Every year, thousands of patients are at risk because someone handed them a pill, liquid, or injection that was past its expiration date. It’s not always negligence-it’s often a simple oversight. A cabinet full of meds, a busy shift, a stack of boxes in a storage room. But what if technology could do the work for you? What if your meds could tell you when they’re about to expire-before you even reach for them?
Why Medication Expiration Tracking Matters
Expired medications don’t just lose effectiveness. Some can become harmful. Antibiotics that degrade may not kill infections, leading to worse illness or antibiotic resistance. Insulin that’s been sitting too long won’t regulate blood sugar properly. Epinephrine auto-injectors in expired condition might fail during an allergic emergency. The FDA says most medications retain potency past their expiration date, but that’s not a guarantee-and in healthcare settings, you don’t gamble with safety. Hospitals and pharmacies lose millions annually to expired drugs. One study found that a mid-sized hospital can throw away $150,000 worth of expired meds each year. That’s not just waste-it’s a safety failure waiting to happen. Technology doesn’t just help you avoid that-it makes tracking automatic, accurate, and foolproof.How RFID Systems Work for Medication Tracking
RFID (Radio Frequency Identification) is the most powerful tool in this space. Each medication bottle, vial, or blister pack gets a tiny, invisible tag. These tags don’t need line-of-sight like barcodes. A single scan can read 100 items at once-whether they’re in a drawer, a crash cart, or a refrigerator. Systems like KitCheck use UHF RFID to scan entire trays in seconds. The software knows exactly what’s in each container, when it was stocked, and when it expires. When a drug is within two days of expiring, the system flags it. It won’t let you dispense it. No manual entry. No missed dates. No guesswork. Texas Children’s Hospital started using RFID to track 784 high-value drugs-each costing over $100. Before, pharmacists spent hours manually checking lot numbers and expiration dates. Now, it takes minutes. They cut inventory checks from 8 hours down to 45 minutes. And they hit 100% accuracy in stock counts-up from 65-75% with manual methods.Electronic Medication Administration Records (eMAR)
If you work in long-term care, home health, or intellectual and developmental disabilities (IDD) agencies, eMAR is your go-to. These aren’t just digital charts-they’re smart systems that link directly to pharmacy orders. When a nurse gives a pill, they scan the patient’s wristband and the medication’s barcode. The system logs the time, the dose, and the expiration date. If the medication is expired or about to expire, it blocks the action and sends an alert. It also auto-generates reports for audits, compliance checks, and recalls. eVero’s platform, for example, integrates with pharmacy systems so orders are automatically generated when stock runs low. It even requires biometric login-so only authorized staff can administer meds. In IDD agencies, where staff turnover is high and training is limited, eMAR has cut medication errors by over 60% since 2020.Automated Dispensing Cabinets (ADCs)
Think of ADCs as smart medication vending machines. Used in hospitals and closed-door pharmacies, they store controlled substances, IV bags, and oral meds. Each drawer locks until the right person logs in. When a nurse takes a drug, the cabinet automatically records:- Who took it
- What was taken
- Lot number
- Expiration date
Mobile Solutions for EMS and Field Teams
Emergency responders don’t have access to hospital systems. But they still need to know if their epinephrine, naloxone, or glucose gel has expired. That’s where LogRx comes in. LogRx runs on standard iPhones and Androids. No new hardware. Just download the app, scan the barcode on each medication, and the system tracks expiration dates in real time. When a drug is due to expire in 30 days, it sends a push notification. When it expires, it turns red and locks out the item. Portland Fire & Rescue started using LogRx in 2023. They reported a 70% drop in administrative time spent on medication logs. They also passed DEA inspections with zero findings-something they hadn’t done in five years. Matt Gibson, Clinical Lead at Elite EMS in the UK, said: “It’s not just compliance-it’s culture. We’re now seen as leaders in medicine safety because we’re using tech others still ignore.”What You Need to Get Started
You don’t need a billion-dollar budget. But you do need a plan. Step 1: Assess your needsAre you a hospital with hundreds of drugs? Then RFID or ADCs make sense. Are you a small clinic or home care agency? Start with eMAR or a mobile app like LogRx. Step 2: Pick the right system
- RFID: Best for large hospitals, operating rooms, high-value meds.
- eMAR: Best for long-term care, home visits, IDD facilities.
- ADCs: Best for controlled substances in hospitals.
- Mobile apps: Best for EMS, field teams, small pharmacies. Step 3: Plan the rollout
Implementation takes 8 to 17 weeks. You’ll need:
- 2-4 weeks to evaluate vendors and choose software
- 1-3 weeks to install hardware
- 2-6 weeks to train staff
- 2-4 weeks to test and fix glitches
Costs and ROI
RFID systems cost between $50,000 and $200,000 upfront. That sounds steep. But consider this: one hospital saved $280,000 in a year by cutting expired drug waste. Another saved 1,200 hours of staff time on inventory checks. That’s over 60 full workdays. eMAR and mobile apps cost far less-often under $10,000 per year for a small clinic. And they pay for themselves in months. The American Hospital Association estimates that by 2027, 45% of U.S. hospitals will use RFID for medication tracking. That’s up from 25% today. The market is growing because the ROI is undeniable.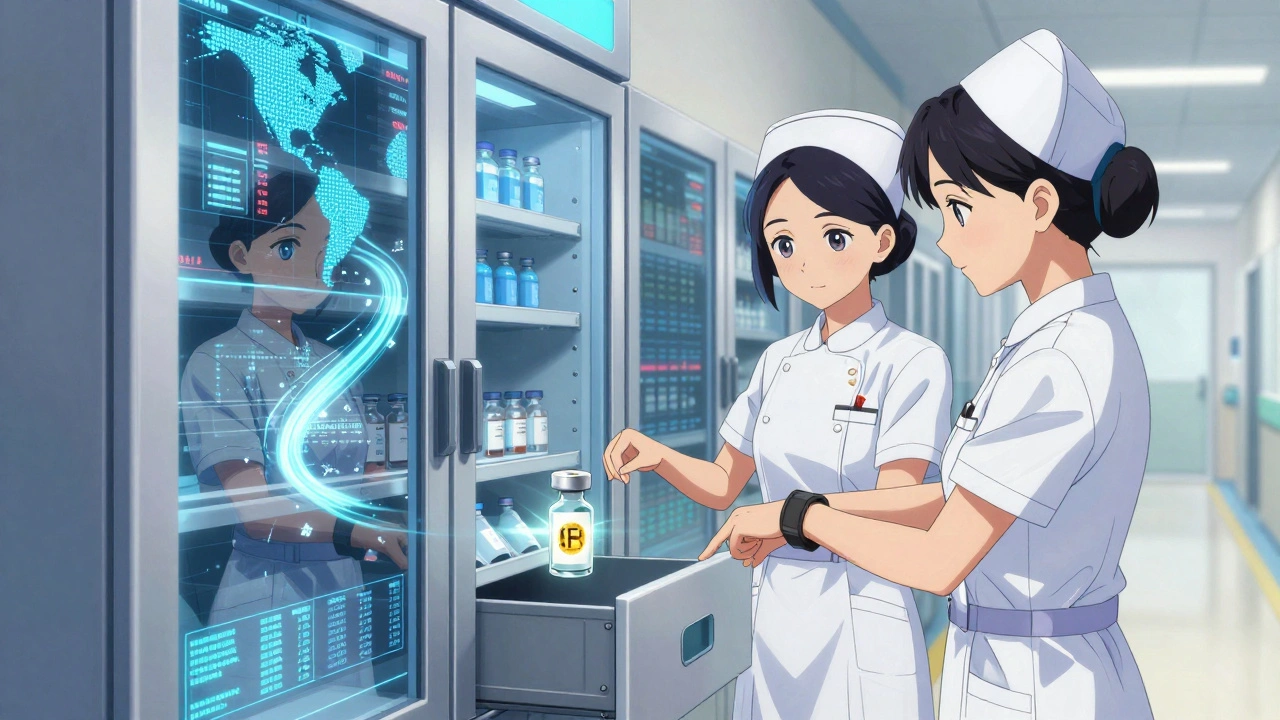
What’s Next? AI and Blockchain
The future is smarter. Intelliguard Health is testing AI that predicts which meds are most likely to expire based on usage patterns. It doesn’t just alert you-it tells you to reorder before you run out. Blockchain is being piloted to track meds from manufacturer to patient. If a batch is recalled, you’ll know instantly which patients got it. No delays. No guesswork. And manufacturers are starting to pre-tag meds with RFID before they even ship. That means hospitals won’t need to tag each bottle themselves. Implementation time drops from weeks to days.Common Mistakes to Avoid
Don’t make these errors:- Trying to use barcode scanners for everything-RFID is faster and more accurate.
- Skipping staff training-tech fails without buy-in.
- Choosing a system that doesn’t integrate with your EHR or pharmacy software.
- Ignoring maintenance-tags can wear out, readers need updates.
Final Thought: It’s Not About Tech-It’s About Safety
Technology doesn’t replace good judgment. But it removes the chance for human error. In a world where one expired pill can lead to hospitalization-or death-automated tracking isn’t a luxury. It’s the baseline. If you’re still managing expiration dates by hand, you’re not just behind-you’re vulnerable. The tools exist. The data proves they work. The only question left is: when will you start using them?Can I use my phone to track medication expiration dates?
Yes. Apps like LogRx work on standard iPhones and Android devices. You scan the barcode on each medication, and the app tracks expiration dates, sends alerts, and blocks expired items. It’s ideal for EMS teams, home care nurses, and small clinics without complex systems.
Do RFID tags work on all types of medications?
Most can be tagged, including pills, liquids, injections, and inhalers. The tags are tiny and designed to be attached to packaging without affecting the drug. Some fragile items like glass vials may need special handling, but vendors provide solutions. Pre-tagged medications from manufacturers are becoming more common, making this easier.
Is RFID better than barcode scanning for medication tracking?
Yes, in most healthcare settings. Barcodes require line-of-sight and must be scanned one at a time. RFID reads multiple items simultaneously-even if they’re stacked or in a drawer. It’s 10 times faster and reduces human error. Hospitals using RFID report 100% inventory accuracy, compared to 65-75% with barcodes.
How much does medication tracking technology cost?
Costs vary. RFID systems for large hospitals range from $50,000 to $200,000. eMAR platforms and mobile apps like LogRx cost $5,000-$15,000 per year. ADCs can cost $20,000-$50,000 per cabinet. Most systems pay for themselves in under a year through reduced waste, labor savings, and avoiding fines.
What happens if a medication expires in the system?
The system blocks it from being dispensed. Alerts go to pharmacists or nurses. Some systems automatically flag the item for return or destruction and update inventory logs. In emergency situations, overrides are possible-but only with dual authentication and a documented reason.
Are there legal requirements to track medication expiration dates?
Yes. The FDA’s Drug Supply Chain Security Act requires traceability of prescription drugs. The DEA mandates strict tracking of controlled substances. CMS requires long-term care facilities to maintain accurate medication records. While manual tracking is still allowed, automated systems are the only way to reliably meet these standards without risk.
Can small clinics afford medication tracking tech?
Absolutely. Mobile apps like LogRx and basic eMAR platforms start under $10,000 per year. Many vendors offer tiered pricing, pay-as-you-go models, or grants for nonprofit clinics. The cost of not using tech-expired drugs, compliance fines, patient harm-is far higher.






Iris Carmen
December 9, 2025 AT 22:57Shubham Mathur
December 11, 2025 AT 12:22Sabrina Thurn
December 12, 2025 AT 18:47Noah Raines
December 14, 2025 AT 17:50Stacy Tolbert
December 15, 2025 AT 01:04Chris Marel
December 16, 2025 AT 23:33Nikhil Pattni
December 18, 2025 AT 09:44Larry Lieberman
December 18, 2025 AT 13:49Courtney Black
December 18, 2025 AT 17:48Andrea Beilstein
December 19, 2025 AT 06:40Morgan Tait
December 20, 2025 AT 16:29precious amzy
December 21, 2025 AT 15:57Brianna Black
December 22, 2025 AT 07:57Maria Elisha
December 22, 2025 AT 18:21