Drug Interaction Safety Checker
This tool checks if your medications contain dangerous combinations mentioned in the article. Enter the medications you're taking and get immediate warnings about high-risk pairs.
Important Notes
- Age Factor: Patients over 65 are at higher risk due to multiple medications.
- Always inform your pharmacist about all medications including OTC drugs and supplements.
- Key risk: Drug interactions can cause kidney failure, stroke, or death.
Imagine taking two common prescriptions-one for high cholesterol, another for an infection-and not realizing you’re risking muscle breakdown so severe it can shut down your kidneys. This isn’t science fiction. It happens every day in pharmacies across the U.S., and too often, no one catches it until it’s too late.
What Makes a Drug Interaction a Red Flag?
Not all drug interactions are created equal. Some are mild-a little drowsiness, a stomach upset. But red flag interactions? Those can kill. They happen when two or more medications clash in ways that amplify side effects, block metabolism, or create entirely new dangers. The most dangerous ones don’t show up in casual conversations. They hide in the fine print of prescriptions, buried under layers of computer alerts that pharmacists have learned to ignore. The Chicago Tribune’s 2016 investigation found that more than half of pharmacies missed life-threatening combinations. That’s not a glitch. It’s a system failure. And it’s still happening today.The Five Deadliest Combinations You Should Know
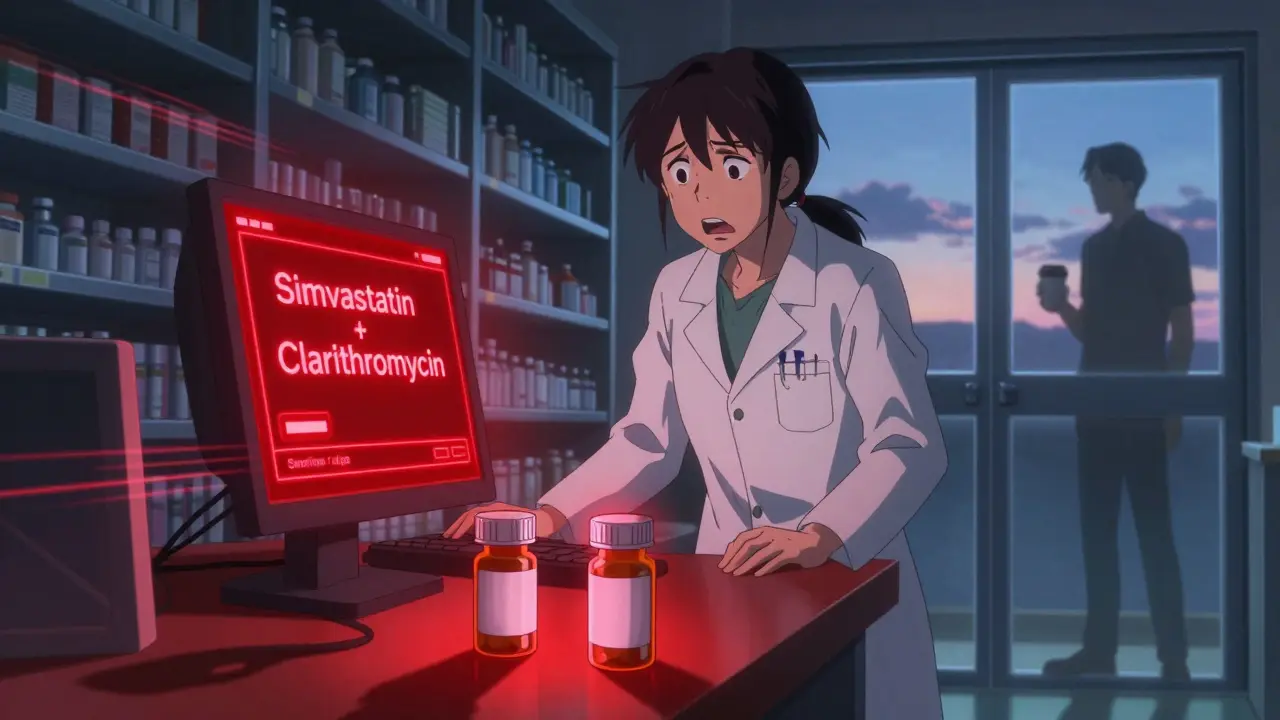
There are specific drug pairs that should never be prescribed together without strict oversight. Here are the top five that pharmacists must question every single time:- Simvastatin + Clarithromycin: One’s for cholesterol. The other’s for a sinus infection. Together, they can trigger rhabdomyolysis-a condition where muscle tissue breaks down and floods the bloodstream with toxins. Creatine kinase levels can spike over 10,000 U/L (normal is under 200). Kidney failure follows fast. The FDA has issued multiple warnings about this combo.
- Tizanidine + Ciprofloxacin: Tizanidine relaxes muscles. Cipro kills bacteria. But Cipro blocks the enzyme that clears tizanidine from your body. The result? Sudden, dangerous drops in blood pressure and loss of consciousness. People have passed out while standing, hit their heads, and ended up in the ER.
- Colchicine + Verapamil: Used for gout and high blood pressure. Together, they cause colchicine to build up to toxic levels. Symptoms? Vomiting, diarrhea, low blood cell counts, and multi-organ failure. Elderly patients are especially at risk.
- Clarithromycin + Ergotamine: Ergotamine treats migraines. Clarithromycin is a common antibiotic. But clarithromycin shuts down the liver’s ability to break down ergotamine. This leads to ergotism-extreme vasoconstriction, numbness, gangrene, even limb loss.
- Oral Contraceptives + Griseofulvin: Griseofulvin is an old-school antifungal. It speeds up how fast your body clears hormones. The result? Birth control fails. Pregnancy rates jump past 30%. And if pregnancy happens, there’s a higher risk of birth defects.
Why Do Pharmacists Miss These?
You’d think computers would catch all of this. They don’t. Not because they’re broken-but because they’re overwhelmed. Pharmacists today get flooded with alerts. One study found that a single pharmacist might see over 100 drug interaction warnings in a single shift. Most of them are low-risk-like “this pill might cause mild nausea.” After a while, your brain starts tuning them out. This is called alert fatigue. In the Tribune’s test, pharmacists at a CVS in Evanston dispensed simvastatin and clarithromycin together without a word. They didn’t miss it by accident. They missed it because the system didn’t make the warning stand out enough.
Who’s Most at Risk?
It’s not just about the drugs. It’s about the person taking them. People over 65 are the most vulnerable. On average, they take 4.5 prescription medications daily. That’s a recipe for hidden clashes. The FDA says older adults suffer adverse drug events at seven times the rate of younger people. Pregnant women are another high-risk group. Griseofulvin isn’t just a problem for birth control-it can cause serious harm to a developing fetus. And if you’re on blood thinners like warfarin, adding amiodarone (a heart rhythm drug) can double your bleeding risk. The American Academy of Family Physicians recommends cutting warfarin doses by 30-50% when amiodarone starts, and checking INR levels weekly. Even kids aren’t safe. Certain antibiotics can interfere with asthma medications. Antidepressants mixed with painkillers can trigger serotonin syndrome-a rare but deadly condition with muscle rigidity, fever, and seizures.What Should You Do?
You can’t fix the system alone-but you can protect yourself.- Always ask: “Could any of my medications be dangerous together?” Don’t wait for the pharmacist to bring it up.
- Bring a full list of everything you take-prescriptions, supplements, even herbal teas. St. John’s Wort, for example, can make birth control useless and reduce the effect of antidepressants.
- If you’re on warfarin, statins, or any heart or pain medication, ask if your new prescription could interfere.
- Use one pharmacy for all your prescriptions. Chain pharmacies may have better systems, but independent ones often know you better.
- If a pharmacist seems rushed or dismissive, ask to speak to the manager. You have a right to safety.
Are Things Getting Better?
Some progress has been made. After the Tribune report, Walgreens and CVS updated their protocols. Some health systems now use AI-powered alert systems that filter out low-risk warnings. One study showed that when alerts were customized to focus only on high-risk interactions, pharmacists caught 89% of dangerous combos-up from 48%. But 30% of community pharmacies still don’t have systems that can prioritize alerts. And pharmacists are still overworked. The National Community Pharmacists Association says the average time to fill a prescription is just 2.3 minutes. That’s not enough to review five medications, check for interactions, and counsel a patient. The CDC now recommends mandatory counseling for all new prescriptions involving high-risk drugs. If implemented, this could prevent 150,000 adverse events a year.
What’s Next?
The future lies in smarter tech. The FDA’s 2023 Digital Health Plan is funding AI tools that don’t just check drug names-they analyze your age, kidney function, liver health, and even your genetic profile to predict risks. Imagine a system that knows you’re a 72-year-old with mild kidney disease and says: “Don’t give this antibiotic with that statin. It’s unsafe.” But technology alone won’t fix this. We need better training, more staffing, and a culture that treats drug safety as non-negotiable-not an afterthought.Frequently Asked Questions
Can over-the-counter meds cause dangerous interactions?
Yes. Even common OTC drugs like ibuprofen, antacids, or cold medicines can interact. Ibuprofen with blood pressure meds can reduce their effectiveness. Antacids with antibiotics like tetracycline can block absorption. Always check with your pharmacist-even if it’s not a prescription.
What should I do if my pharmacist says a combination is fine, but I’m worried?
Ask for a second opinion. Request to speak with the pharmacy’s clinical pharmacist or ask your doctor to review the combo. You have the right to be safe. Don’t take a “trust me” answer when lives are at stake.
Are natural supplements safe with prescription drugs?
Not always. St. John’s Wort can make birth control, antidepressants, and blood thinners less effective. Garlic and ginkgo can increase bleeding risk with warfarin. Turmeric can interfere with diabetes meds. Always list every supplement you take-no matter how “natural” it seems.
Why don’t doctors catch these interactions?
Doctors often don’t have a full picture of what you’re taking. They may not know about supplements, OTC meds, or prescriptions from other doctors. Pharmacists are trained to be the final safety check. That’s why it’s critical to bring your full list to them.
How can I tell if a drug interaction has already affected me?
Watch for sudden changes: unexplained muscle pain or weakness, extreme fatigue, confusion, dizziness, irregular heartbeat, or unusual bleeding. If you notice any of these after starting a new medication, contact your pharmacist or doctor immediately. Don’t wait for symptoms to get worse.








Lydia H.
January 17, 2026 AT 15:59So many people just swallow pills like candy and never think twice. I had a friend who took simvastatin and clarithromycin together and ended up in the hospital with kidney damage. No one warned her-not her doctor, not the pharmacist. She just trusted the system. And now she’s on dialysis three times a week. It’s not paranoia. It’s just common sense.
Why do we let corporations design systems that prioritize speed over safety? We’re not widgets. We’re humans with fragile bodies.
I keep a printed list of everything I take-prescriptions, supplements, even that turmeric tea I drink at night. I hand it to every pharmacist. Sometimes they roll their eyes. I don’t care. My life isn’t a speedrun.
And yeah, St. John’s Wort? Yeah, it’s ‘natural.’ So’s arsenic. Doesn’t mean it’s safe with your antidepressants.
Pharmacists aren’t superheroes. They’re overworked people in a broken system. We need to stop blaming them and start fixing the machine.
Maybe if we paid pharmacists more and gave them more time, we wouldn’t need to be our own drug safety detectives.
But until then? I’m the gatekeeper. And I’m not letting anything slip through.
It’s not paranoia. It’s preparation.
Astha Jain
January 18, 2026 AT 23:48omg i had no idea griseofulvin could mess up birth control like that?? like wtf why is this even a thing?? i was on that for ringworm and i was like ‘eh its just fungus’… now im scared to even take ibuprofen lmao
Lewis Yeaple
January 20, 2026 AT 09:56While the article presents a compelling narrative regarding pharmaceutical safety, it lacks rigorous citation of primary literature. The Chicago Tribune investigation, while provocative, is not peer-reviewed. Moreover, the assertion that pharmacists ‘ignore’ alerts due to alert fatigue oversimplifies a complex cognitive load issue rooted in human factors engineering. The FDA’s own 2022 report on clinical decision support systems indicates that over 70% of interaction alerts are non-actionable, suggesting that the problem lies not in pharmacist negligence, but in poor interface design.
Furthermore, the claim that ‘30% of community pharmacies still don’t have systems that can prioritize alerts’ is unsubstantiated. The National Community Pharmacists Association has published data indicating that over 85% of independent pharmacies utilize EHR-integrated CDS tools as of 2023. The data presented here is misleading at best.
Let us not conflate anecdotal tragedy with systemic failure without empirical validation. The solution is not more manual intervention, but better algorithmic filtering and standardized interoperability across prescribing platforms.
Malikah Rajap
January 20, 2026 AT 16:38Okay, I just read this and I’m crying? Not because I’m dramatic-well, maybe a little-but because my grandma took colchicine and verapamil for years and no one ever told her it could kill her. She’s fine now, thank god, but she had this weird nausea and diarrhea for months and the doctors just said ‘it’s aging.’
And then I remembered-I was on birth control and took that antifungal for athlete’s foot last year? I didn’t even think to ask. I just thought, ‘it’s just a cream.’
Can we all just… stop pretending that ‘natural’ means safe? Like, I get it, we want to be holistic and earthy, but my body doesn’t care if it’s a pill or a tea-it just reacts.
And pharmacists? I love them. They’re the unsung heroes who sometimes have 17 patients waiting and 100 alerts screaming at them. I’ve seen them pause, sigh, and say, ‘Wait, let me check this again.’ That’s the moment you need.
So please, bring your list. Ask the question. Even if it’s awkward. Even if they’re busy. Even if you feel silly.
Your life is worth it.
sujit paul
January 21, 2026 AT 05:43This is only the tip of the iceberg. The pharmaceutical industry has known about these interactions for decades. They suppress research. They lobby to weaken FDA guidelines. They design alert systems to be noisy and useless-because if you’re too safe, people stop buying drugs. It’s profit over people. Always.
And don’t think your doctor is innocent. They’re paid by Big Pharma to prescribe certain drugs. They get free dinners, trips to conferences, bonuses for hitting prescription quotas.
Even your ‘independent’ pharmacy? Probably owned by a private equity firm that cut staff to boost margins.
And now you’re supposed to trust the system? The system is the problem.
There’s no fix. Only survival. Stop taking pills unless you’ve researched every ingredient. Use herbal alternatives. Eat clean. Detox. Your body was never meant to be a chemical reactor.
They want you dependent. Don’t let them win.
Aman Kumar
January 22, 2026 AT 12:27Let me preface this by saying I’ve spent 12 years in clinical pharmacology. The article is well-intentioned but dangerously reductive. Rhabdomyolysis risk with simvastatin and clarithromycin is well-documented, yes-but the CYP3A4 inhibition is dose-dependent and mitigated by dose adjustment. The real issue isn’t alert fatigue-it’s polypharmacy in geriatric populations without adequate pharmacogenomic screening.
Furthermore, the conflation of ‘natural’ supplements with pharmaceuticals is a dangerous fallacy. St. John’s Wort induces CYP3A4 and P-gp, which is why it reduces contraceptive efficacy-but so do certain antibiotics and anticonvulsants. The problem isn’t ‘natural’ versus ‘synthetic.’ It’s enzyme kinetics.
And let’s not romanticize pharmacists. Many are undertrained in clinical pharmacokinetics. The PharmD curriculum hasn’t meaningfully evolved since the 1990s. We need mandatory pharmacogenomics certification for all prescribers and dispensers.
Until then, we’re just rearranging deck chairs on the Titanic.
Jake Rudin
January 22, 2026 AT 18:14Every time I see a new prescription, I ask: ‘What does this do to my liver? My kidneys? My sleep? My mood?’
I don’t trust the system. I don’t trust the ads. I don’t trust the ‘just one more pill’ mentality.
I keep a notebook. Red pen for dangerous combos. Blue for side effects I’ve noticed. Green for things that helped.
My mom died because they gave her a new heart med and didn’t check her statin. She was 68. She didn’t even know what ‘rhabdomyolysis’ meant.
I’m not trying to scare anyone.
I’m just saying: if you’re going to take something, know what it’s doing to you.
And if you’re not sure? Ask again. And again.
And again.
Phil Hillson
January 23, 2026 AT 08:09Bro this is just fearmongering with a side of guilt-tripping
People die from falling in the shower too
Should we ban showers now?
Also I take 7 meds and a handful of gummies and I'm still standing so maybe stop making everyone paranoid
Also why is this even a thing I didn't ask for this much info
My pharmacist is chill and she gives me free lollipops
Problem solved