Medication Timing Checker
Check Your Medication Timing
Discover if the time you take your medication matters based on biological rhythms
Timing Analysis
CRITICAL
Best Time:
Why It Matters:
Key Impact
Tip: Use a medication reminder app with alarms for high-risk drugs.
What if taking your pill at 8 a.m. instead of 8 p.m. could make it less effective-or worse, more dangerous? It’s not science fiction. For many medications, timing isn’t just a suggestion-it’s a safety rule. The body doesn’t operate on a flat 24-hour cycle. It pulses. It slows. It wakes up. And when you take your medicine matters just as much as how much you take.
Why Your Body Cares When You Take Your Pills
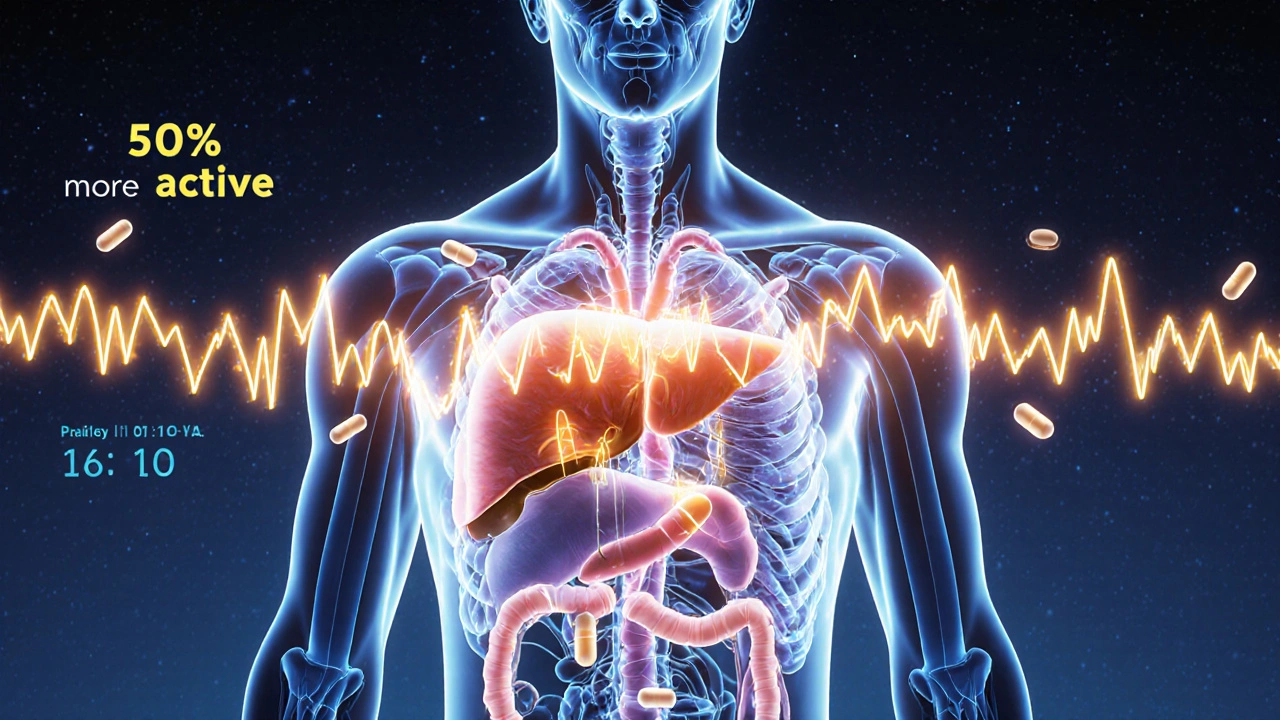
Your body runs on a clock. Not a wristwatch, but a biological one-called the circadian rhythm. This internal timer controls everything from your sleep-wake cycle to how your liver breaks down drugs. Studies show liver enzymes that metabolize medications can be up to 50% more active at night than during the day. That means the same dose taken in the morning might stay in your system longer, increasing side effects. At night, it might clear too fast, reducing its effect. Take statins, for example. These cholesterol-lowering drugs work best when taken in the evening. Why? Because your liver makes most of its cholesterol at night. Taking the pill then means the drug is working right when it’s needed most. Research shows evening doses lower LDL (bad) cholesterol by 15-20% more than morning doses. That’s not a small difference-it’s the difference between staying healthy and needing a stent. The same goes for blood pressure meds. A major study called MAPEC found that taking ACE inhibitors at bedtime reduced heart attacks, strokes, and heart failure by 29% compared to taking them in the morning. Why? Because blood pressure naturally dips at night. If your medication doesn’t match that rhythm, you’re not protecting your heart when it’s most vulnerable.High-Risk Medications: When Minutes Matter
Not all drugs are created equal when it comes to timing. Some can wait. Others can’t. For high-risk medications, being off by even 15 minutes can have real consequences. Insulin is one of them. If you take rapid-acting insulin too early before a meal, your blood sugar can crash. Too late, and it spikes dangerously high. Studies show mistimed insulin causes hypoglycemia in 22% of cases. That’s more than one in five people. In hospitals, nurses often have to rush between patients, and even a 30-minute delay can turn a routine dose into an emergency. Anticoagulants like warfarin are another. Timing errors here can increase bleeding risk by up to 37%. Why? Because the drug’s effect builds slowly over hours. If you take it at 6 p.m. one day and 11 a.m. the next, your blood’s ability to clot swings unpredictably. That’s why many doctors insist on the same time every day-no exceptions. Chemotherapy drugs are even more sensitive. Deviating from the scheduled time by more than 30 minutes can cut effectiveness by 15-20%. Cancer cells divide at certain times of day. Timing chemo to hit them at their weakest point isn’t just smart-it’s life-saving.When Timing Doesn’t Matter (Much)
Before you panic, not every pill needs a stopwatch. Some medications are forgiving. Hydrochlorothiazide, a common water pill for high blood pressure, can be taken anytime within a 12-hour window with little effect on safety or results. Same with many antibiotics and pain relievers like ibuprofen. The key is knowing which is which. A 2007 study in the Journal of the American Medical Informatics Association classified drugs by “timing criticality.” Some need precision. Others don’t. The problem? Most patients-and even many doctors-don’t know the difference. You might be told to take your pill “in the morning,” but no one tells you why. That’s where chronotherapy comes in. It’s not a new drug. It’s a smarter way to use the ones you already have. By matching the drug’s action to your body’s rhythm, you get better results with fewer side effects-no extra cost, no new prescriptions.
Why Hospitals Get It Right (And You Don’t)
In hospitals, timing errors are tracked. Nurses use barcode scanners. Systems flag late doses. Staff get trained. And yet, 48-53% of IV medication doses still get given late or early. Why? Interruptions. A nurse is called away to check on another patient. A phone rings. A family member asks a question. Each interruption increases the chance of a timing mistake. A JAMA Internal Medicine study found that with five interruptions during a med pass, error rates jumped from 39% to 61%. Five interruptions. That’s it. And in the real world, nurses face 10, 15, even 20 per shift. At home, it’s worse. A survey of 1,200 patients found 68% failed to stick to their scheduled times. Why? Work schedules. Kids’ activities. Forgetfulness. Low health literacy. One woman told researchers she took her evening statin at lunch because she forgot until then. Another took his blood pressure pill after his morning coffee because he was too tired to get up earlier. The truth? We live in a world that doesn’t respect biological clocks. We work nights. We scroll at 2 a.m. We eat at odd hours. And we expect our meds to work the same no matter when we take them.What You Can Do Right Now
You don’t need a PhD to get timing right. Here’s how to start:- Ask your pharmacist: “Is the time I take this important?” Don’t assume. Many don’t know.
- Use alarms: Set two: one for the time you should take it, and another 15 minutes later as a backup.
- Keep a log: Write down when you take each pill for a week. You’ll spot patterns-like always forgetting your evening dose because you’re watching TV.
- Group your meds: If you take multiple pills, ask if they can be taken together. Some can. Some can’t. But you won’t know unless you ask.
- Know your high-risk drugs: Insulin, warfarin, chemo, beta-blockers, and certain seizure meds need strict timing. Treat them like fuel for a jet-not a soda you can drink whenever.






Suzan Wanjiru
November 22, 2025 AT 21:51Statins at night makes total sense-my dad’s LDL dropped 22% after his pharmacist told him to switch from morning to bedtime. He used to take it with breakfast like everyone told him to. Turns out, his liver was just ignoring it until 11 p.m. Now he sleeps better too.
Henrik Stacke
November 24, 2025 AT 17:37As someone who’s spent 12 years in NHS wards, I can tell you-timing isn’t a suggestion, it’s a protocol. We had a case where a patient on warfarin took his dose at 8 a.m. one day and 6 p.m. the next. INR spiked to 8.7. He nearly bled out in the hallway. No one had explained circadian metabolism to him. Just ‘take it daily.’ That’s criminal negligence in my book.
Manjistha Roy
November 25, 2025 AT 21:20My grandmother took her blood pressure meds at random times for years because she said she ‘forgot’-until she had a mild stroke. Now she uses a pillbox with alarms. No emojis, no fuss, just discipline. If you’re serious about your health, treat your meds like your oxygen tank-not your snack drawer.
Jennifer Shannon
November 26, 2025 AT 04:52I’ve been thinking about this for months now-how we treat our bodies like machines that run on ‘whenever,’ when in reality we’re biological symphonies. The liver doesn’t punch a clock, but it does dance to a rhythm older than civilization. And we’re out here swallowing pills like candy, hoping the universe doesn’t notice we’re out of sync. It notices. It always notices. The body doesn’t lie. It just gets tired of screaming.
When I switched my statin from morning to night, my muscle aches vanished. Not because I changed the dose, but because I finally listened. I didn’t need a study. I needed silence. I needed to stop rushing. I needed to remember that healing isn’t a to-do list. It’s a conversation.
And maybe that’s the real crisis-not that people forget their meds, but that we’ve forgotten how to be still long enough to hear what our bodies are trying to say. We schedule meetings. We track steps. We set alarms for coffee. But we don’t schedule reverence.
I used to think chronotherapy was just science. Now I think it’s a spiritual practice. Taking your pill at the right time isn’t compliance-it’s communion. With your cells. With your ancestors. With the moon, the sun, the quiet pulse beneath your skin that’s been ticking since before you were born.
And if you’re reading this and thinking, ‘I’m too busy,’ then maybe the real medication you need isn’t in the bottle. Maybe it’s in the pause. In the breath before you swallow. In the moment you stop and say: ‘I matter enough to get this right.’
Olanrewaju Jeph
November 28, 2025 AT 02:49Correct timing of anticoagulants is critical. A 2021 study in the Nigerian Journal of Clinical Pharmacology showed that 63% of patients on warfarin who took their doses inconsistently experienced major bleeding events within 18 months. This is preventable. Patients need structured education, not just prescriptions. Community health workers can play a vital role in monitoring adherence through weekly phone calls.
Kane Ren
November 29, 2025 AT 02:00Just started taking my beta-blocker at night and wow-I actually slept through the night for the first time in years. No more 3 a.m. heart palpitations. I didn’t even know that was a thing until I read this. Life-changing stuff. Thank you for sharing this.
Charmaine Barcelon
November 29, 2025 AT 20:01You people are overcomplicating this. Just take your pills at the same time every day. If you can’t do that, maybe you shouldn’t be on meds. End of story.
Kezia Katherine Lewis
December 1, 2025 AT 13:51Chronotherapy’s integration into EHRs is a significant advancement in pharmacokinetic personalization. The FDA’s mandate for chronopharmacology data in 17 new NDAs reflects a paradigm shift from population-based dosing to circadian-optimized regimens. Clinically, this reduces inter-individual variability in drug exposure, particularly for substrates of CYP3A4 and CYP2C9 enzymes, whose expression oscillates diurnally.
However, real-world implementation remains hampered by patient-reported barriers: socioeconomic constraints, cognitive load, and fragmented care coordination. The ChronoGene cohort data, pending publication, may offer genotype-guided chronodosing algorithms that could eventually be embedded into clinical decision support systems.
Until then, pharmacists must assume the role of circadian educators-not just dispensers. The disconnect between evidence and practice persists because we still treat chronobiology as an elective, not a cornerstone of therapeutics.
Lisa Detanna
December 1, 2025 AT 22:18What’s wild is that we’ve known this for decades-yet nothing changes. I work in a hospital pharmacy. We have a whole shelf of meds labeled ‘Take at bedtime’ and 80% of patients ask, ‘Can I take it with lunch?’ It’s not ignorance. It’s systemic. No one taught them. No one made it easy. We need standardized patient handouts, not just verbal instructions. And maybe a damn app that pings you like your Uber driver.
Jennifer Skolney
December 2, 2025 AT 14:28This is the most important post I’ve read all year. I used to take my insulin whenever I remembered… until I passed out at the grocery store. Now I have three alarms. One for the time, one for 15 mins later, and one for ‘did you eat?’ I’m alive because I finally listened. Thank you for saying this.
JD Mette
December 3, 2025 AT 00:49I’ve been taking my blood pressure meds at 7 a.m. for 12 years. My doctor never mentioned timing. Just ‘take it daily.’ I’m glad I read this. I’ll switch to bedtime tomorrow. No drama. Just… better.
Henrik Stacke
December 3, 2025 AT 05:07Exactly. And if you’re a nurse or caregiver-don’t just assume they know. Ask. Show them. Make it visual. A sticky note on the mirror. A voice note on their phone. Tiny things. Big impact.