Bromocriptine Timing Calculator
How to Use This Calculator
Bromocriptine (Cycloset) must be taken within 2 hours of waking for maximum effectiveness. Enter your typical wake-up time below to see your optimal dosing window and learn how to avoid nausea.
Most people with type 2 diabetes start with metformin. But if that doesn’t work, or if you can’t take it, there’s another option most doctors don’t talk about: bromocriptine. Specifically, the quick-release version called Cycloset. It’s not flashy like GLP-1 drugs, and it doesn’t make you lose weight. But it does something no other diabetes pill does-it targets your brain’s internal clock to lower blood sugar and cut your risk of heart attack or stroke. The catch? It’s easy to mess up. Take it at the wrong time, and it won’t work. Take it on an empty stomach, and you might feel sick for weeks. This is the real-world guide to making bromocriptine work for you-not against you.
How Bromocriptine Actually Works (It’s Not What You Think)
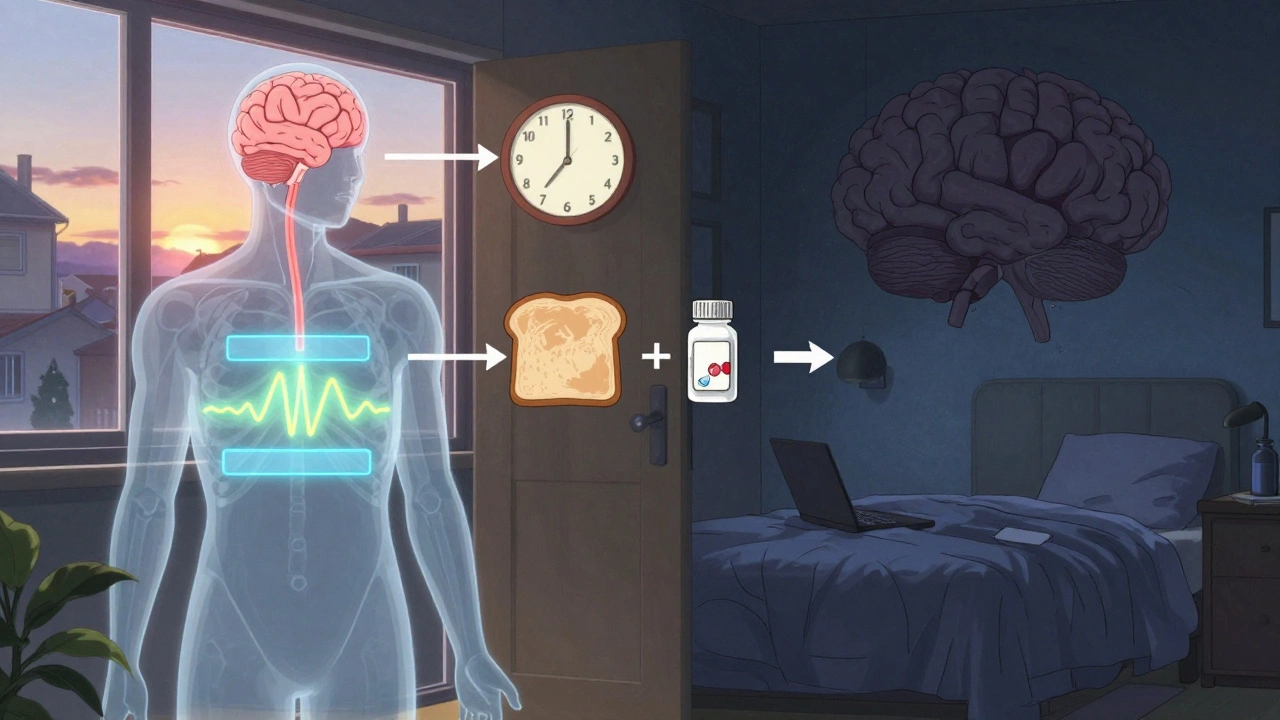
Bromocriptine doesn’t boost insulin. It doesn’t block sugar absorption. It doesn’t even make your body more sensitive to insulin like metformin does. Instead, it talks to a tiny area in your brain called the hypothalamus. That’s the part that controls your body’s daily rhythms-when you wake up, when you feel hungry, when your liver releases glucose. In people with type 2 diabetes, this system gets stuck in overdrive. Your liver dumps out too much sugar in the morning, even if you haven’t eaten. Your nerves fire too much, making your muscles resistant to insulin. Bromocriptine resets that clock. It calms down the overactive signals, so your body behaves more like it did when you were younger. That’s why, after 24 weeks, people on bromocriptine see their HbA1c drop by 0.4% to 0.8%. It’s not huge, but it’s steady. And unlike other drugs, it doesn’t cause weight gain or low blood sugar. In fact, a major study showed people taking it had 40% fewer heart attacks, strokes, or heart-related deaths over a year. That’s why it’s still around, even though it’s not the first choice.
Why Timing Is Everything-And What Happens If You Get It Wrong
This is the part most patients miss. Bromocriptine only works if you take it within two hours of waking up. Not when you get to work. Not after your coffee. Not when you finally feel awake. Two hours after you open your eyes. That’s because your brain’s dopamine system is most responsive to the drug in the early morning. If you take it at noon, it’s like trying to turn off a light switch after the sun’s already up. The effect is gone.
One study found patients who took it at the right time dropped their HbA1c by 0.7% more than those who didn’t. That’s the difference between a good result and a useless one. Night shift workers? It’s a problem. If you wake up at 6 p.m., you’re supposed to take it by 8 p.m. That’s not practical. Most doctors will switch you to something else. But if you work days and sleep at night, set an alarm. Put the pill on your nightstand. Make it part of your morning routine-right after brushing your teeth, before you get out of bed.
The Nausea Problem-And How to Beat It
One in three people who start bromocriptine quit because of nausea. It’s not mild. It’s the kind that makes you want to lie down, skip breakfast, and cancel your day. But here’s the good news: it gets better. And there are proven ways to make it manageable.
The key is slow dosing. Don’t start at 4.8 mg. That’s the max. Start with 0.8 mg once a day for a full week. Then go to 1.6 mg for a week. Then 2.4 mg. Keep adding 0.8 mg each week until you hit 4.8 mg. This six-week ramp-up cuts nausea from 32% down to 18%. That’s huge.
Take it with food-dry food. One slice of toast. Two plain crackers. Nothing greasy. Nothing sugary. Just something to coat your stomach. A study found 78% of people who did this reported much less nausea. Avoid liquids for 30 minutes after taking it. Water can speed up absorption and make nausea worse.
Try ginger. Not the candy. Not the tea. A 250 mg capsule taken 30 minutes before your dose. One clinical trial showed it reduced nausea severity by 40%. It’s cheap, safe, and works better than most anti-nausea pills for this specific issue.

Dizziness: The Morning Fog You Can’t Ignore
Dizziness hits about 1 in 8 people. It’s not vertigo. It’s not fainting. It’s that weird, floating feeling right after you stand up-like your head’s too light. It lasts 15 to 30 minutes. And yes, it’s from the drug.
Bromocriptine can lower blood pressure slightly, especially in the morning. That’s why sitting up slowly matters. Don’t jump out of bed. Sit on the edge for a minute. Let your body adjust. Then stand. Wait another 10 minutes before you start walking around or making coffee. Most people find the dizziness fades after two to four weeks of consistent use. If it doesn’t, talk to your doctor. Your dose might be too high, or you might need to switch.
Who Should Even Try This Drug?
Bromocriptine isn’t for everyone. It’s not a first-line drug. But it’s a smart choice if you:
- Have type 2 diabetes and heart disease-or major risk factors like high blood pressure, smoking, or high cholesterol
- Can’t take metformin because of stomach issues or kidney problems
- Want to avoid weight gain or low blood sugar
- Have a consistent morning routine and can stick to the timing
It’s not a good fit if you:
- Work nights or have irregular sleep
- Get dizzy easily or have a history of fainting
- Have severe kidney disease (eGFR under 30)
- Can’t tolerate even mild nausea for a few weeks
Most prescriptions come from endocrinologists or cardiologists-not regular GPs. That’s because this drug needs a plan. You can’t just pick it up and go. You need guidance.
How It Compares to Other Diabetes Pills
Let’s be clear: bromocriptine doesn’t lower blood sugar as much as metformin (which drops HbA1c by 1.1%) or newer drugs like semaglutide (which can drop it by 1.5% or more). But it does something they don’t: it cuts heart risks. In head-to-head studies, it reduced heart attacks and strokes by 40% compared to placebo. That’s not matched by DPP-4 inhibitors or SGLT2 drugs in the same way. SGLT2 inhibitors help the heart too, but they cause dehydration, yeast infections, and sometimes ketoacidosis. Bromocriptine doesn’t. It’s weight-neutral. No hypoglycemia. Just a small drop in blood sugar-and a big drop in heart risk.
The trade-off? Side effects and timing. Metformin can give you diarrhea, but you can take it anytime. Bromocriptine? You have to be a morning person. And you have to tolerate the nausea at first. That’s why it’s only used by 0.8% of people with type 2 diabetes in the U.S. It’s a niche tool. But for the right person, it’s the only tool that does what it does.
What to Do If It’s Not Working
If you’ve been on bromocriptine for 12 weeks and your HbA1c hasn’t budged, talk to your doctor. It could be timing. Maybe you’re taking it after your coffee. Maybe you’re skipping the toast. Maybe you rushed the dose increase. Keep a log: write down what time you took it, what you ate, and how you felt. Bring it to your appointment.
If nausea never improves, or dizziness lasts more than a month, don’t suffer. There are other options. GLP-1 agonists, SGLT2 inhibitors, even insulin if needed. But if you’ve tried those and they didn’t fit, bromocriptine might still be worth another shot-with better support.
The manufacturer now offers a program called Cycloset Success. It includes personalized coaching on timing, nausea tips, and even reminders. If your doctor doesn’t mention it, ask. You’re not supposed to figure this out alone.
What’s Next for Bromocriptine?
A big trial called BROADEN-CV is wrapping up in late 2025. It’s testing 3,500 people with diabetes and heart disease to see if bromocriptine really does cut heart events long-term. If the results are strong, it could move from a niche option to a standard recommendation for high-risk patients. Until then, it’s a quiet hero in diabetes care-underused, misunderstood, but uniquely powerful for the right person.
If you’re considering it, don’t give up after the first week of nausea. Stick with the slow ramp-up. Take it with toast. Set your alarm. Wait 20 minutes before you rush out the door. It’s not easy. But for some, it’s the difference between managing diabetes-and managing your future.








Carole Nkosi
December 4, 2025 AT 13:12They don't want you to know this because Big Pharma makes more money off GLP-1s that turn you into a walking skeleton. Bromocriptine is ancient, cheap, and it works on the root cause - your broken circadian rhythm. They’d rather sell you a $10,000 shot that makes you vomit and lose your appetite. This is medicine as control, not healing.
an mo
December 4, 2025 AT 16:49Per the 2023 ADA guidelines, bromocriptine-QR (Cycloset) demonstrates a modest HbA1c reduction (Δ -0.7%) with a statistically significant CVD risk attenuation (HR 0.60, 95% CI 0.47–0.77) per the BRIGHT trial. However, its pharmacokinetic profile is highly time-sensitive - Cmax occurs within 1.5–2h post-ingestion, and bioavailability plummets if administered outside the 2-h post-awakening window due to dopaminergic receptor desensitization.
aditya dixit
December 4, 2025 AT 22:34This is one of the most thoughtful explanations of bromocriptine I’ve ever read. Most people chase the flashy drugs, but the real magic is in syncing with your body’s rhythm. The slow titration tip? Gold. So many people quit because they rush - like trying to sprint before learning to walk. And the ginger trick? Simple, ancient, effective. It’s not about finding the strongest drug. It’s about finding the right one for your life.
Lynette Myles
December 6, 2025 AT 20:24They’re hiding this because it’s a dopamine modulator - same class as antipsychotics. They don’t want you to know your diabetes is being treated with a drug that alters brain chemistry. Next they’ll say your depression is just a clock problem.
Annie Grajewski
December 8, 2025 AT 01:03ok but like… who even *is* this drug for? i took it for 3 days and felt like a zombie who missed caffeine for 3 weeks. also why is the brand called Cycloset? sounds like a yoga retreat. also why does it taste like regret?
Mark Ziegenbein
December 9, 2025 AT 04:26Let me tell you something - most doctors are lazy. They don’t care about your circadian rhythm. They just want to hand you a script and call it a day. Bromocriptine? It’s not a pill. It’s a lifestyle. It demands discipline. It demands silence in the morning. It demands you rise before the world and sit still with your own biology. Most people can’t handle that. They’d rather take a drug that makes them lose weight and then complain about being hungry all the time. I’ve been on it for 18 months. My HbA1c is 5.8. My blood pressure is down. And I haven’t had a single episode of dizziness since week 5. But I didn’t just take it. I honored it.
Rupa DasGupta
December 9, 2025 AT 21:47Ugh I tried this and it made me feel like my brain was melting. I cried for 3 days. I’m not even diabetic but I read this and now I’m scared to wake up. 😭
Marvin Gordon
December 10, 2025 AT 17:31Don’t let the nausea scare you off. It’s the worst in week one. After that? It fades. I took mine with two crackers and a cup of warm water. No coffee for 45 minutes. Set three alarms. One to wake up, one for the pill, one to sit still. It’s not glamorous. But after six weeks, I felt like I had my mornings back. This isn’t a magic bullet. It’s a quiet reset.
ashlie perry
December 12, 2025 AT 16:53They’re testing this in 3500 people because they know it works and they’re scared it’ll expose how overpriced everything else is. The real trial is whether they’ll ever let this be OTC. They won’t. Too cheap. Too simple. Too real.
Juliet Morgan
December 13, 2025 AT 20:02I’ve been on this for 4 months. The nausea was brutal at first. But the toast trick? Lifesaver. And ginger capsules - I get them at the grocery store. I didn’t even know they existed. I’m not a morning person… but now I am. Because I have to be. And it’s worth it.
Norene Fulwiler
December 15, 2025 AT 11:44In India, we’ve used circadian rhythm-based healing for centuries - sunrise routines, fasting until noon, morning walks. This drug just confirms what ancient medicine knew: timing matters. We don’t need fancy pills. We need to remember how to live.
William Chin
December 16, 2025 AT 18:14While I acknowledge the clinical efficacy and temporal specificity of bromocriptine-QR, I must emphasize that its administration must be strictly supervised by a licensed endocrinologist or cardiologist, particularly in patients with comorbid hypotension or autonomic dysfunction. Self-administration without prior cardiovascular risk stratification constitutes a significant medical liability.