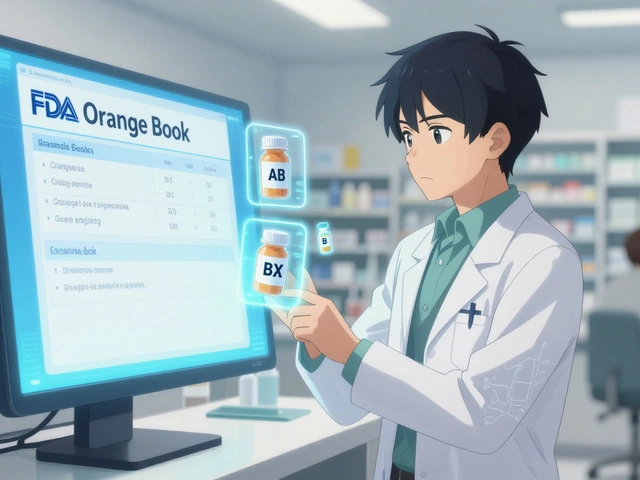
But for osteoporosis? The numbers are tiny. Oral bisphosphonates - the kind most people take - show almost no increased risk compared to people not taking them. A 2011 study of over 260,000 osteoporosis patients found no higher rate of jaw necrosis in those on alendronate. Even the FDA’s warnings are careful: they note the risk exists, but stress it’s far more common in cancer patients getting high doses.
Still, the fear lingers. Why? Because it’s dramatic. A dentist finds exposed bone. You panic. You Google it. And suddenly, every ache in your jaw feels like the start of something terrible.

The Real Danger: Skipping Dental Care
The biggest mistake patients make isn’t taking the medication - it’s avoiding the dentist because they’re scared. A 2023 survey by the American Association of Oral and Maxillofacial Surgeons found 63% of MRONJ cases in osteoporosis patients happened after a tooth extraction. That doesn’t mean the drug caused it. It means the tooth was already infected or loose, and the body couldn’t heal after removal.
Here’s the truth: if you have active gum disease, cavities, or loose teeth before starting bisphosphonates, your risk goes up. That’s why the American Dental Association recommends a full dental exam - including X-rays - before you start treatment. Fix the problems first. Get your mouth healthy. Then begin the medication. After that, keep seeing your dentist. Twice a year. No exceptions.
Some dentists, afraid of liability, refuse to do even routine cleanings on bisphosphonate users. That’s wrong. Cleanings, fillings, crowns - these are safe. The real danger is invasive surgery without preparation. If you need an extraction, your dentist and doctor should talk. Sometimes, a short drug holiday - stopping the bisphosphonate for 3 to 6 months - helps. But here’s the catch: stopping the drug raises your fracture risk by nearly 30%. So it’s not a simple fix.
What About Denosumab (Prolia)?
Denosumab is newer. It’s not a bisphosphonate. It’s an antibody that blocks a different bone-breakdown signal. It’s just as good at preventing fractures - maybe even better in some cases. But its risk for jaw necrosis is higher than oral bisphosphonates. Studies show it’s 1.7 to 2.5 times more likely to cause MRONJ. And unlike bisphosphonates, which stay in your bones for years, denosumab leaves your system fast. That means if you stop it, your bone loss can rebound quickly. So skipping doses isn’t an option.
For many, denosumab is a good alternative - especially if bisphosphonates cause stomach upset. But it’s not safer when it comes to jaw health. You still need to keep your mouth in top shape.
When Should You Worry? The Red Flags
Most people on bisphosphonates will never see a single symptom. But if you notice any of these, call your dentist right away:
- Exposed bone in your gums that doesn’t go away after two weeks
- Pain, swelling, or pus around a tooth or extraction site
- Loose teeth without any obvious reason
- A numb feeling or tingling in your jaw
Stage 1 MRONJ is just exposed bone - no pain, no infection. Stage 2 includes pain and infection. Stage 3? That’s when the bone breaks, or the infection spreads to your face or neck. Catching it early makes a huge difference. Early cases can heal with antibiotics and mouth rinses. Late cases need surgery.
What’s the Bottom Line?
Let’s cut through the noise. If you have osteoporosis and your doctor recommends a bisphosphonate, the benefits almost always outweigh the risks. Your chance of breaking a hip, spine, or wrist is far greater than your chance of developing jaw necrosis. In fact, studies show that people who avoid these medications because of fear are more likely to end up in the hospital with a fracture.
But that doesn’t mean you ignore the risk. You manage it. Get your mouth checked before you start. Keep your teeth clean. Don’t skip dental visits. Tell your dentist you’re on a bisphosphonate. If you need surgery, don’t panic - talk to both your doctor and dentist. They can plan ahead.
And if you’ve been on the medication for years with no issues? Don’t stop. The drug stays in your bones for over a decade. Stopping now won’t suddenly make your jaw safe - but it will make your bones weak again.
What’s Changing Now?
New research is changing how we think about this. A 2024 study showed that stopping intravenous bisphosphonates for more than a year cuts MRONJ risk by 82%. But it also increases fracture risk by 28%. That’s a hard trade-off. Doctors are starting to use blood tests to measure bone turnover. If your levels are low, you might not need the drug anymore. If they’re high, you’re still at risk for fractures.
In the next few years, treatment will get more personalized. Not everyone needs 10 years of bisphosphonates. Some people get 3 to 5 years and stop. Others need more. The goal isn’t to avoid the drug - it’s to use it wisely.
Final Thought: Don’t Let Fear Stop You From Living
I’ve spoken to patients who turned down a root canal because they were scared of jaw necrosis. One woman canceled her denture fitting for two years. Another refused to have a tooth pulled - even though it was causing constant pain and infection. These are real consequences. The fear of a rare side effect can cost you your quality of life.
Bisphosphonates aren’t perfect. But they’ve kept millions of people upright, mobile, and independent. The risk of jaw necrosis is real - but it’s not common. And it’s preventable. Your best defense? A healthy mouth and open communication with your care team. Don’t let silence be your default. Ask questions. Get checked. Stay informed. Your bones - and your smile - will thank you.








Ellen Sales
November 25, 2025 AT 01:40Just read this and I’m crying-not because I’m scared, but because I finally feel seen. I’ve been on Fosamax for 8 years. Had a root canal last year. No issues. My dentist didn’t even blink when I told her I was on bisphosphonates. She just said, ‘Keep brushing, keep flossing, and don’t let fear make you sick.’ And she was right. I’m 71. I walk 3 miles every morning. My bones are stronger than my will to quit coffee. That’s the real win.
giselle kate
November 26, 2025 AT 13:08Typical Big Pharma propaganda. They want you scared of fractures so you’ll keep taking poison. Jaw necrosis isn’t rare-it’s covered up. Dentists are paid to look the other way. You think your doctor cares about you? They care about their bonus. Read the FDA’s internal memos. They knew. They always knew. Stop being a sheep.
Emily Craig
November 28, 2025 AT 05:42Okay but let’s be real-your jaw is the only bone that has to deal with bacteria, chewing, and your ex’s text messages. It’s under constant stress. So yeah, it’s the one that breaks down first. And if you’re skipping dental cleanings because you’re terrified of a 0.0007% chance? Honey, your anxiety is the real osteoporosis.
Karen Willie
November 30, 2025 AT 05:16I’m a nurse who’s seen a lot. I’ve had patients avoid bisphosphonates because of fear-and then break their hip on the way to the bathroom. I’ve also had patients with MRONJ who recovered because they caught it early. The key isn’t avoiding the drug. It’s staying connected-to your dentist, your doctor, and your own body. You’re not powerless. You’re just human. And humans need to talk.
Andrew Camacho
December 1, 2025 AT 01:12Oh wow. Another ‘trust your doctor’ sermon. Let me guess-you also think vaccines are fine and 5G isn’t spying on you? The FDA’s warnings are there for a reason. And if you’re telling people not to worry about jaw necrosis, you’re either paid by a pharma company or you’ve never held a dead piece of bone in your hand. I’ve seen it. It’s not a ‘rare side effect.’ It’s a slow-motion horror story. And you’re normalizing it.
Arup Kuri
December 2, 2025 AT 18:37US doctors sell poison to old people and call it medicine. In India we use turmeric and massage. No drugs. No necrosis. No lawsuits. You think your pills are helping? They’re just making your bones brittle and your jaw rot. The real cure is walking barefoot on grass and eating neem leaves. But you won’t do that because you’re too busy scrolling and trusting the system. Wake up.
Elise Lakey
December 4, 2025 AT 03:31I’ve been on Reclast for 4 years. My dentist said I’m a perfect candidate because I have no cavities, no gum disease, and I floss daily. She even called my oral hygiene ‘impeccable.’ I didn’t know that mattered. I thought the drug was the only thing. Turns out, my mouth is my first line of defense. I’m glad I listened.
Roscoe Howard
December 4, 2025 AT 16:28It is of paramount importance to acknowledge that the pharmacokinetic profile of bisphosphonates, particularly their affinity for hydroxyapatite, renders them disproportionately concentrated in high-turnover bone matrices-such as the mandible-thereby increasing susceptibility to osteonecrotic sequelae following iatrogenic or pathologic insult. Furthermore, the presence of oral microbiota introduces a pro-inflammatory milieu that synergistically exacerbates the anti-angiogenic effects of the medication. Ergo, a multidisciplinary pre-treatment dental evaluation is not merely advisable-it is a bioethical imperative.
Kimberley Chronicle
December 6, 2025 AT 09:30From a clinical pharmacology standpoint, the differential MRONJ incidence between oral and IV bisphosphonates is statistically significant (p < 0.001), with oral formulations demonstrating near-background risk in osteoporosis cohorts. The real clinical takeaway? Pre-treatment dental optimization reduces risk by >90%. It’s not about avoiding the drug-it’s about managing the microenvironment. We need more protocols, not more panic.
Shirou Spade
December 8, 2025 AT 04:17Every medicine has a shadow. The question isn’t whether the shadow exists-it’s whether we’re willing to live in the light anyway. I lost my aunt to a hip fracture. She refused bisphosphonates because she read about jaw necrosis on a blog. She spent her last year in a wheelchair, afraid to walk. I’d rather have a dead piece of jaw than a dead life.
Lisa Odence
December 8, 2025 AT 12:22OMG I just found out I’m on Fosamax and I’ve been skipping dentist visits for 3 years 😱😱😱 I’m literally gonna book an appointment right now 🙏🙏🙏 I didn’t know my mouth mattered so much 😭 I’m so sorry to my dentist 😭🙏 #BisphosphonateAwareness #DentalHealthIsBoneHealth
Pallab Dasgupta
December 9, 2025 AT 10:16I’m from India, been on Actonel for 5 years. My dentist here doesn’t even know what MRONJ is. I had to print out the FDA guidelines and show him. He laughed. Then he called his mentor. Now he checks my gums every visit. You think this is just an American problem? Nah. It’s global. But no one talks about it outside the US. That’s the real danger.
fiona collins
December 10, 2025 AT 08:00Shivam Goel
December 12, 2025 AT 01:30Let me break this down. You’re comparing a 0.0007% risk to a 20% fracture risk. That’s math. But you’re ignoring the psychological toll. People don’t die from jaw necrosis often-but they lose their dignity. They lose their ability to eat. To smile. To speak without shame. That’s not a side effect. That’s a tragedy disguised as a statistic. And you’re normalizing it by calling it rare. It’s not rare to the person living it.
Jefriady Dahri
December 12, 2025 AT 14:51My mom took Fosamax for 7 years. Never had a problem. But she went to the dentist every 6 months like clockwork. She told me, 'I don't trust my bones to a pill. I trust my mouth to a brush.' That stuck with me. I’m 32, no osteoporosis, but I floss daily. Because health isn’t about avoiding risks. It’s about building habits that outlive fear.