Potassium Level Estimator for Irbesartan/HCTZ
Predict Your Potassium Level
Estimate how Irbesartan/HCTZ might affect your potassium after 3 months
Estimated Potassium Level
Enter your details to see prediction
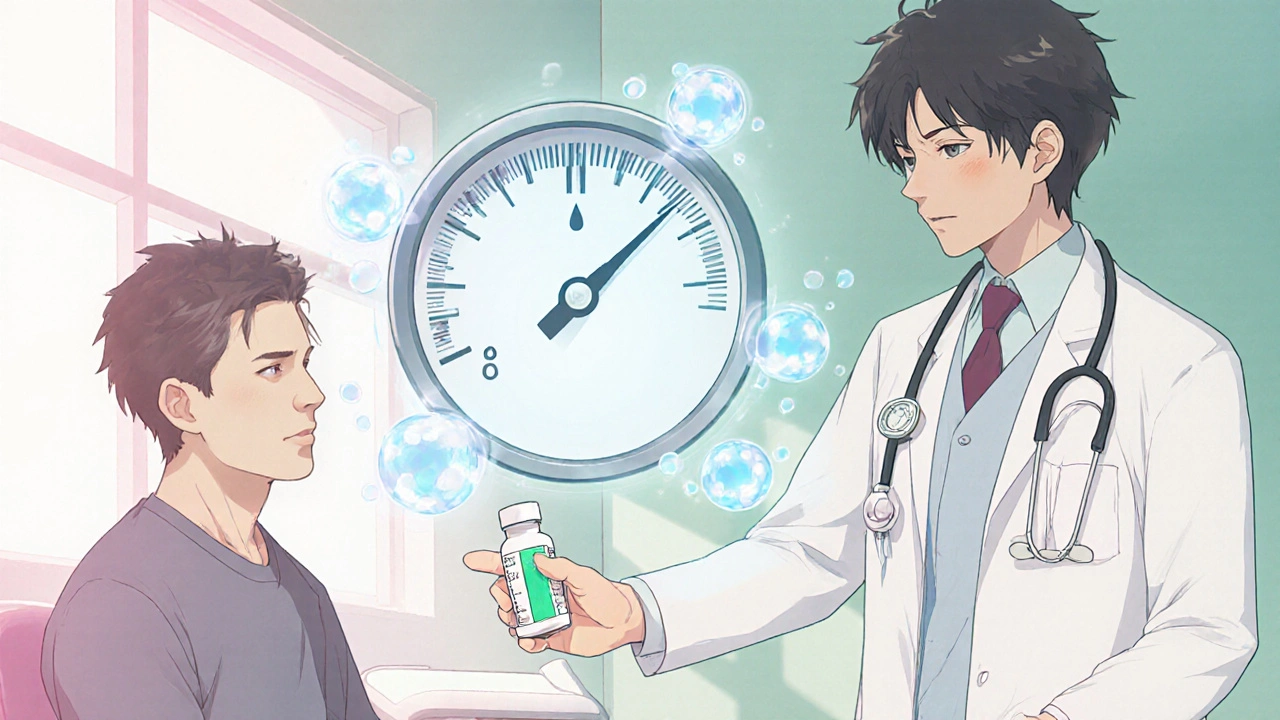
When doctors prescribe a pill that combines Irbesartan Hydrochlorothiazide (an ARB paired with a thiazide diuretic), they’re trying to hit two goals at once: lower blood pressure and reduce fluid buildup. That clever duo works well for many, but it also nudges the body’s potassium balance in ways that can be easy to miss. Understanding how the combo affects potassium helps patients and clinicians catch problems before they turn serious.
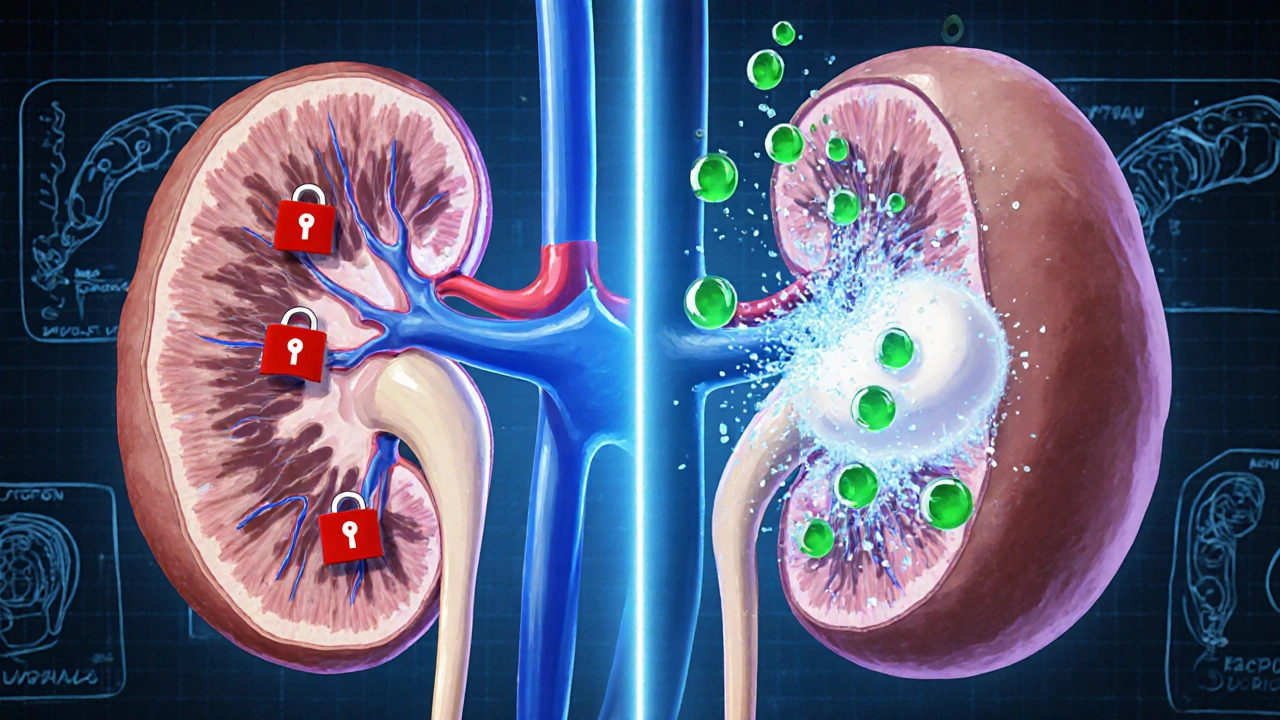
How the Two Compounds Work Together
Irbesartan belongs to the angiotensin‑II receptor blocker (ARB) family. By blocking the Renin‑Angiotensin System a hormone cascade that tightens blood vessels, it relaxes arteries and lowers pressure without the cough that ACE inhibitors often cause.
Hydrochlorothiazide, on the other hand, is a thiazide diuretic. It tells the kidneys to let more sodium and water leave the body through urine, which drops volume and pressure. The trade‑off is that thiazides can push potassium out of the bloodstream, leading to lower serum levels.
When paired, irbesartan’s tendency to keep potassium in check can offset the diuretic’s potassium‑wasting effect, creating a more balanced electrolyte profile for many patients. But the balance isn’t perfect, and several factors tilt it either way.
Why Potassium Matters
Potassium (K the main intracellular cation) is essential for nerve signaling, muscle contraction, and heart rhythm. Normal serum potassium sits between 3.5 and 5.0 mmol/L. Drop below 3.5 mmol/L (hypokalemia) and you risk muscle weakness, arrhythmias, and, in extreme cases, cardiac arrest. Push above 5.5 mmol/L (hyperkalaemia) and the heart can also go into dangerous rhythms.
Because blood pressure meds sit right in the kidney’s filtration system, they are among the most common culprits for electrolyte swings. Monitoring potassium becomes a routine part of managing patients on Irbesartan Hydrochlorothiazide.
Factors That Shift Potassium Levels
- Kidney function: Reduced glomerular filtration rate (GFR) hampers the kidney’s ability to excrete excess potassium, raising the risk of hyperkalaemia.
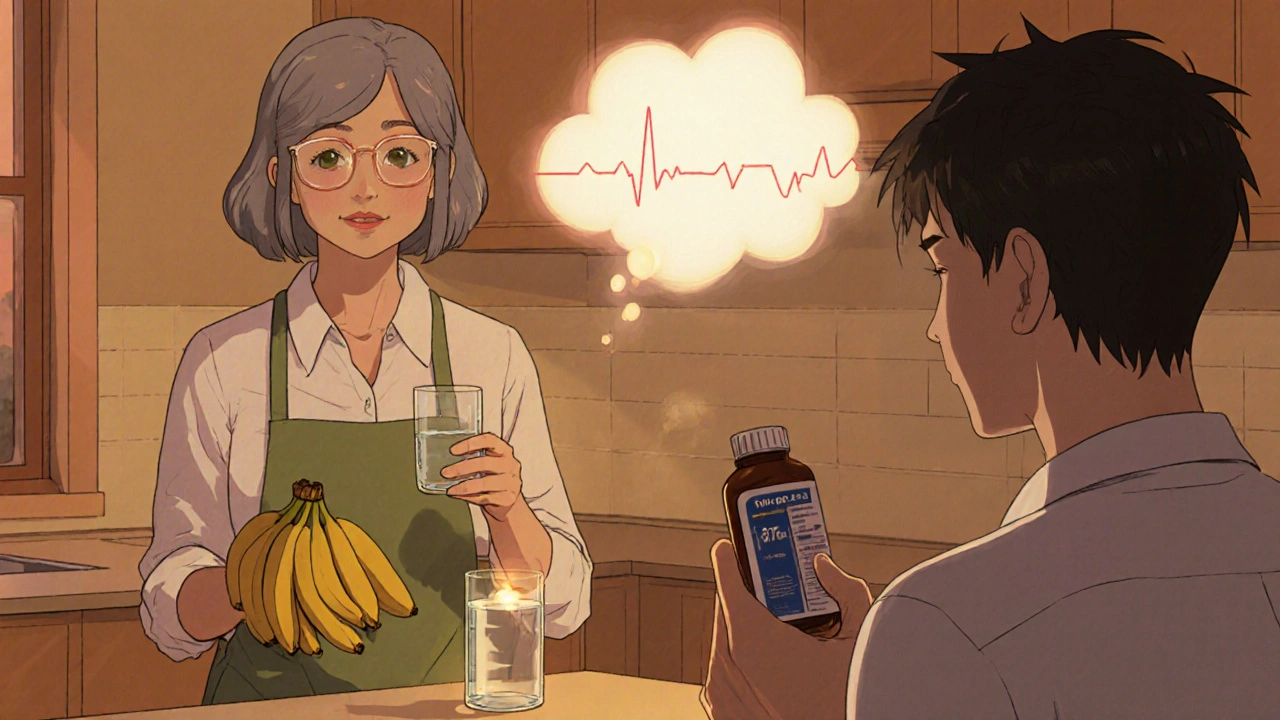
- Diet: High‑potassium foods (bananas, potatoes, oranges) can push levels up, while low‑potassium diets (often advised for CKD) can accentuate hypokalemia.
- Other medications: NSAIDs, potassium‑sparing diuretics, or ACE inhibitors added on top of the combo can stack potassium‑raising effects.
- Dosage: Higher doses of hydrochlorothiazide (e.g., 25 mg) tend to cause more urinary potassium loss than lower doses (12.5 mg).
- Comorbidities: Conditions like diabetes, chronic kidney disease, or heart failure each bring their own electrolyte quirks.
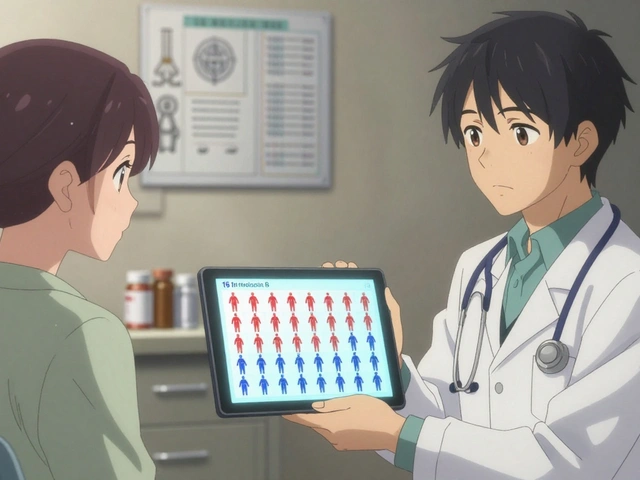
Typical Potassium Changes Observed in Clinical Practice
Large‑scale studies of the Irbesartan/HCTZ combo (often marketed under names like Co‑Aprovel) show a modest average drop of about 0.2 mmol/L in serum potassium after three months of therapy. However, the spread is wide:
| Regimen | Average Potassium Change (mmol/L) | Incidence of Hypokalemia (<3.5) | Incidence of Hyperkalaemia (>5.5) |
|---|---|---|---|
| Irbesartan alone | +0.1 | 2 % | 1 % |
| Hydrochlorothiazide alone | -0.4 | 8 % | 0 % |
| Irbesartan + Hydrochlorothiazide | -0.2 | 5 % | 2 % |
| Losartan + Hydrochlorothiazide | -0.15 | 4 % | 3 % |
The table shows that adding irbesartan tempers the potassium‑loss effect of hydrochlorothiazide, but the net change still leans negative for many patients. Those with borderline low potassium at baseline should be watched closely.
Monitoring Recommendations
- Check serum potassium and creatinine before starting therapy.
- Repeat labs after 2 weeks, then at 1‑month, and every 3‑6 months thereafter.
- If potassium falls below 3.5 mmol/L, consider dose reduction, adding a potassium‑rich diet, or prescribing a potassium supplement.
- If potassium climbs above 5.5 mmol/L, pause the thiazide component, reduce the irbesartan dose, or switch to an ARB without a diuretic.
- Always reassess after any change in concomitant meds, especially NSAIDs or potassium‑sparing agents.
These steps reflect guidance from the European Society of Cardiology and UK NICE recommendations for ARB‑diuretic combos.
Real‑World Patient Stories
Emma, 62, hypertension & chronic kidney disease stage 3: After three months on Irbesartan 12.5 mg/HCTZ 12.5 mg, her labs showed potassium 3.3 mmol/L. Her doctor added a low‑dose potassium chloride supplement and advised a banana‑rich snack. Six weeks later, potassium steadied at 4.0 mmol/L and blood pressure improved.
James, 55, type 2 diabetes: He started the same combo but also took ibuprofen daily for back pain. His potassium spiked to 5.8 mmol/L, prompting the clinician to switch the diuretic to a lower‑dose thiazide and to replace ibuprofen with acetaminophen. Potassium normalized within a month.
Both cases illustrate how lifestyle, kidney health, and other drugs swing the potassium needle.
When to Consider Alternatives
If a patient repeatedly swings outside the safe potassium window, look at other options:
- ARB alone: Irbesartan monotherapy avoids diuretic‑related potassium loss but may need an additional antihypertensive (e.g., calcium‑channel blocker).
- ACE inhibitor + thiazide: Similar blood‑pressure effect but carries a cough risk.
- Calcium‑channel blocker + thiazide: No direct potassium‑retaining effect, so monitor more closely.
- SGLT2 inhibitor: For patients with diabetes, this class lowers BP and can improve kidney outcomes while modestly raising potassium.
Choosing hinges on the patient’s overall risk profile, comorbidities, and tolerance.
Key Takeaways
- Irbesartan Hydrochlorothiazide lowers blood pressure but can push potassium down slightly.
- Kidney function, diet, other meds, and dose level are the biggest modifiers.
- Regular lab checks-baseline, 2 weeks, then every 3‑6 months-catch problems early.
- Adjust dose, add supplements, or switch drugs if potassium drifts outside 3.5‑5.5 mmol/L.
- Patient education on diet and over‑the‑counter meds is essential.
Frequently Asked Questions
Can Irbesartan Hydrochlorothiazide cause high potassium?
Yes, especially in people with reduced kidney function or when combined with other potassium‑raising drugs. If serum potassium exceeds 5.5 mmol/L, doctors usually lower the dose or pause the thiazide component.
What foods should I avoid to keep potassium stable?
If you’re prone to low potassium, add bananas, oranges, potatoes, and leafy greens. If you risk high potassium, limit those foods and focus on apples, berries, and white rice.
How often should I have blood tests while on this medication?
Check electrolytes and kidney labs before starting, then after 2 weeks, at 1 month, and every 3‑6 months thereafter. More frequent testing is needed after any dose change or if you add new meds.
Is it safe to take ibuprofen with Irbesartan Hydrochlorothiazide?
Occasional ibuprofen can be okay, but regular use may raise potassium and stress the kidneys. Talk to your clinician about safer pain relievers like paracetamol.
What should I do if I feel muscle weakness?
Muscle weakness can signal low potassium. Get a quick blood test; if levels are low, your doctor may add a supplement or adjust the diuretic dose.






Rajesh Singh
October 18, 2025 AT 19:07When patients ignore the subtle tug that potassium levels give, they gamble with their own heartbeats.
A careless sip of diuretic without a concomitant potassium check is nothing short of negligence.
The Irbesartan‑HCTZ duo, while clever, is a double‑edged sword that demands respect.
Kidney function is the gatekeeper; if it falters, potassium can surge like an unchecked river.
Conversely, a high‑dose thiazide can strip potassium faster than a desert wind erodes sand.
Dietary choices are not mere preferences; they are medical interventions that tilt the electrolyte scale.
Bananas and oranges can rescue a low potassium portrait, but the same foods can poison a patient already flirting with hyperkalaemia.
Over‑the‑counter NSAIDs add another layer of risk, sneaking potassium spikes into an already fragile system.
Regular labs are the only compass to navigate this volatile terrain, and skipping them is akin to sailing blind.
Two‑week checks after initiation, followed by quarterly reviews, form the backbone of safe stewardship.
If a readout shows 3.3 mmol/L, a modest potassium supplement and a banana‑rich snack can restore balance without upheaval.
Should the number creep above 5.5 mmol/L, the clinician must consider pausing the thiazide or dialing back the ARB.
Patient education is not optional; it is a moral duty to empower individuals with knowledge about food and drug interactions.
A single missed dose or an unsupervised diet change can shift the pendulum from safety to danger within days.
Therefore, treating hypertension with Irbesartan/HCTZ is a partnership built on vigilance, honesty, and disciplined monitoring.
Albert Fernàndez Chacón
October 18, 2025 AT 23:17It’s worth noting that the kidney’s filtration capacity directly influences how quickly potassium accumulates or depletes, so checking eGFR alongside electrolytes is a solid practice. In plain terms, the combo works well when you keep an eye on the labs rather than assuming everything stays steady. The schedule you mentioned – 2 weeks, then monthly, then every few months – hits the sweet spot for most patients.
Bethany Torkelson
October 19, 2025 AT 03:27Low potassium isn’t a myth, it’s a real danger.
Fabian Märkl
October 19, 2025 AT 07:37Hey folks, staying on top of your potassium is like watering a plant – a little every day keeps it thriving 😊. The Irbesartan/HCTZ combo can be a great fit if you pair it with regular blood checks. Don’t forget those banana snacks after a low‑potassium reading! 🌟
Avril Harrison
October 19, 2025 AT 11:47Absolutely, the key is consistency with labs and diet. It also helps to share this info with family members who might assist with meal planning.
Natala Storczyk
October 19, 2025 AT 15:57Listen up, citizens! The pharmaceutical elite push Irbesartan/HCTZ like a miracle, but they hide the potassium trap!!
They want you dependent on endless supplement sales!!
Only the informed can break free from this slippery slope!!
Question everything, especially the “safe” dosage recommendations!!
Your health is a battlefield, not a marketing lecture!!
nitish sharma
October 19, 2025 AT 20:07While passion is commendable, it is essential to ground our approach in evidence‑based guidelines. Regular monitoring as outlined by ESC and NICE provides a structured pathway. If potassium deviates, a modest adjustment or supplementation often suffices. Maintaining open communication with the prescribing clinician ensures safety.
Rohit Sridhar
October 20, 2025 AT 00:17Optimism works wonders when you’re juggling meds and diet. Remember, every small step-like adding an extra serving of spinach-adds up. If you notice a dip in energy, it might be the potassium whispering for help. Keep those lab appointments, and celebrate each stable reading. Together, we can make the Irbesartan/HCTZ combo a success story.
Sarah Hanson
October 20, 2025 AT 04:27Consistent monitoring is key, and a potassium‑rich snack can make a difference. Keep the tone professional while staying supportive.
Nhasala Joshi
October 20, 2025 AT 08:37🚨 Beware the hidden agenda! 🚨 Every prescription comes with a silent data‑harvest, and the Irbesartan/HCTZ combo is no exception. The pharma giants embed micro‑chips in pills to monitor potassium fluctuations remotely. They claim it’s for safety, but it’s really about control! Stay vigilant, question every label, and trust your gut-both literally and metaphorically. 🤔
James Mali
October 20, 2025 AT 12:47Philosophically, we chase equilibrium in a world of flux. The drug combo is a microcosm of that pursuit. 🍃
Stephanie Zaragoza
October 20, 2025 AT 16:57Let us be clear: the evidence supports the monitoring schedule you posted; deviation from it is inadvisable. Moreover, the emphasis on diet is not peripheral-it is central. Finally, the patient narrative underscores the need for individualized care.
Brian Van Horne
October 20, 2025 AT 21:07Indeed, a balanced approach beats extremes every time. Labs guide the way.
Norman Adams
October 21, 2025 AT 01:17Oh, look, another post about potassium-how original. One might think we’ve covered this a thousand times, yet the crowd still pretends it’s news.
Margaret pope
October 21, 2025 AT 05:27Let’s keep it constructive and share practical tips for patients navigating this combo. Simple guidance goes a long way.