Dermatomyositis and polymyositis are rare autoimmune diseases that cause severe muscle inflammation and progressive weakness. Together, they affect tens of thousands of Americans, but diagnosis often takes months due to symptom overlap with other diseases like lupus or fibromyalgia.
Key Takeaways
- Dermatomyositis includes skin rashes; polymyositis does not.
- Diagnosis requires blood tests, EMG, and muscle biopsy for confirmation.
- Corticosteroids like prednisone are first-line treatment, but long-term use risks osteoporosis and diabetes.
- Recent advances include JAK inhibitors and abatacept for treatment-resistant cases.
- Early treatment within six months of symptoms leads to better long-term outcomes.
What Are Dermatomyositis and Polymyositis?
Dermatomyositis is an autoimmune condition where the immune system attacks muscle tissue and skin blood vessels. It causes muscle weakness and distinctive rashes. The name comes from 'derma' (skin) and 'myositis' (muscle inflammation).
Polymyositis is similar but lacks skin involvement. It primarily affects muscles, leading to progressive weakness in shoulders, hips, and neck. Both conditions are rare, with polymyositis affecting 1-7 per 100,000 people annually and dermatomyositis 0.6-10 per 100,000.
The American College of Rheumatology notes these conditions are more common in women-two to three times more likely than men. Dermatomyositis has two age peaks: children aged 5-15 and adults 40-60, while polymyositis mainly affects adults over 20.
Symptoms and Key Differences
Dermatomyositis and polymyositis share muscle weakness symptoms but differ in skin involvement. Dermatomyositis patients develop a heliotrope rash-a purple or red rash on eyelids, face, neck, elbows, knuckles, and knees. This rash often appears before muscle weakness. Polymyositis patients typically experience muscle weakness without skin changes.
Common symptoms for both include:
- Progressive weakness in proximal muscles (shoulders, hips, thighs, neck)
- Difficulty climbing stairs, rising from chairs, or lifting objects
- Unexplained fatigue that worsens daily tasks
- Swallowing difficulties (dysphagia) in 15-30% of cases
Dermatomyositis also commonly involves interstitial lung disease in 30-40% of patients, while polymyositis rarely affects the lungs directly. Additionally, 20% of dermatomyositis cases are linked to cancer-especially ovarian, lung, or gastrointestinal-making cancer screening essential at diagnosis.

Diagnosis Process
Diagnosing these conditions takes time-often 3-6 months from symptom onset. Doctors start with blood tests to check for elevated CPK levels. Normal CPK is 10-120 U/L; in myositis, it often exceeds 500 U/L, sometimes 5-10 times higher.
Electromyography (EMG) measures electrical activity in muscles. Abnormal patterns like short-duration motor unit potentials indicate muscle inflammation. However, the gold standard is a Muscle Biopsy, which reveals different patterns: dermatomyositis shows perifascicular atrophy and perivascular inflammation, while polymyositis features T-cell infiltration around muscle fibers.
Specialists also test for myositis-specific antibodies (MSAs), which help distinguish between conditions. For example, anti-Mi-2 antibodies are common in dermatomyositis, while anti-synthetase antibodies may point to polymyositis or overlap syndromes.
Treatment Options
First-line treatment for both conditions is corticosteroids like prednisone. Doctors typically start with 1 mg/kg daily (about 40-60 mg for adults) for 4-8 weeks, then slowly taper the dose. However, long-term steroid use causes side effects: 30-50% of patients develop osteoporosis, 15-30% get diabetes, and 20-40% develop cataracts.
For treatment-resistant cases, second-line immunosuppressants are used:
- Methotrexate or Azathioprine for long-term control
- Intravenous Immunoglobulin (IVIG) shows strong results in refractory dermatomyositis
- Rituximab (a B-cell therapy) has 60-70% response rates in severe cases
Recent trials show promise with JAK inhibitors like tofacitinib. A 2023 study found 65% improvement in skin scores and 52% muscle strength recovery in dermatomyositis patients after 24 weeks. Similarly, Abatacept trials for polymyositis show 40% of participants achieving minimal disease activity at six months.
Managing Long-Term Care and Side Effects
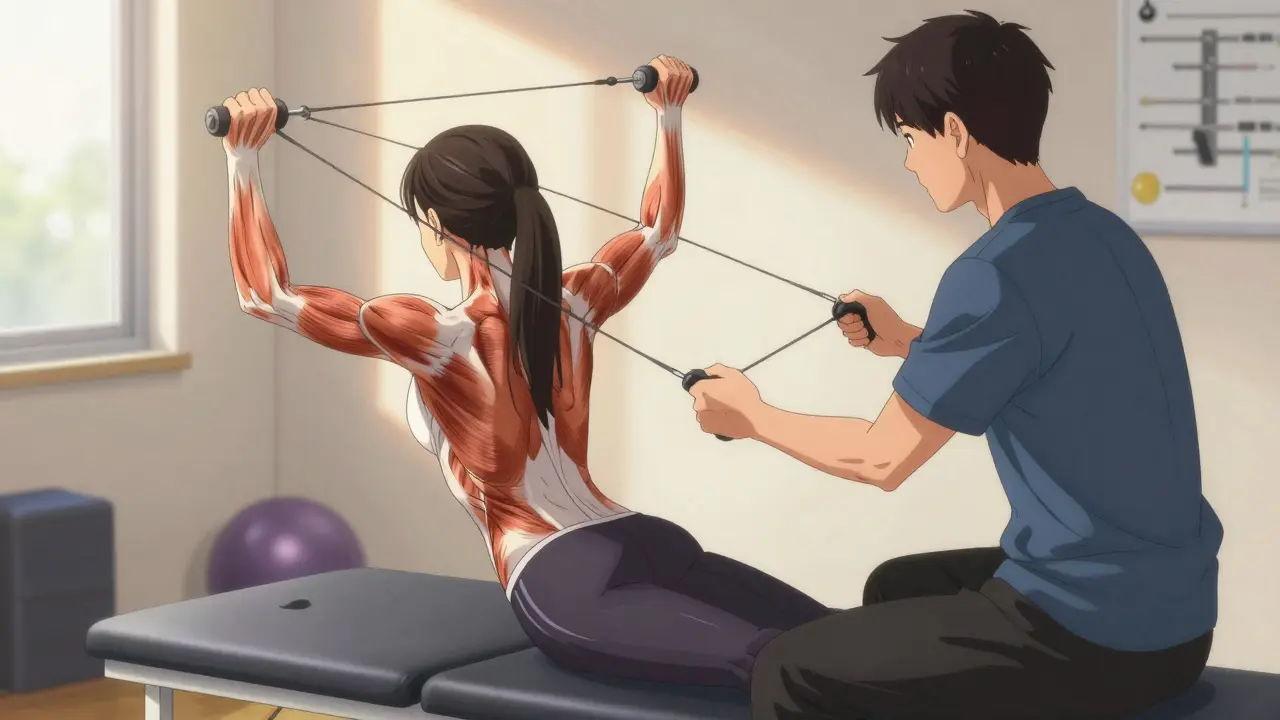
Living with dermatomyositis or polymyositis requires ongoing management. Physical therapy is critical-starting within two weeks of diagnosis-to maintain mobility without worsening inflammation. A 2022 Hospital for Special Surgery report found structured exercise programs improved functional capacity by 35-45% over six months.
For steroid side effects, doctors often prescribe calcium and vitamin D supplements to protect bones. Patients should also monitor blood sugar regularly and get annual eye exams. Swallowing difficulties may require speech therapy; 15-30% of patients experience dysphagia, which can lead to malnutrition if untreated.
Regular cancer screenings are essential for dermatomyositis patients due to the 20% malignancy link. This includes mammograms, colonoscopies, and pelvic exams based on risk factors. The Myositis Association's 2022 survey found 68% of patients struggle with fatigue, so pacing activities and energy conservation techniques are vital for daily life.
Frequently Asked Questions
Can dermatomyositis be cured?
There is no known cure for dermatomyositis or polymyositis. However, with proper treatment, most patients achieve remission or low disease activity. About 80% of those treated within six months of symptom onset see significant improvement. Long-term management is often needed to prevent relapse.
What are the most common side effects of prednisone?
Prednisone, a common corticosteroid treatment, can cause weight gain (82% of patients with side effects), insomnia (67%), osteoporosis (30-50% long-term), diabetes (15-30%), and cataracts (20-40%). Doctors often prescribe calcium, vitamin D, and bone density monitoring to manage these risks.
How long does diagnosis typically take?
Diagnosis often takes 3-6 months due to symptom overlap with other conditions like lupus or fibromyalgia. Initial blood tests, EMG, and muscle biopsy are required. The Myositis Support and Understanding Association reports patients visit an average of 4.7 specialists before getting an accurate diagnosis.
Is there a link between dermatomyositis and cancer?
Yes, approximately 20% of dermatomyositis cases are associated with cancer, particularly ovarian, lung, or gastrointestinal cancers. This link isn't seen in polymyositis. Doctors recommend thorough cancer screening at diagnosis, including imaging and blood tests based on risk factors.
What role does physical therapy play in treatment?
Physical therapy is essential for maintaining muscle function and preventing atrophy. Studies show structured exercise programs improve functional capacity by 35-45% over six months. Therapists focus on low-resistance exercises tailored to each patient's abilities to avoid overexertion while building strength.







Gregory Rodriguez
February 6, 2026 AT 09:34Diagnosis takes months? Yeah, because doctors love playing 'what's wrong with you' roulette. But hey, at least we have JAK inhibitors now. My doc says 65% skin score improvement. Not bad for a disease that's been a nightmare. Though, the side effects of prednisone are brutal-weight gain, insomnia, osteoporosis. I'm glad there's progress. Still, the cancer link with dermatomyositis is scary. Had to get a colonoscopy last year. But hey, at least they're testing for it. Maybe next time they'll find a cure. I've been on this rollercoaster for years, but the recent advances give me hope. Even with all the hurdles, the medical community's pushing hard. It's not perfect, but it's better than nothing. Still, the wait for a cure is agonizing. But hey, we'll get there. Maybe.
lance black
February 7, 2026 AT 02:09Early treatment within six months leads to better outcomes.
Pamela Power
February 7, 2026 AT 16:00It's laughable how many people still rely on prednisone as a first-line treatment. Modern medicine has moved on. JAK inhibitors and abatacept are the future, yet many physicians cling to outdated protocols. The lack of urgency in adopting new therapies is appalling. Patients deserve better than outdated, dangerous steroid regimens. This is why we need more specialists who actually understand the disease. Most doctors don't even know the difference between dermatomyositis and polymyositis. They just throw steroids at it and hope for the best. Pathetic.
Bella Cullen
February 8, 2026 AT 16:23Not sure why they're pushing JAK inhibitors so hard. Side effects could be worse. Maybe stick with what works. Just saying.
Phoebe Norman
February 10, 2026 AT 10:51Myositis-specific antibodies are crucial for diagnosis anti-Mi-2 for dermatomyositis anti-synthetase for polymyositis but many clinicians overlook them leading to misdiagnosis the lack of standardized testing protocols is a major issue
Samantha Beye
February 12, 2026 AT 06:40Physical therapy is essential. Start within two weeks of diagnosis to maintain mobility. Gentle exercises can prevent atrophy without worsening inflammation. It's important to pace yourself and listen to your body. You're not alone in this journey.
Rene Krikhaar
February 13, 2026 AT 04:19CPK levels above 500 indicate muscle inflammation but normal levels don't rule out myositis EMG and biopsy are more reliable for diagnosis the key is early intervention to prevent long-term damage
one hamzah
February 13, 2026 AT 13:27diagnosis takes months? yeah but the new treatments are promising 🌟 JAK inhibitors 65% skin improvement 🎉 cancer screening is a must for dermatomyositis patients though 🤔
Diana Phe
February 13, 2026 AT 19:51Why is the FDA so slow to approve new treatments? Big Pharma is blocking progress. The government should mandate faster approval for life-saving drugs. This is why we need national healthcare to cut out the greedy corporations.
Carl Crista
February 15, 2026 AT 00:45the real reason diagnosis takes months is because the medical system is designed to keep patients in the dark big pharma wants you dependent on prednisone forever
Andre Shaw
February 15, 2026 AT 07:36Everyone's jumping on the JAK inhibitor bandwagon but the real breakthrough is in stem cell therapy. The studies on that are way more promising than what they're pushing now. JAK inhibitors? Overrated. I've done my research.