More than one in three adults between 60 and 70 are taking five or more prescription drugs at once. By age 75, that number jumps to 41%. It’s not just common-it’s becoming the norm. But here’s the problem: the more pills you take, the higher the chance one will clash with another. A simple mix of blood pressure medicine and a common painkiller could send you to the hospital. Or worse. You might not even notice it’s happening until it’s too late.
Why Medication Conflicts Happen
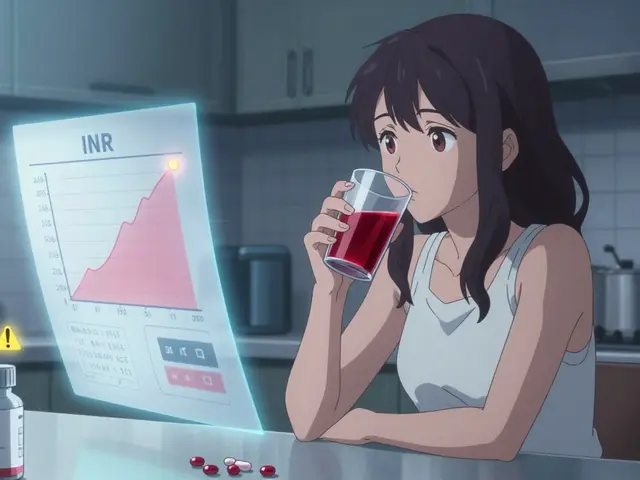
It’s not that doctors are careless. It’s that modern medicine works too well. We treat high blood pressure, diabetes, arthritis, depression, and heart disease-all at the same time. Each condition needs its own drug. Add in supplements, over-the-counter pain relievers, and herbal teas, and you’ve got a cocktail that even pharmacists struggle to keep track of.The biggest danger? Drug interactions. Some combinations can cause kidney damage. Others can make you dizzy, drowsy, or cause internal bleeding. NSAIDs like ibuprofen, for example, are linked to 22% of preventable hospital stays in seniors because they raise blood pressure and hurt the stomach when mixed with other meds. And here’s the scary part: 82% of dangerous interactions happen with things patients don’t tell their doctors-like turmeric pills, fish oil, or melatonin.
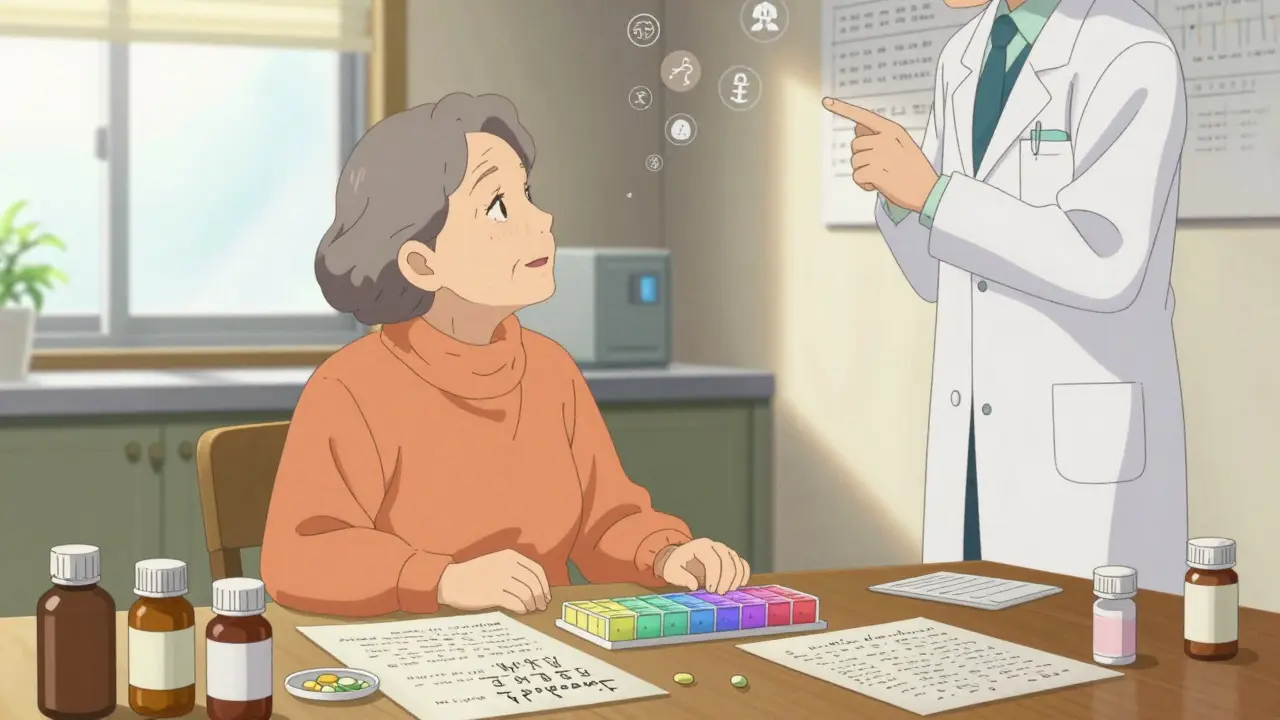
Your Medication List: The First Line of Defense
You can’t manage what you can’t see. Start with a real, written list-not a note on your phone, not a mental tally. Include every single thing you take:- Brand name and generic name (e.g., Lisinopril, also sold as Zestril)
- Dosage (e.g., 10 mg)
- When to take it (e.g., “Take with breakfast,” “Take at bedtime”)
- Why you’re taking it (e.g., “for high blood pressure”)
- Special instructions (e.g., “Avoid grapefruit,” “Take on empty stomach”)
Don’t forget vitamins, supplements, and OTC drugs. Many people think “natural” means safe. It doesn’t. St. John’s Wort can make your antidepressant useless. Calcium can block thyroid meds if taken too close together. Write it all down. Keep a printed copy in your wallet and another on your fridge.
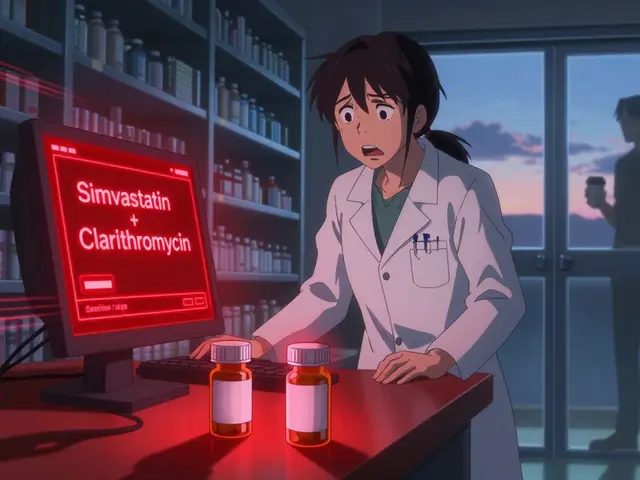
Use One Pharmacy Only
This is the single most effective thing you can do. If you get your blood pressure meds from one pharmacy, your painkillers from another, and your diabetes pills from a third, no one has the full picture. Pharmacists can’t warn you about a dangerous mix if they don’t know about all your drugs.Studies show pharmacies that see all your prescriptions catch 94% of potential interactions. When prescriptions are split across multiple pharmacies, that drops to 47%. That’s more than double the risk. Switching to one pharmacy doesn’t mean you’re stuck with bad service. Most chains and independent pharmacies now offer free medication reviews and refill reminders.
Medication Synchronization: Get All Your Refills on One Day
Imagine getting all your monthly pills on the same day-say, the first Tuesday of every month. No more juggling different refill dates. No more forgetting one pill because you were busy last week. That’s medication synchronization.It’s simple: you tell your pharmacy you want all your maintenance meds (not PRN or as-needed drugs) synced to one pickup date. They adjust your refill schedules so everything lines up. You might need to pick up some pills early or late for the first few weeks, but after 2-3 weeks, it’s smooth sailing.
The results? People in sync programs have 31% fewer missed doses, 22% fewer ER visits, and save $1,200-$1,800 a year in avoided hospital bills. Medicare Part D requires pharmacies to offer this to patients on 8+ medications for two or more chronic conditions. Ask your pharmacist if you qualify.
Pill Organizers: Don’t Guess What You Took
If you take four or more pills a day, a simple pill organizer isn’t a luxury-it’s a necessity. Look for a 7-day organizer with morning and afternoon compartments. Fill it once a week, preferably on Sunday evening while watching your favorite show. That routine makes it stick.One study with 1,245 seniors showed adherence jumped from 62% to 87% in six months just by using a basic organizer. Some advanced models, like Hero Health’s smart dispenser, beep, flash, and even call your family if you miss a dose. But they cost nearly $900. For most people, a $10 plastic organizer from CVS does the job.
Important: Don’t just dump all your pills in. Some meds can’t be stored long-term in plastic. Check with your pharmacist. Also, never store pills in the bathroom-it’s too humid. Keep them in a cool, dry place like a kitchen cabinet.
Digital Tools: Helpful, But Not for Everyone
Apps like Medisafe and MyMeds send alerts, track doses, and even tell you if a new drug might interact with your current ones. In trials, users were 28% more likely to take their meds on time than those using paper logs.But here’s the catch: 62% of adults over 75 don’t use smartphones regularly. If you’re not comfortable with tech, don’t force it. A paper list and a pill box work better than an app you never open. If you do use an app, make sure a family member can access it too-so they can help if you forget.
Timing Matters More Than You Think
It’s not just what you take-it’s when. Some drugs need space between them. Take calcium supplements too close to your thyroid medicine, and your body won’t absorb either properly. Wait at least two hours. Proton pump inhibitors like omeprazole work best 30 minutes before breakfast. If you take them after, they’re half as effective.Ask your pharmacist: “Are there any of my meds that need to be spaced apart?” Write those times down on your list. Use alarms on your phone or a kitchen timer if you need help remembering.

Deprescribing: Sometimes Less Is More
Just because you’ve been taking a pill for years doesn’t mean you still need it. Blood pressure meds, cholesterol drugs, even antidepressants can sometimes be safely reduced-or stopped-after your condition improves. But never quit on your own.The American Geriatrics Society recommends regularly reviewing every medication. Ask your doctor: “Is this still necessary? Could I take less? Are there side effects I’m ignoring?” Many seniors are taking drugs that were prescribed for short-term use years ago. A 2023 study found 1 in 5 older adults were still on antibiotics they’d been given for a urinary infection five years earlier.
What to Do If You Think Something’s Wrong
If you start feeling unusually tired, dizzy, confused, nauseous, or have unexplained bruising or swelling-stop blaming it on aging. These are red flags. They could mean your meds are clashing.Call your pharmacist first. They’re trained to spot interactions. Don’t wait for your next doctor’s appointment. Many community pharmacies now offer free Medication Therapy Management (MTM) sessions. Pharmacists spend 20-25 minutes going over your list, checking for risks, and making suggestions. You don’t need an appointment-just walk in.
The Bigger Picture
Medication coordination isn’t about being organized-it’s about staying alive. Every year, over 277,000 people in the U.S. die from preventable drug reactions. The cost? $300 billion in wasted healthcare spending. But here’s the good news: every dollar spent on coordinated care saves $7.20 in hospital bills.Women take 17% more medications than men. Rural patients visit four or more providers a year, making coordination even harder. If you’re in either group, you’re at higher risk. That means you need to be even more proactive.
Start today. Make your list. Pick one pharmacy. Ask about sync. Get a pill organizer. Talk to your pharmacist. You don’t need to fix everything at once. Just take one step. Then another. Your body will thank you.






Dave Alponvyr
December 16, 2025 AT 06:35They say take one pill at a time, but then they hand you a whole damn pharmacy. I’ve got my grandpa’s list taped to the fridge - and still, I forget half of it. Simple? Yeah. Easy? Nah.
Cassandra Collins
December 16, 2025 AT 17:54EVERYONE knows the pharma companies plant those pills to keep you hooked. They don’t want you to heal - they want you to keep buying. Turmeric? That’s a natural blood thinner. They banned it in 1998 but let it sneak back in as a ‘supplement.’ Don’t trust the system.
Tiffany Machelski
December 17, 2025 AT 19:32i just started using a pill box and it changed my life. i used to take my blood pressure med at night by accident and then wonder why i was dizzy all day. now? i fill it every sunday with my tea and its like a little ritual. still typo prone but at least i’m not dead.
Hadi Santoso
December 18, 2025 AT 15:45As someone who grew up in Jakarta with a mom who mixed traditional jamu with her statins, I can tell you - coordination isn’t just American advice. It’s survival. My aunt in Bali takes 11 meds and still walks 5 miles a day. She writes everything on a scrap of paper tied to her keychain. No app. No fancy organizer. Just memory, trust, and a lot of tea. The system may be broken, but people? We adapt.
Arun ana
December 19, 2025 AT 00:27Love this post! 🙌 I’ve been syncing my mom’s meds with her local pharmacy in Mumbai and it’s been a game-changer. She used to miss doses because of different refill days. Now? One day a month, one trip. Even the pharmacist remembers her name now 😊
Kayleigh Campbell
December 19, 2025 AT 05:33They call it polypharmacy. I call it ‘The Great Pill Circus.’ You’re not sick - you’re a human pharmacy. And the worst part? No one’s holding the ringmaster accountable. I once asked my doctor why I was on a blood thinner I didn’t need. He said, ‘Well, you were on it in 2017.’ That’s not a plan. That’s a habit. And habits kill.
Andrew Sychev
December 20, 2025 AT 01:42THIS is why elderly people are dying in their sleep. The system is designed to kill you slowly. Doctors don’t care. Pharmacies don’t care. They just want your insurance to keep paying. You think your pills are helping? They’re just keeping you alive long enough to pay for more pills. Wake up.
Dan Padgett
December 21, 2025 AT 15:29You know what’s wild? Back home in Lagos, folks don’t have pill organizers or synced refills. They use matchsticks. One stick for each pill, every morning. Burn one, take one. Simple. No tech. No apps. Just rhythm. Maybe the answer isn’t more tools - maybe it’s just remembering that your body isn’t a machine. It’s a story. And every pill’s a chapter.
Elizabeth Bauman
December 22, 2025 AT 18:23One pharmacy? Are you kidding? I’ve got Medicare and I’m not letting some foreign-owned chain dictate where I get my meds. I get my blood pressure pills from the VA, my painkillers from Costco, and my vitamins from the corner store. That’s American freedom. You want control? Take it. Don’t let them herd you like cattle.
Dylan Smith
December 24, 2025 AT 15:23My mom took 14 pills a day and never told anyone about the melatonin and the fish oil. Then she fell and broke her hip. Turns out the combo made her blood thin as water. We found the list in her sock drawer. I cried. Then I made her switch to one pharmacy. She hates it. But she’s alive. So I don’t care.