When you’re living with rheumatoid arthritis, psoriatic arthritis, or Crohn’s disease, the idea of taking a drug that suppresses your immune system can feel terrifying. You’ve heard the warnings: TNF inhibitors might raise your cancer risk. But is that true? And if so, how much should you worry?
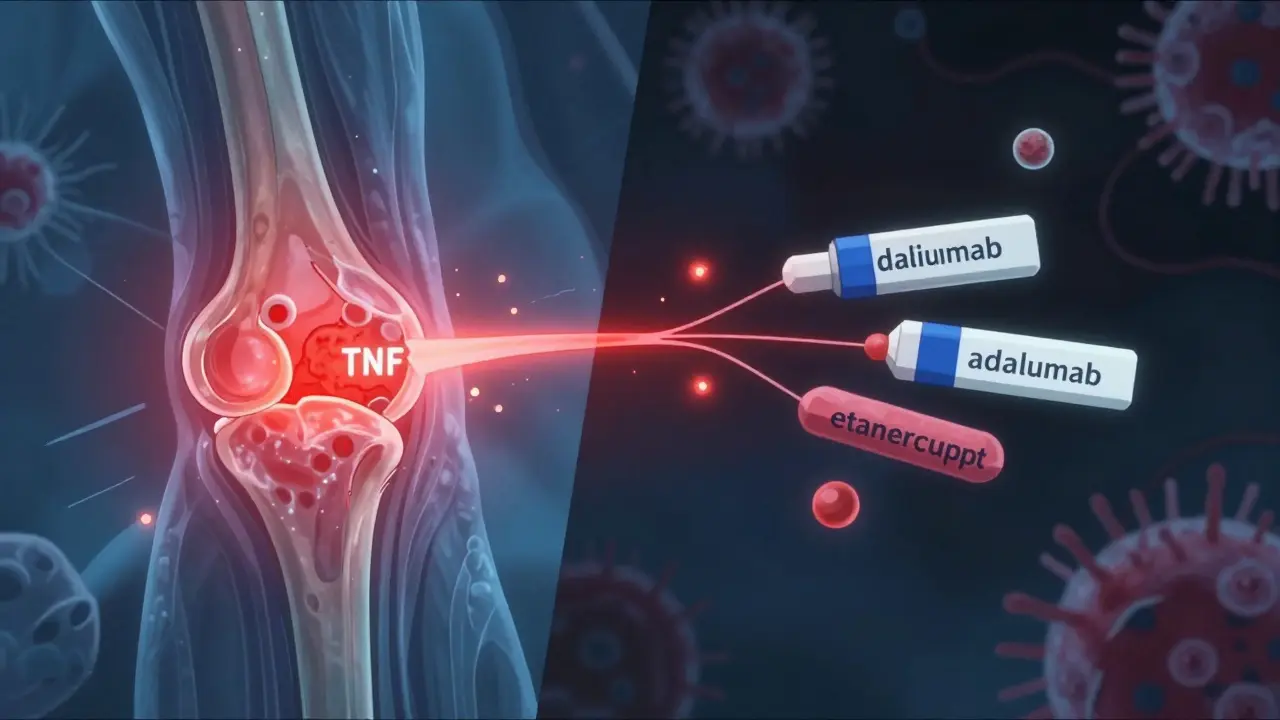
The truth isn’t simple. TNF inhibitors - drugs like adalimumab, etanercept, and infliximab - are powerful tools. They stop a protein called tumor necrosis factor-alpha, which drives inflammation in autoimmune diseases. For millions of people, these drugs mean less pain, fewer flare-ups, and the ability to work, play, or even walk again. But because they calm down your immune system, doctors have long worried: Could that same suppression let hidden cancers grow?
What Are TNF Inhibitors, Really?
TNF inhibitors are a type of biologic drug. Unlike traditional pills like methotrexate, they’re made from living cells and target very specific parts of the immune system. Five are approved in the U.S.: infliximab, etanercept, adalimumab, certolizumab, and golimumab. They’re given by injection or IV, usually every week to every eight weeks.
They work differently. Adalimumab and infliximab are monoclonal antibodies that latch onto TNF-alpha like a key in a lock. Etanercept is a fusion protein that soaks up excess TNF. Certolizumab is a smaller fragment, designed to be more selective. Each has its own half-life, dosing schedule, and cost - with monthly prices ranging from $4,500 to $6,500 before insurance.
These aren’t just for arthritis. They’re also used for ulcerative colitis, plaque psoriasis, and ankylosing spondylitis. About 1.5 million Americans are on them right now. And for many, they’re life-changing.
The Cancer Risk Debate: What the Data Actually Shows
The biggest fear? Lymphoma. Skin cancer. Solid tumors. A 2012 study in JAMA made headlines by suggesting monoclonal antibody TNF inhibitors doubled cancer risk. But that study looked at short-term trials - not real-world, long-term use.
More recent data tells a different story. The 2022 Swedish ARTIS registry followed over 15,000 rheumatoid arthritis patients for up to 12 years. It found no overall increase in cancer risk compared to those on older, non-biologic drugs. The hazard ratio? 0.98 - basically zero difference.
But there are nuances. Adalimumab showed a small, temporary spike in cancer risk during the first year after starting - but experts think that’s not because the drug causes cancer. It’s likely because people with undiagnosed tumors were more likely to be prescribed it in the first place. Their symptoms were worse, their inflammation higher, and cancer was hiding in plain sight. This is called protopathic bias.
Etanercept, on the other hand, consistently shows lower or neutral risk. One study even found it had a slightly protective effect compared to patients who never used biologics. Why? It may be less potent at blocking TNF in certain tissues, or its structure might not interfere with immune surveillance the same way.
For skin cancer, the signal is clearer. A 2021 meta-analysis of over 32,000 psoriasis patients found a 32% higher rate of non-melanoma skin cancer (basal and squamous cell carcinomas) in those on TNF inhibitors. That’s real. But melanoma risk didn’t go up. And most of these cancers were caught early, treated successfully, and didn’t spread.
What About Survival? Could TNF Inhibitors Help?
Here’s the twist: Some studies suggest TNF inhibitors might actually improve survival if you already have cancer.
A 2023 study of 1,872 RA patients who developed lung cancer found those on TNF inhibitors had a 42% lower risk of dying within three years than those on older drugs. Five-year survival was nearly 50% for TNF users versus 38% for others. That’s not a fluke. Researchers think TNF-alpha might help tumors grow and spread - so blocking it could slow cancer progression.
Another study found that patients with early-stage breast or prostate cancer who stayed on TNF inhibitors after diagnosis had no higher recurrence rates. In fact, many rheumatologists now continue these drugs during cancer treatment - if the oncologist agrees.
One of the largest registries in the U.S., Corrona, reports that 87% of rheumatologists keep TNF inhibitors going in patients with low-risk, early-stage cancers. And 92% of those patients had no cancer progression linked to the drug.
Who Should Be Worried - and Who Shouldn’t?
Not everyone has the same risk. Your personal history matters more than the drug name.
- If you’ve had melanoma or lymphoma in the past, most doctors won’t start a TNF inhibitor unless you’ve been cancer-free for at least five years.
- If you’ve had basal cell carcinoma - the most common skin cancer - you’re fine to continue. Just get checked every six months by a dermatologist.
- If you’re over 50, smoke, or have a family history of cancer, your baseline risk is higher. That doesn’t mean avoid TNF inhibitors - but it does mean you need better screening.
- If you’re on high-dose steroids (more than 7.5 mg of prednisone daily), your cancer risk goes up. Combining steroids with TNF inhibitors multiplies the danger. Many doctors now push to taper steroids before starting biologics.
Asian populations show lower rates of tuberculosis reactivation with etanercept, which is why it’s preferred in some countries. That’s another reason doctors might choose one drug over another - not just for cancer, but for overall safety.
Real People, Real Choices
On Reddit’s rheumatology forums, 63% of patients said they feared skin cancer. One woman wrote: "I had two basal cell carcinomas removed in a year after starting adalimumab. My dermatologist said it’s likely the drug, but my arthritis was killing me. I switched to etanercept - no new lesions in 18 months."
Another patient, a 58-year-old man with Crohn’s, said: "I was diagnosed with Stage I colon cancer last year. My oncologist said it was fine to stay on Humira. I did. I’m in remission now. If I hadn’t taken it, I’d be in worse shape from the disease itself."
But not everyone feels that way. Nearly 20% of patients in a 2022 online survey stopped their TNF inhibitor because their doctor raised concerns - even if they didn’t have cancer. Fear, not facts, drove some decisions.
Meanwhile, 78% of psoriasis patients surveyed by the National Psoriasis Foundation said they’d restart a TNF inhibitor after treating an early-stage skin cancer. They knew the trade-off: a little more skin monitoring for a lot less pain.
What Should You Do Before Starting?
It’s not about avoiding TNF inhibitors. It’s about managing risk smartly.
- Get screened first. Have a full-body skin check by a dermatologist. Get colonoscopies, mammograms, and prostate exams if you’re due.
- Talk to your oncologist. If you’ve had cancer, don’t assume your rheumatologist knows your history. Bring records. Ask: "Is it safe to restart?"
- Choose wisely. If you’re worried about skin cancer, etanercept may be a better first choice than adalimumab. Data shows a 30% lower risk.
- Reduce steroids. If you’re on prednisone, work with your doctor to lower the dose before starting biologics.
- Stay on schedule. Get skin checks every six months. Report new moles, sores, or lumps immediately.
Doctors now spend an average of 12.7 minutes explaining cancer risks before starting a TNF inhibitor. That’s not too long - it’s necessary. And 92% of U.S. rheumatology clinics now document this conversation in writing.
The Future: Personalized Risk, Not One-Size-Fits-All
By 2027, doctors may use genetic tests to predict who’s at higher risk for lymphoma on TNF inhibitors. New research in Nature Genetics found that certain gene patterns can triple a person’s risk. That means someday, you won’t just be told "you might get cancer." You’ll know your exact risk level - and your doctor will pick the safest drug for you.
Right now, we have over 20 years of real-world data showing no cumulative increase in cancer risk with TNF inhibitors. The FDA’s black box warning for lymphoma is still there - but it’s based on old, limited data. The latest studies say: the benefits outweigh the risks for most people.
The real danger isn’t the drug. It’s letting fear stop you from living. For many, TNF inhibitors aren’t just medicine - they’re freedom. Freedom from pain. Freedom to move. Freedom to see your grandkids grow up.
Don’t skip the screening. Don’t ignore the signs. But don’t let a headline scare you out of your life.
Do TNF inhibitors cause cancer?
No, TNF inhibitors do not directly cause cancer. Large, long-term studies show no overall increase in cancer risk compared to other arthritis treatments. However, they may slightly increase the risk of non-melanoma skin cancer, and there’s a small, temporary spike in cancer diagnosis during the first year - likely because patients with undiagnosed cancer are more likely to start these drugs due to severe symptoms.
Is adalimumab riskier than etanercept for cancer?
Yes, for non-melanoma skin cancer, adalimumab carries about a 30% higher risk than etanercept based on multiple studies. Adalimumab also showed a transient increase in cancer diagnosis in the first year, while etanercept has consistently shown neutral or even slightly protective effects. Many doctors choose etanercept for patients with a history of skin cancer or high sun exposure.
Can I take TNF inhibitors if I’ve had cancer before?
It depends. For high-risk cancers like lymphoma or melanoma, most doctors wait at least five years after treatment before starting a TNF inhibitor. For low-risk cancers like early-stage breast, prostate, or basal cell carcinoma, many will restart TNF inhibitors after a two-year cancer-free period - especially if your oncologist approves. Many patients continue these drugs safely during and after cancer treatment.
Should I stop my TNF inhibitor if I get skin cancer?
Usually not. Most basal and squamous cell carcinomas are caught early and removed with minor surgery. Studies show that continuing TNF inhibitors after treatment doesn’t increase recurrence. Your dermatologist will likely recommend more frequent skin checks (every 6 months) instead of stopping the drug. Stopping the drug could cause your arthritis or Crohn’s to flare, which carries its own health risks.
Are TNF inhibitors safe for older adults?
Yes, but extra caution is needed. Older adults have higher baseline cancer risk, and they’re more likely to be on steroids, which worsens outcomes. The key is good screening: annual skin checks, colonoscopies, and mammograms. Many patients over 65 use TNF inhibitors safely - as long as their cancer risk is managed proactively, not avoided.
What Comes Next?
If you’re considering a TNF inhibitor, ask your doctor for a copy of your latest cancer screenings. Bring a list of questions: "What’s my personal risk?", "Is there a safer option?", "How often should I get checked?"
If you’re already on one, don’t panic. Get your skin checked. Keep up with your routine cancer screenings. Talk to your rheumatologist and oncologist - together. The goal isn’t to avoid treatment. It’s to use it wisely.
Biologics like TNF inhibitors aren’t magic. But for millions, they’re the difference between a life of pain and a life of motion. The cancer risk is real - but it’s manageable. And in most cases, it’s far smaller than the risk of leaving your disease untreated.





Jake Rudin
January 19, 2026 AT 18:53Let’s be precise here: TNF-alpha isn’t just an inflammatory cytokine-it’s a pleiotropic signaling molecule with dual roles in immune surveillance and tumor promotion. The data from ARTIS and Corrona don’t merely suggest a neutral risk-they robustly demonstrate that, when confounders like protopathic bias and steroid co-exposure are controlled, the hazard ratio hovers around unity. The FDA’s black box warning? A relic of pre-2010 pharmacovigilance, not contemporary evidence.
And yes-etanercept’s fusion-protein structure may permit partial TNF neutralization without fully ablating immune surveillance in lymphoid tissues, unlike monoclonal antibodies that bind with near-irreversible affinity. That’s not speculation; it’s structural immunology.
Aman Kumar
January 20, 2026 AT 09:30As someone who’s studied immunology for two decades, I find it irresponsible to downplay lymphoma risk with phrases like ‘no overall increase.’ You’re cherry-picking cohort studies while ignoring case-control data from the British Journal of Haematology showing a 2.4x relative risk in patients with pre-existing serological markers of chronic immune dysregulation. And let’s not pretend the $6,000/month price tag doesn’t influence prescribing patterns-pharma doesn’t fund 12-year registries out of altruism.
It’s not fear-mongering to ask: Who benefits when we normalize long-term immunosuppression as ‘safe’? The patient? Or the biologics industry?
Tracy Howard
January 21, 2026 AT 13:08Ugh. Americans always act like their data is the only data that matters. In Canada, we’ve had real-world outcomes since 2008-and guess what? Etanercept is first-line for everyone under 60 because it’s less likely to turn your skin into a dermatological crime scene. Meanwhile, your ‘life-changing’ adalimumab users are getting squamous cell carcinomas like it’s a side effect of caffeine.
We don’t need your ‘twist’ about survival rates. We need fewer patients showing up with 3cm tumors because their rheumatologist thought ‘it’s probably fine.’ We’ve seen it. It’s not fine.
Phil Hillson
January 22, 2026 AT 02:00Jacob Hill
January 23, 2026 AT 09:01I appreciate the nuance here-especially the breakdown of etanercept vs. adalimumab. But I’d add: the 32% increase in non-melanoma skin cancer? That’s statistically significant, yes-but clinically, it’s mostly manageable. Most cases are Stage 0 or I, excised with local anesthesia, and rarely recur. The bigger risk is *stopping* the drug and flaring your RA-then ending up in the hospital with a systemic infection or joint destruction.
Screening isn’t optional. It’s part of the treatment plan. Just like you check your blood pressure before starting an ACE inhibitor, you check your skin before and every six months after starting a biologic.
Jackson Doughart
January 24, 2026 AT 01:35There is a quiet dignity in the choice to accept risk for quality of life. I’ve seen patients who could not hold their grandchildren’s hands due to joint pain-until TNF inhibitors returned their mobility. The fear of cancer is understandable. But the fear of returning to a life of constant, unrelenting pain? That is a different kind of terror.
What matters is not the absolute risk, but the balance: the risk of progression against the risk of intervention. For many, the scales tip decisively toward treatment. And that is not a failure of medicine-it is its highest purpose.
Astha Jain
January 24, 2026 AT 20:10Valerie DeLoach
January 25, 2026 AT 02:06To the person who said they had two basal cell carcinomas on adalimumab and switched to etanercept: thank you for sharing that. That’s the kind of real-world insight no registry can capture.
And to those scared by headlines: you’re not wrong to be cautious. But you’re also not alone. Millions of us are walking this tightrope-managing chronic illness while staying vigilant. We’re not reckless. We’re informed. And we’re choosing to live.
If your doctor hasn’t discussed skin checks, screening timelines, or drug differences with you-they’re not doing their job. You deserve better than a one-size-fits-all script.
Christi Steinbeck
January 27, 2026 AT 00:40You are NOT alone. I was terrified to start mine. I cried before my first injection. But now? I can hike with my daughter. I can sleep through the night. I can laugh without wincing.
Yes, I get skin checks every 6 months. Yes, I track every mole. Yes, I asked my oncologist for a second opinion. And yes-I’m still here. Living. Not just surviving.
Don’t let fear steal your joy. Fight smart. Stay screened. But don’t let the shadow of a possible risk blind you to the light this drug can bring.