Medication Switch Calculator
Compare Your Options
Enter your current and new medication side effect risks to see the real difference
Your Comparison
Absolute risk difference:
Current Treatment
Side effect risk: 0%
New Option
Side effect risk: 0%
Why switching medications isn’t just a doctor’s call
Switching medications can feel like a leap into the unknown. One pill stops working. Another gives you nausea every morning. Or maybe your doctor says a newer option is better-but you’re not sure if it’s worth the risk. What if you could see the real odds? Not vague warnings, but clear numbers: how many people out of 100 actually get side effects? How much does this drug lower your chance of a heart attack? That’s what decision aids do. They turn guesswork into informed choices.
What exactly is a decision aid for medication switching?
A decision aid isn’t a brochure or a website that just lists drug facts. It’s a structured tool designed to help you and your doctor make a decision together. It shows you the benefits and risks of staying on your current medicine versus switching to another. It doesn’t push you toward one option. It helps you figure out what matters most to you.
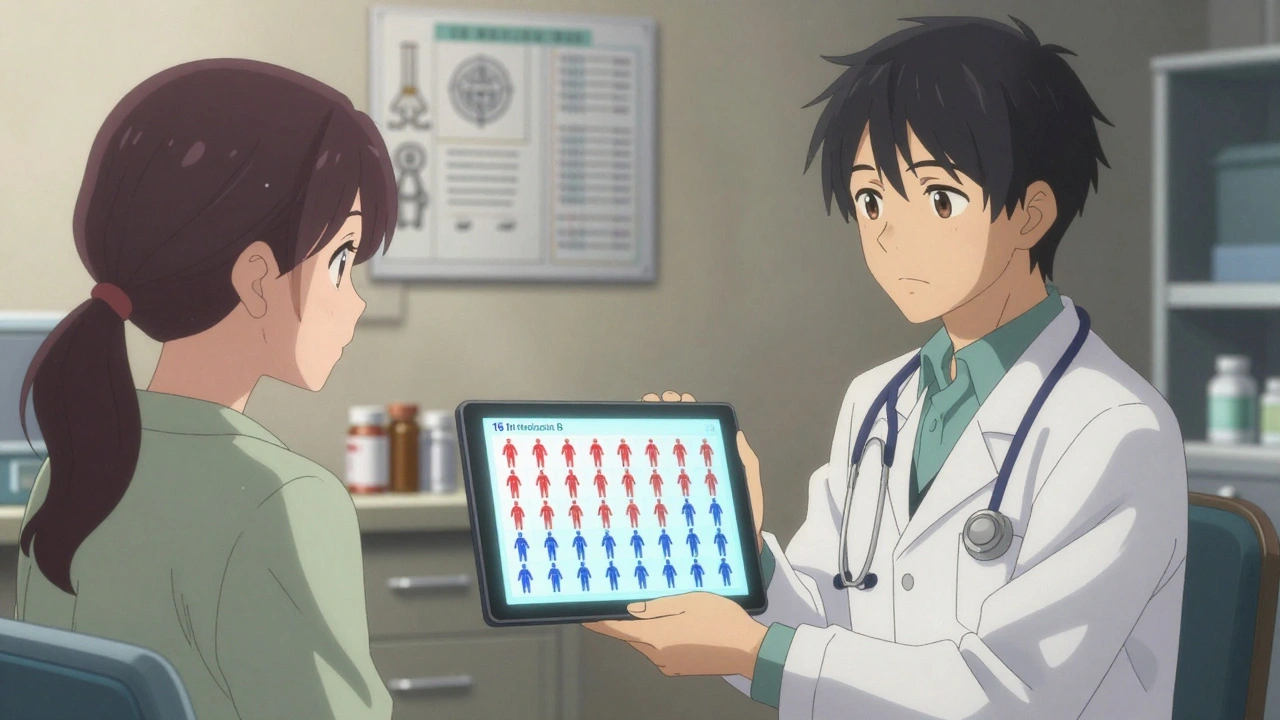
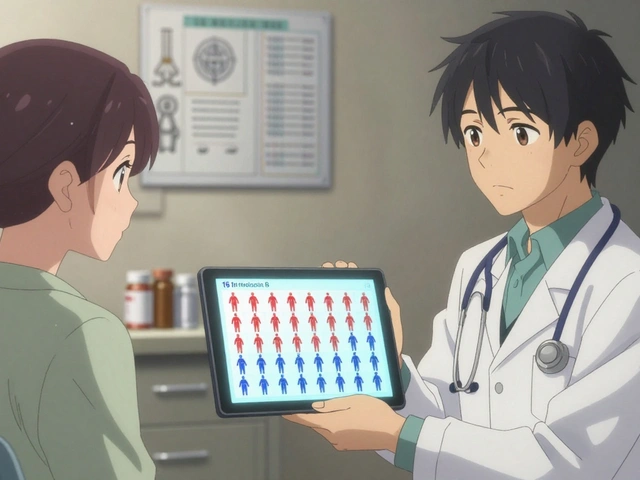
These tools use real data. For example, they might say: “Of 100 people taking Medication A, 30 will gain weight. Of 100 people taking Medication B, only 15 will.” They show this with simple pictures-like icons of 100 people, colored in to show who gets side effects. They ask you questions: Is cost more important than dosing frequency? Are you okay with a small risk of bleeding to avoid daily pills? Your answers guide the conversation.
How do these tools actually help patients?
Studies show patients who use decision aids understand their options better. One review of over 100 studies found people who used these tools scored 15-25% higher on tests about their medications than those who just got verbal advice. That’s not just a little better-it’s a big jump in understanding.
They also reduce anxiety. When you’re unsure whether to switch, you might feel stuck or overwhelmed. Decision aids cut through the noise. A veteran on Reddit shared how seeing an icon array of 100 people-3 with bleeding on a new blood thinner, 8 on his old one-made the choice feel real. “It wasn’t abstract anymore,” he wrote. “I could picture it.”
And it works. One 2022 study found patients using decision aids were 28% less likely to feel conflicted about their choice. That’s huge. Because when people feel confident, they stick with their treatment. And that’s the whole point.
When do decision aids work best-and when don’t they?
These tools shine when there’s no single “right” answer. For example, choosing between different diabetes drugs, antidepressants, or blood thinners. Each has pros and cons. One might help you lose weight. Another might be cheaper. One has a higher risk of nausea. None are clearly better for everyone. That’s when decision aids help the most.
But they’re not magic. They don’t help in emergencies. If you’re having a stroke and need a clot-buster now, there’s no time for a tool. They also struggle when patients have severe memory or thinking problems. If someone can’t process numbers or probabilities, the tool becomes confusing, not helpful.
And here’s a warning: some patients misinterpret the numbers. One study found 22% of people thought “reducing risk by 20%” meant they’d be completely safe. That’s not true. If your risk was 10%, a 20% reduction brings it down to 8%. That’s still a 1 in 12.5 chance. Decision aids need to be clear-not misleading.
What’s in a good decision aid?
A strong one includes four things:
- Clear options: What happens if you stay? What happens if you switch?
- Real numbers: Not percentages alone-absolute risks shown in simple visuals.
- Side effect comparisons: Side-by-side tables showing how often each drug causes weight gain, dizziness, fatigue, etc.
- Value clarification: Questions like: “How important is avoiding weight gain compared to avoiding daily injections?”
Tools from the VA, Mayo Clinic, and Ottawa Hospital Research Institute are widely trusted. The VA’s anticoagulant decision aid, for example, walks patients through bleeding risk versus stroke prevention across different life scenarios. It’s not just information-it’s a conversation starter.
Why aren’t more doctors using them?
Because they take time. A 2023 study found using a decision aid adds 7-12 minutes to a visit. In a 15-minute appointment, that’s a lot. Many doctors say they don’t have the time-or they’re not trained to use them well.
And there’s another problem: technology. Some tools are web-based or app-only. Older patients, or those without reliable internet, can’t access them. One survey found 23% of negative reviews mentioned difficulty logging in or using the tool.
But adoption is growing. The VA uses decision aids in 68% of mental health clinics. Medicare Advantage plans are now required to offer shared decision-making for high-cost drugs. That’s pushing more systems to invest. Training programs exist. After 4 hours of practice, 87% of clinicians report feeling confident using them.
What do patients really say?
Most patients who’ve used decision aids say they feel more in control. A VA survey of 1,250 veterans showed 78% felt more confident after using one. One woman switched from warfarin to a newer blood thinner after seeing the bleeding risk drop from 8 in 100 to 3 in 100. “I didn’t know it was that big a difference,” she said.
Others used the tool to say no. A man with depression was offered a new antidepressant with a 1 in 5 chance of sexual side effects. He’d been struggling with that before. The decision aid showed him the odds. He chose to stay on his old medication. “It gave me permission to pick what worked for me,” he told his doctor.
But not everyone had a good experience. Some said the tools gave false equivalence-making two drugs look equally good when one had much stronger evidence. Others felt flooded with numbers. One Mayo Clinic user said, “It was like being handed a spreadsheet at 8 a.m.”
What’s next for decision aids?
The future is personalization. Intermountain Healthcare launched an AI tool in early 2024 that adapts the information based on how you learn. If you respond better to pictures, it shows more icons. If you prefer numbers, it highlights stats. It even adjusts for your health literacy level.
The FDA is also stepping in. In 2024, they proposed new rules requiring decision aids to be tested on diverse patients to make sure they’re truly understandable. No more vague language. No more hiding risks.
Still, challenges remain. Only 38% of hospitals have money set aside to update these tools as new drugs come out. A decision aid that’s accurate today might be outdated in 18 months. That’s why experts warn: tools must be living documents, not static PDFs.
How to ask for a decision aid
You don’t have to wait for your doctor to offer one. If you’re thinking about switching meds, say this:
- “I’ve heard about decision aids. Do you have one for this switch?”
- “Can we go over the real chances of side effects-not just ‘some people’ get them?”
- “What matters most to you when you recommend a switch?”
Ask to use the tool before your appointment. Many are available online. Print it out or bring your phone. Bring someone with you if you’re overwhelmed.
Remember: your doctor doesn’t know what you fear. Maybe it’s weight gain. Maybe it’s drowsiness. Maybe it’s cost. Decision aids help you say it out loud-and help your doctor hear you.
Final thought: It’s your body, your choice
Medication switching isn’t just science. It’s personal. What works for one person might ruin another’s life. Decision aids don’t make the choice for you. They just give you the tools to make it with your eyes open. You deserve that.
What is a decision aid for switching medications?
A decision aid is a structured tool that helps patients and doctors make informed choices about switching medications. It presents clear, balanced information on the benefits and risks of each option, uses visual aids like icon arrays to show probabilities, and includes exercises to help patients identify what matters most to them-like side effects, cost, or dosing schedule.
Are decision aids proven to work?
Yes. Multiple studies, including a Cochrane review of over 100 trials, show patients who use decision aids understand their options better, feel less conflicted, and are more likely to stick with their chosen treatment. They score 15-25% higher on knowledge tests compared to those who only receive verbal advice.
Can decision aids help me avoid bad side effects?
They can. By showing you the actual likelihood of side effects-like weight gain, dizziness, or bleeding-decision aids let you weigh what you’re willing to accept. One patient declined a switch after seeing a 30% chance of sexual side effects, which he had previously found unbearable. The tool gave him the data to say no confidently.
Why don’t all doctors use decision aids?
Mainly because they take time-7 to 12 extra minutes per visit-and many doctors aren’t trained to use them. Some tools are digital and hard for older or low-tech patients to access. But adoption is growing, especially in VA hospitals and Medicare Advantage plans, where shared decision-making is now required.
Where can I find a reliable decision aid?
Trusted sources include the Ottawa Hospital Research Institute’s decision aid library, the VA’s MIRECC program, and Mayo Clinic’s patient resources. These are evidence-based, regularly updated, and designed for real-world use. Avoid tools from drug companies-they often focus only on benefits and downplay risks.





Keasha Trawick
December 14, 2025 AT 03:47Okay, but let’s be real-decision aids are the only thing that stopped me from taking that SSRI that turned me into a zombie with a side of libido annihilation. The icon array showing 1 in 3 people getting sexual dysfunction? That’s not a ‘maybe,’ that’s a red flag waving like a flag at a NASCAR race. I walked out of that appointment with my old med and a newfound respect for data over vibes.
Tommy Watson
December 14, 2025 AT 22:51lol doctors dont wanna use these cause they gotta think. why not just tell me what to do like my grandpa used to? ‘take the blue pill, son.’ simple. now i got spreadsheets and icons and i still dont know if i’m gonna live or die.
sharon soila
December 16, 2025 AT 17:07You are not alone in feeling overwhelmed. Every person deserves clarity, not confusion. Decision aids are not about numbers-they are about dignity. They give you the power to say, ‘This is my body, and I choose with understanding.’ That is not a luxury. It is a right.
Constantine Vigderman
December 16, 2025 AT 21:56OMG YES!!! I used the VA’s tool for my blood thinner switch and it literally changed my life 😭 The bleeding risk went from 8/100 to 3/100-I cried. My doc was like ‘uh… you good?’ and I was like ‘I’m FINE, I just realized I’m not gonna bleed out.’ 🙌 #DecisionAidHero
Cole Newman
December 17, 2025 AT 05:07you guys are overcomplicating this. if your doc says switch, switch. they went to med school. you went to tiktok. stop making it a democracy. also, 20% risk reduction doesn’t mean you’re safe-duh. why are we even talking?
kevin moranga
December 18, 2025 AT 21:53I know this sounds like a lot, but hear me out-you’ve been carrying this weight alone, and you don’t have to anymore. Decision aids aren’t just tools, they’re bridges. They help you speak your truth to your doctor without fear. I used one when I was terrified to say no to a new antidepressant. I told them I couldn’t handle sexual side effects again. They didn’t push. They listened. And I stayed on my old med-and I’ve slept through the night for the first time in years. You’re not weak for wanting to understand. You’re brave.
Jamie Clark
December 20, 2025 AT 20:42This is what happens when you let patients make medical decisions. You get people rejecting proven treatments because they saw a pretty icon chart. Medicine isn’t a customer survey. It’s science. If you can’t handle a 12% chance of nausea, maybe you shouldn’t be on medication at all. Stop romanticizing ignorance.
Bruno Janssen
December 21, 2025 AT 19:34I read all this. I didn’t say anything. I just stared at the screen. The numbers looked like ghosts. I still took the pill. I still feel nothing.
Scott Butler
December 23, 2025 AT 02:51Why are we letting Americans turn medicine into a TikTok trend? In my country, doctors decide. Patients take the pill. No icons. No surveys. No emotional hand-holding. This is why our healthcare is efficient. You want to live? Shut up and swallow.