When your pharmacy hands you a pill that looks nothing like the one you’ve been taking for years, it’s normal to feel uneasy. The shape is different. The color’s off. The name on the tablet doesn’t match what your doctor wrote. You’re not alone. Millions of people in the UK and the US switch from brand-name drugs to generics every year - usually because it’s cheaper, sometimes because they’re told they have to. But what really happens when you make the switch? And should you be worried?
Generic drugs aren’t fake - they’re regulated
The first thing to know: generic drugs are not inferior copies. They’re not knock-offs. They’re not cheap imitations made in backrooms. In the UK and the US, they’re held to the same strict standards as brand-name drugs. The FDA and the MHRA require that generics contain the same active ingredient, in the same strength, and work the same way in your body. That means if you’re taking a generic version of metformin for diabetes, it’s doing exactly what the brand-name version does - lowering blood sugar.
The difference? Generics don’t have the fancy packaging, the marketing budget, or the patent protection. That’s why they cost 80% less on average. A 30-day supply of brand-name Lipitor might cost £120. The generic atorvastatin? Around £10. That’s not a trick. That’s how the system works. When a patent expires, other manufacturers can produce the same drug. The government doesn’t allow them to cut corners - they have to prove it works the same.
But why do some people feel worse after switching?
Here’s where things get messy. Some people swear their generic version doesn’t work as well. They report new side effects. Their seizures get worse. Their thyroid levels go haywire. Their blood thinners feel unpredictable. And in some cases, they’re right.
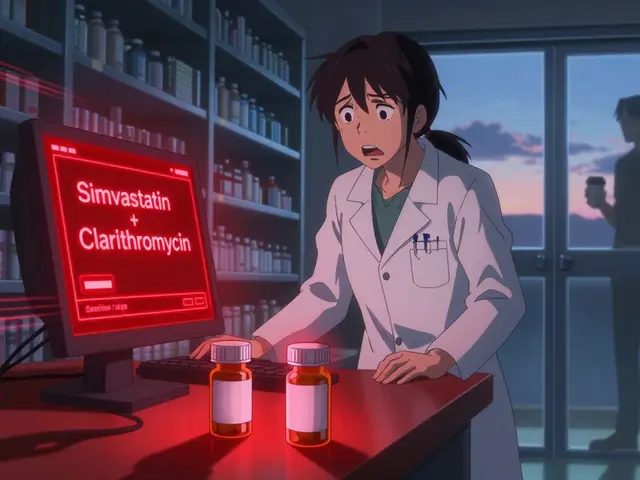
The issue isn’t the active ingredient. It’s the inactive stuff. Fillers. Dyes. Coatings. Binders. These don’t treat your condition, but they affect how the drug is absorbed. For most people, this doesn’t matter. But for drugs with a narrow therapeutic index - where the difference between a helpful dose and a harmful one is tiny - even small changes in absorption can cause problems.
That’s why switching is riskier with certain medications:
- Levothyroxine (for hypothyroidism): Tiny changes in absorption can throw off your TSH levels. One patient in the UK reported their TSH jumped from 2.5 to 8.7 after switching from Synthroid to generic.
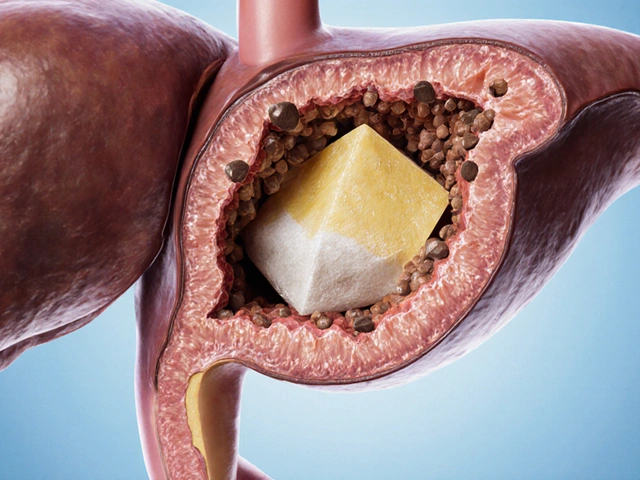
- Warfarin (a blood thinner): Small fluctuations can increase bleeding risk or cause clots.
- Anti-epileptic drugs: Multiple studies show higher seizure rates after switching generics. In one review, 1 in 5 patients had more seizures after the switch.
- Immunosuppressants (like cyclosporine): Critical for transplant patients. Even minor changes can lead to organ rejection.
These aren’t edge cases. They’re real, documented risks. That’s why doctors often write “dispense as written” on prescriptions for these drugs - meaning the pharmacist can’t swap it out without permission.
Why does the pill look different every time?
Have you ever filled a prescription and gotten a completely different-looking pill? One month it’s blue, the next it’s white. One time it’s round, the next it’s oval. That’s because pharmacies don’t always get the same generic manufacturer.
Generic drugs are made by dozens of companies - some in the UK, some in India, some in the US. When your pharmacy’s contract with one supplier ends, they switch to another. The active ingredient stays the same, but the fillers change. The shape changes. The imprint changes. To you, it looks like a different drug.
That’s confusing. And confusion leads to non-adherence. People think the new pill isn’t real. They skip doses. They panic. One study in Massachusetts found 63% of patients were initially worried about effectiveness after a switch - even though 82% were satisfied after three months.
Some pharmacies now label bottles with notes like “New manufacturer” or “Appearance changed.” That helps. But it’s not universal. If your pill looks different and you’re unsure, call your pharmacist. Don’t assume it’s wrong.
Cost savings are real - but so are hidden costs
Let’s talk money. Generic drugs save the NHS and private insurers billions every year. In the US, generics account for 90% of all prescriptions but only 20% of total drug spending. In the UK, similar savings are seen. For patients, that means lower copays. Many generics cost under £5 a month. Brand names? Often £50 or more.
But here’s the catch: if switching causes a bad reaction, you might end up in the ER, on more tests, or with a hospital stay. That’s not savings. That’s extra cost. One study found that while switching saved £100 on the drug, it led to £800 in additional care due to side effects.
And then there’s the cost of not taking your medicine. A 2019 report showed patients were 266% more likely to abandon a brand-name drug because of cost. Switching to a generic helped them stick with treatment. That’s a win. But if the generic makes them feel worse, they might stop anyway.
When switching works - and when it doesn’t
For most people, switching to generic drugs is safe and effective. If you’re taking a statin, an antibiotic, or a blood pressure pill, the odds are extremely high you won’t notice a difference. In fact, 78% of patient reviews on Drugs.com rated generic effectiveness as “good” or “excellent.”
But for others - especially those on narrow therapeutic index drugs - switching can be risky. The key is communication. Talk to your doctor before the switch. Ask:
- Is this drug one where small changes matter?
- Can I stay on the same generic manufacturer?
- Should I ask for “dispense as written” on my prescription?
Also, pay attention to how you feel after the switch. Keep a simple log: sleep, energy, mood, symptoms. If something changes - especially in the first 4-6 weeks - tell your doctor. Don’t wait. A simple blood test can check if your levels are still in range.

What to do if you’re worried
If you’re anxious about switching, here’s what you can do:
- Ask your pharmacist - “Is this the same generic I got last time?” If not, ask why it changed.
- Check your prescription - Does it say “dispense as written”? If not, you can ask your doctor to add it.
- Monitor your symptoms - Especially for thyroid, seizure, or blood-thinning meds. Write down changes.
- Don’t stop taking it - Even if you’re worried, don’t skip doses. Call your doctor instead.
- Know your rights - In the UK, pharmacists can switch generics unless your doctor says otherwise. But you can always request the brand if you feel it’s necessary.
Some patients do better on brand-name drugs. That’s okay. It’s not about being stubborn. It’s about finding what works for your body. If your doctor agrees, they can write a note to your pharmacy to keep you on the brand. Insurance might push back - but many will approve it if there’s documented clinical need.
Bottom line: It’s not all good or all bad
Generic drugs are not the enemy. They’re a vital tool that makes medicine affordable. For most people, they work just as well. But they’re not magic. They’re medicine - and like all medicine, they need to be used wisely.
Don’t assume all switches are safe. Don’t assume all generics are identical. Don’t assume your doctor knows every detail of your pharmacy’s supply chain. Be an informed patient. Ask questions. Track your response. Speak up if something feels off.
Medicine isn’t one-size-fits-all. Your body knows what works. Trust it - and back it up with facts.
Are generic drugs as effective as brand-name drugs?
Yes, for most medications, generics are just as effective. They contain the same active ingredient and must meet the same safety and strength standards as brand-name drugs. Regulatory agencies like the MHRA and FDA require proof of bioequivalence. However, for drugs with a narrow therapeutic index - like levothyroxine, warfarin, or anti-seizure meds - even small differences in absorption can matter. In these cases, some patients do better on the brand.
Why do generic pills look different?
Trademark laws prevent generic drugs from looking exactly like the brand-name version. So manufacturers change the color, shape, or size. They also use different inactive ingredients (fillers, dyes, coatings). This doesn’t affect how the drug works - but it can confuse patients. If your pill looks different, it doesn’t mean it’s wrong. Call your pharmacist to confirm it’s the same medication.
Can I ask my doctor to keep me on the brand-name drug?
Yes. If you’ve had a bad experience with a generic, or if you’re on a drug with a narrow therapeutic index, your doctor can write “dispense as written” or “no substitution” on your prescription. Insurance may require you to try the generic first, but if it causes problems, they usually approve the brand. Keep a record of any side effects or lab changes to support your request.
What should I do if I feel worse after switching?
Don’t stop taking the medication. Contact your doctor right away. Keep track of your symptoms - when they started, how severe they are, and whether they match any changes in your routine. For thyroid, seizure, or blood-thinning meds, your doctor may order a blood test to check your levels. Many times, switching back to the brand or staying on the same generic manufacturer resolves the issue.
Are there any risks with switching between different generic manufacturers?
Yes. Switching between different generic versions - even if both are approved - can cause problems for sensitive patients. Each manufacturer uses different fillers and manufacturing processes. For drugs like levothyroxine or warfarin, multiple switches can lead to unstable blood levels. Some experts recommend sticking with the same generic manufacturer whenever possible. Ask your pharmacist if you can get the same one each time.
If you’re switching drugs, remember: cost savings matter, but your health matters more. Stay informed. Stay alert. And never be afraid to speak up if something doesn’t feel right.





Destiny Annamaria
November 19, 2025 AT 11:05Okay but have y’all ever had your thyroid med switch from Synthroid to generic and suddenly feel like a zombie? I did. Took me 3 months to convince my doc to switch me back. Now I just pay out of pocket because my life’s not a spreadsheet.
Ron and Gill Day
November 19, 2025 AT 18:12Ugh. Another ‘generic drugs are fine’ lecture. Newsflash: if you’re not on a narrow therapeutic index drug, you’re not the patient who gets screwed. The FDA’s standards are a joke. I’ve seen generics with 20% variation in absorption. That’s not bioequivalent - that’s gambling with your life.
Alyssa Torres
November 21, 2025 AT 00:45Y’all need to hear this: I’m a nurse and I’ve watched patients crash because they thought a different-looking pill meant it wasn’t real. One lady stopped her warfarin for a week after her generic changed color - ended up with a pulmonary embolism. Please don’t assume. Talk to your pharmacist. Write down how you feel. Your body isn’t lying. And if you’re scared? You’re not being dramatic - you’re being smart.
Summer Joy
November 21, 2025 AT 19:23So let me get this straight - you’re telling me I can’t trust my meds because some Indian factory made them with a different dye?? 😭 I’m not taking my anxiety pills if they look like a rainbow gummy bear. This is why I pay extra. My mental health is not a cost-cutting experiment.
Aruna Urban Planner
November 22, 2025 AT 11:27The pharmacokinetic variability across generic manufacturers is statistically significant for drugs with a narrow therapeutic index. While regulatory equivalence is mandated, inter-manufacturer bioequivalence is not systematically monitored post-market. This creates a latent risk for polypharmacy patients, particularly those on anticoagulants or antiepileptics. Consistency in sourcing is clinically prudent.
Nicole Ziegler
November 24, 2025 AT 04:46My pill changed color again 😐 but I just took it. If it’s the same active ingredient, it’s fine. 🤷♀️ #genericlife #dontpanic
Bharat Alasandi
November 24, 2025 AT 13:00Bro in India we switch generics every month and no one dies. The real issue is when doctors don’t tell you to monitor your levels. It’s not the pill - it’s the lack of follow-up. Get your TSH checked. Check INR. That’s the fix, not the brand name.
Kristi Bennardo
November 25, 2025 AT 00:45This article is dangerously misleading. It normalizes a system that puts patients at risk for financial convenience. The FDA allows generics to vary by up to 20% in absorption - that’s not ‘equivalent,’ that’s negligence. I’ve lost patients to seizures because of this. This isn’t ‘informative’ - it’s corporate propaganda.
Shiv Karan Singh
November 25, 2025 AT 22:34Everyone’s freaking out about generics? Bro, brand-name drugs are just expensive placebos with better ads. The ‘narrow therapeutic index’ argument is just fearmongering. If your body can’t handle a little variation, maybe you’re the problem.
King Over
November 26, 2025 AT 09:55My pill changed again. Took it anyway. Still alive
Johannah Lavin
November 28, 2025 AT 04:27To the person who said their TSH jumped after switching - I feel you. I had the same thing. I started a little notebook: date, pill color, how I felt, sleep, energy. It helped me prove to my doctor it wasn’t ‘in my head.’ Now I get my brand. And guess what? I’m not broke - I’m alive. Your health is worth fighting for 💪❤️
Ravinder Singh
November 30, 2025 AT 04:08Here’s the truth: generics are the backbone of global access to medicine. But the system is broken when switching happens without patient consent or monitoring. The solution isn’t to reject generics - it’s to demand traceability. Pharmacies should label the manufacturer. Doctors should track outcomes. Patients should have a say. We can have affordability AND safety - it just takes accountability.
Russ Bergeman
December 1, 2025 AT 23:04Wait… so you’re saying that if I’m on warfarin, I should pay $120 for a pill that’s chemically identical to a $10 one? That’s not healthcare - that’s extortion. And if you’re having side effects? Maybe you’re just not compliant. Or maybe you’re overreacting. Get a lab test. Stop blaming the pill.