When you get a burn, the pain and swelling can feel overwhelming. You might reach for anything that promises relief-cool water, aloe, or even that leftover steroid cream from your eczema flare-up. But is fluocinolone safe for burns? And does it actually help, or could it make things worse?
What is fluocinolone?
Fluocinolone is a potent topical corticosteroid. It’s not your average hydrocortisone cream. It’s about 100 times stronger than over-the-counter hydrocortisone and is usually prescribed for stubborn skin conditions like psoriasis, eczema, or severe allergic reactions. It works by calming down inflammation, reducing redness, itching, and swelling. But that same power can be dangerous if used on the wrong kind of skin injury.
Fluocinolone comes in creams, ointments, and sometimes scalp solutions. The most common strengths are 0.01% and 0.025%. It’s not sold over the counter in the UK or US-you need a prescription. That’s because misuse can lead to serious side effects, especially on broken skin.
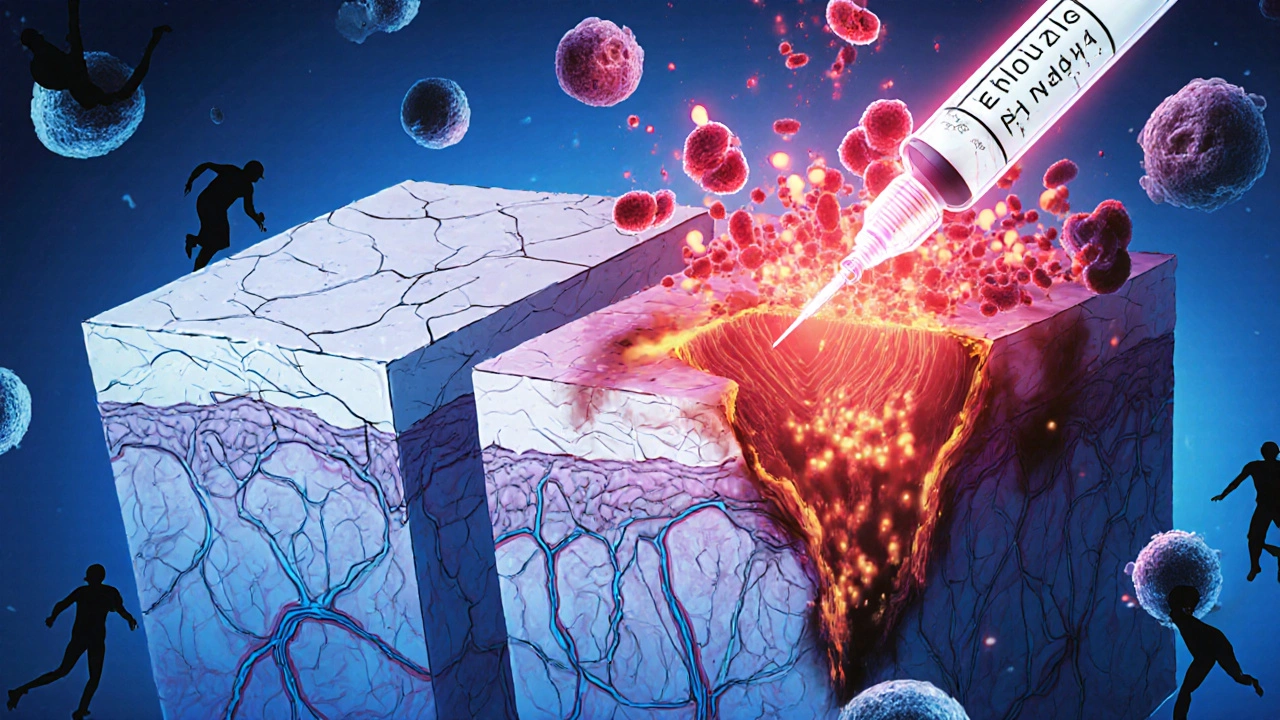
Why burns are different from eczema
Think of your skin like a wall. In eczema, the wall is cracked and leaky, but it’s still mostly intact. In a burn, especially a second-degree or deeper, that wall is partially or fully destroyed. Open tissue, exposed nerves, fluid loss-these are not conditions you want to treat with a strong steroid.
Fluocinolone suppresses the immune response. That’s great for stopping an overactive immune system attacking healthy skin. But with burns, your body needs that immune response to fight infection and start healing. Blocking it can delay healing and raise the risk of infection. A 2023 study in the Journal of Burn Care & Research found that topical corticosteroids, including fluocinolone, were linked to higher rates of bacterial colonization in partial-thickness burns compared to standard silver sulfadiazine treatment.
When fluocinolone might be used after a burn
There’s one exception: healed or nearly healed burns. Once the skin has re-epithelialized-meaning new skin has grown over the wound-some doctors may prescribe fluocinolone to manage scarring and itching. This is called hypertrophic scarring or keloid prevention.
In these cases, fluocinolone isn’t treating the burn itself. It’s treating the aftermath. The steroid helps flatten raised scars and reduces the intense itching that often follows burn recovery. A 2022 clinical review in Plastic and Reconstructive Surgery showed that low-dose fluocinolone (0.01%) applied twice daily for 6-8 weeks improved scar texture and reduced pruritus in 72% of patients with post-burn scars.
But even here, it’s not first-line. Silicone gel sheets and pressure garments are usually tried first. Fluocinolone is a backup when those don’t work enough.
What happens if you use fluocinolone on an open burn?
Using fluocinolone on an open or blistered burn is risky. Here’s what can go wrong:
- Infection risk increases: Steroids suppress local immune cells. Bacteria like Staphylococcus aureus and Pseudomonas aeruginosa can take over quickly in a compromised wound.
- Delayed healing: Corticosteroids interfere with collagen production and fibroblast activity-both essential for tissue repair.
- Thinning skin: Fluocinolone can cause atrophy, making the skin paper-thin. On burned areas, this can lead to permanent damage or easy tearing.
- Systemic absorption: Large or deep burns absorb more medication. You could end up with adrenal suppression, high blood sugar, or even Cushing’s syndrome from long-term use.
A case report from the British Journal of Dermatology in 2024 described a 34-year-old who applied fluocinolone 0.025% to a second-degree burn from a stove. Within 10 days, the wound worsened, developed pus, and required surgical debridement. The patient needed antibiotics and skin grafts.
What should you use instead for burns?
For minor burns (first-degree, red and painful, no blisters), stick to these proven methods:
- Cool the burn under running water for 10-15 minutes.
- Apply a sterile, non-stick dressing.
- Use aloe vera gel or a simple moisturizer like petroleum jelly.
- Take ibuprofen for pain and inflammation.
For second-degree burns (blisters, wet, shiny skin), see a doctor. Treatment usually includes:
- Antibiotic ointments like silver sulfadiazine or mupirocin
- Non-adherent dressings (e.g., Tegaderm, Xeroform)
- Regular wound cleaning and monitoring
For third-degree burns (white, charred, numb skin), call emergency services immediately. These require hospital care, IV fluids, and often surgery.

How to tell if your burn is healing properly
Healing isn’t just about pain going away. Here’s what real healing looks like:
- Redness fades over days, not weeks
- Fluid stops oozing within 48-72 hours
- New skin forms evenly, without dark patches or raised edges
- Itching is mild and improves over time
If you notice any of these, stop what you’re doing and get medical help:
- Wound gets more painful instead of less
- Pus, foul smell, or greenish discharge
- Fever over 38°C (100.4°F)
- Red streaks spreading from the burn
When to talk to your doctor about fluocinolone and burns
If you’ve already used fluocinolone on a burn, don’t panic-but don’t ignore it either. Call your GP or go to urgent care if:
- The burn hasn’t improved after 3 days
- You’ve used the cream for more than a week
- You’re on other steroids (oral or inhaled)
- You have diabetes, a weakened immune system, or are pregnant
If you’re recovering from a burn and have a scar that’s raised, red, and itchy, ask your doctor about fluocinolone as a scar treatment. But make sure the skin is fully closed first. Never use it on open wounds.
Bottom line: Don’t use fluocinolone on fresh burns
Fluocinolone is a powerful tool-but only in the right hands and the right situation. For burns, it’s not a quick fix. It’s a potential hazard. The pain might feel urgent, but rushing into steroid use can turn a minor injury into a serious medical issue.
Stick to the basics: cool, cover, clean, and consult. Your skin will thank you.
Can I use fluocinolone on a first-degree burn?
No. Even first-degree burns involve damaged skin. Fluocinolone can delay healing and increase infection risk. Use cool water, aloe vera, or petroleum jelly instead. Avoid all prescription steroids on open or red skin unless directed by a doctor.
Is fluocinolone the same as hydrocortisone?
No. Fluocinolone is a Class II corticosteroid-much stronger than hydrocortisone, which is Class VII. Fluocinolone is about 100 times more potent. Hydrocortisone cream from the pharmacy is safe for minor rashes, but fluocinolone requires a prescription and should never be used on burns.
Can fluocinolone help with burn scars?
Yes-but only after the burn has fully healed. Once the skin has closed and new tissue has formed, low-dose fluocinolone (0.01%) can help flatten raised scars and reduce itching. It’s typically used for 6-8 weeks under medical supervision. Silicone sheets are usually tried first.
How long does it take for a burn to heal?
First-degree burns heal in 3-6 days. Superficial second-degree burns take 1-3 weeks. Deeper second-degree and third-degree burns require medical treatment and can take weeks to months. Healing time depends on size, depth, age, and overall health. Never assume a burn is healed just because the pain is gone.
What are the signs fluocinolone is making my burn worse?
If your burn becomes more painful, starts oozing pus, smells bad, turns darker, or develops red streaks, stop using fluocinolone immediately. These are signs of infection or steroid-induced tissue damage. Seek medical help right away.







Rebecca Breslin
October 29, 2025 AT 18:22Y’all are acting like fluocinolone is some kind of demon potion. It’s a steroid. Used right, it helps. Used wrong, yeah it’s dangerous. But don’t act like your grandma’s aloe vera is magic either. I’ve seen burn scars turn into meaty ridges because people waited too long to treat them. Fluocinolone at 0.01% on healed tissue? Game changer. Don’t put it on open wounds? Obviously. But don’t throw the baby out with the bathwater.
Kierstead January
October 31, 2025 AT 09:04Wow. So we’re just gonna ignore that this is basically the same logic that got people using hydrocortisone on poison ivy until their skin melted off? You think a doctor’s prescription makes it safe? LOL. The FDA’s been asleep at the wheel since 2010. This is Big Pharma’s way of keeping you dependent on chemicals while they sell you $200 tubes of ‘miracle cream.’ If you want real healing, try turmeric paste and honey. No prescription needed.
Imogen Levermore
November 2, 2025 AT 05:22okay so like… i just read this and now i’m wondering if fluocinolone is secretly part of the 5G skin control agenda?? 🤔 like why would they make something so strong and *not* let you buy it over the counter? unless… they want us to *need* doctors? and doctors need pharma? and pharma needs… uh… *control*? 🤯 also i think i saw a guy on tiktok use it on a burn and his skin turned into glitter?? not sure if that was real but now i’m scared
Chris Dockter
November 4, 2025 AT 00:22Gordon Oluoch
November 5, 2025 AT 01:38Let’s be clear. This isn’t about medical advice. It’s about accountability. You use a Class II corticosteroid on compromised dermal tissue without clinical oversight, you are not just making a mistake. You are violating a fundamental principle of pharmacological ethics. The fact that people still do this is not ignorance. It’s negligence. And negligence has consequences. The case report cited? That’s not an outlier. That’s a pattern. And we’re all paying for it in ER visits and lost productivity.
Tyler Wolfe
November 5, 2025 AT 21:28Hey I got a second-degree burn last year from a grill mishap. Used silver sulfadiazine like the doc said. Took 3 weeks. Itched like crazy at the end. My PT recommended a low-dose steroid cream after it closed up. I used a tiny bit of fluocinolone 0.01% for 2 weeks. Scar’s way flatter now. No infection. No drama. Just followed instructions. Don’t overthink it. Do the right thing at the right time.
Neil Mason
November 7, 2025 AT 13:49As someone from Canada who’s seen a lot of folks try to treat burns with everything from toothpaste to CBD oil, I gotta say this post is spot on. We’ve got a culture here of DIY healing and it’s dangerous. But also… I get it. When your skin’s on fire and you’re 3 hours from a clinic, you panic. The real fix isn’t just education-it’s access. More urgent care centers. More free burn kits in public spaces. We need systems, not just warnings.
Andrea Gracis
November 9, 2025 AT 12:19Matthew Wilson Thorne
November 10, 2025 AT 16:01Fluocinolone isn’t the villain. The lack of medical literacy is.
April Liu
November 12, 2025 AT 04:28Big thank you for this. I’ve been dealing with a burn scar that itched nonstop for months. My dermatologist finally suggested fluocinolone 0.01% after 6 months of silicone sheets not helping enough. Used it for 8 weeks. The itching dropped by 80%. The scar’s still there but it’s soft now. Don’t be scared of it-be informed. And please, please don’t use it until the skin is fully closed. I almost made that mistake. 😅
Emily Gibson
November 12, 2025 AT 19:47This is such a needed post. I’ve seen so many people try to use leftover steroid creams on burns because they ‘just need to calm the redness.’ I get it. It’s tempting. But you’re not just delaying healing-you’re risking infection, scarring, and even systemic effects. Please, if you’re unsure, wait. Call your doctor. Text a nurse line. It’s worth it. Your skin remembers what you do to it.
Mirian Ramirez
November 13, 2025 AT 20:45Okay so I used fluocinolone on my burn after I got scalded by hot oil and I thought it was helping because the redness went away but then the skin got super thin and I could see the veins and it started cracking and I panicked and went to the ER and they were like oh my god what did you do?? And I was like I just wanted it to stop hurting?? And they said you basically gave yourself a chemical burn on top of a burn?? I had to get skin grafts on my forearm and now I have a scar that looks like a map of the moon. So if you’re thinking about using it on a burn… don’t. Just don’t. Even if it’s just a little. Even if it’s ‘just a first-degree.’ I’m 28 and I still cry when I look at my arm. Please learn from me.
Kika Armata
November 15, 2025 AT 09:02Let’s not pretend this is about science. This is about class. Fluocinolone is expensive. It requires a prescription. It requires access to a doctor who won’t judge you for being ‘irresponsible.’ Meanwhile, the poor are left with aloe from the dollar store and a prayer. The real question isn’t whether fluocinolone works-it’s why we’ve built a system where the only safe way to treat a burn is to have enough money to get a specialist who won’t tell you you’re dumb for not knowing better.
Herbert Lui
November 17, 2025 AT 03:40There’s a quiet violence in how we treat pain. We reach for chemicals not to heal-but to silence the signal. A burn screams. And we want it to shut up. Fluocinolone doesn’t heal. It muffles. And sometimes, when you silence the scream, you miss the warning. The body doesn’t lie. It just gets louder when you ignore it. Maybe the real treatment isn’t cream at all… it’s patience. And presence. And letting the pain be part of the process.