Warfarin and NSAIDs Bleeding Risk Calculator
This tool estimates your increased risk of serious bleeding when taking warfarin with NSAIDs based on your specific factors. Please note: This is a risk assessment tool, not a medical diagnosis. Always consult your doctor before changing medications.
Risk Assessment Factors
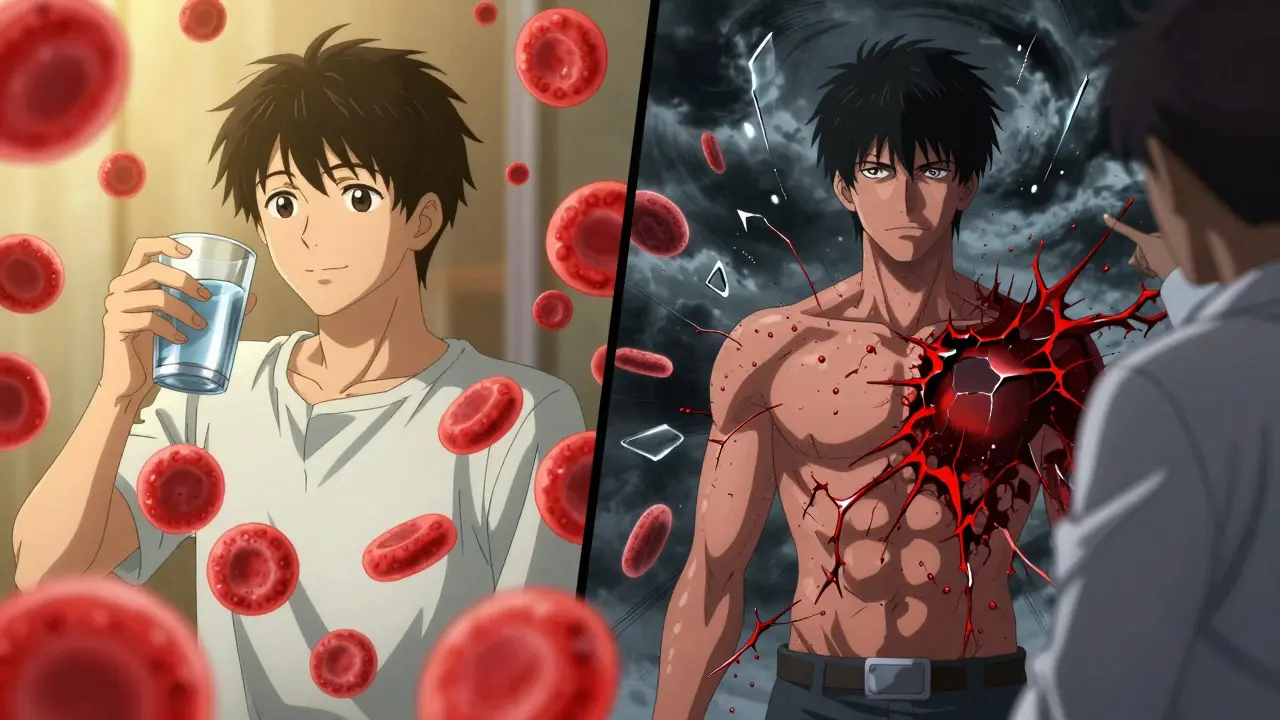
Every year, millions of people take warfarin to prevent dangerous blood clots - often because of atrial fibrillation, a replaced heart valve, or a past deep vein thrombosis. At the same time, countless others reach for ibuprofen, naproxen, or diclofenac for a sore back, a headache, or arthritic knees. What most don’t realize is that combining these two types of medication can turn a simple pain reliever into a silent threat. The result? A sharply increased chance of serious, sometimes deadly, bleeding.
Why This Combination Is So Dangerous
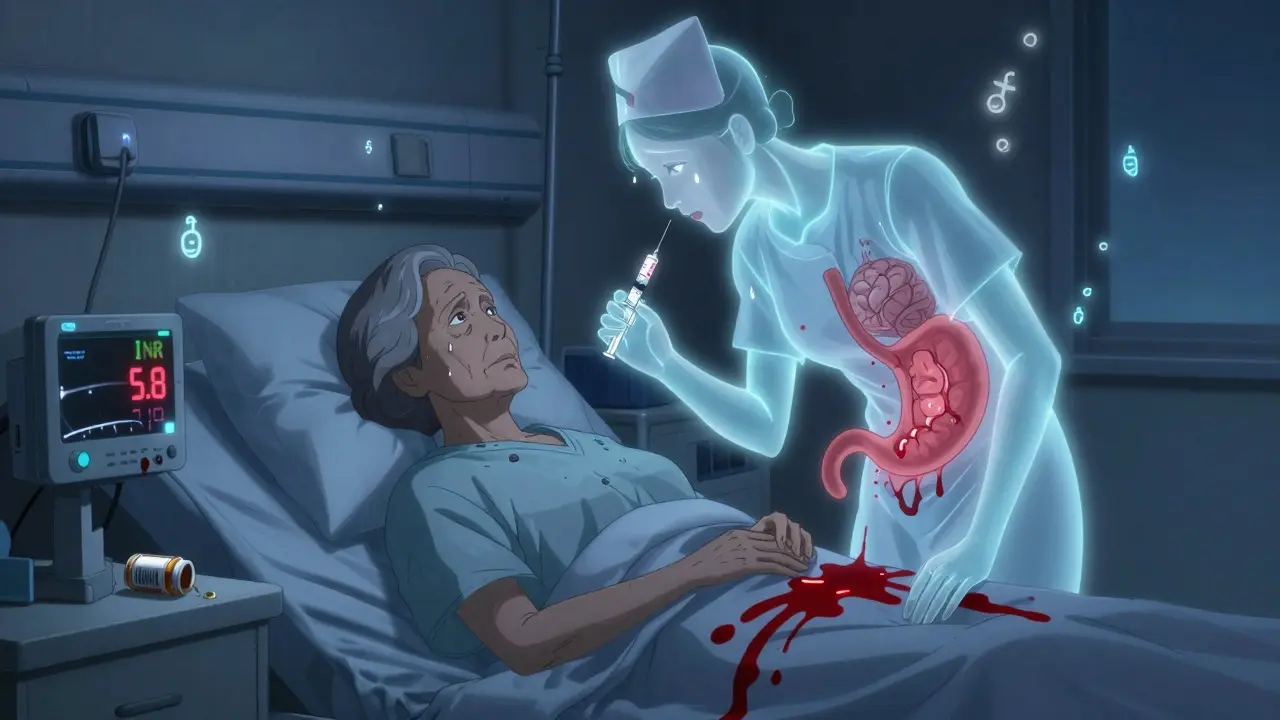
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. Without enough of those factors, your blood takes longer to clot - that’s the goal. But NSAIDs do something different. They shut down cyclooxygenase enzymes, which not only reduces inflammation and pain but also messes with platelets - the tiny blood cells that plug leaks in damaged vessels. On top of that, NSAIDs wear down the protective lining of your stomach, making it easier for ulcers to form and bleed.When you take both, you’re hitting the clotting system from two sides: warfarin slows down the chemical cascade that forms clots, and NSAIDs disable the physical repair crew (platelets) while weakening the walls of your blood vessels. It’s not just additive - it’s multiplicative. A 2023 study from Aarhus University Hospital found that people on warfarin who took NSAIDs had more than double the risk of bleeding compared to those on warfarin alone.
Not All NSAIDs Are Created Equal
You might think all over-the-counter painkillers are equally risky, but they’re not. The danger varies by drug:- Naproxen - highest risk: 4.1 times greater bleeding than warfarin alone
- Diclofenac - 3.3 times higher risk
- Ibuprofen - still dangerous: 1.79 times higher risk
- Meloxicam - especially risky in patients on high-dose warfarin
Even drugs marketed as "gentler" on the stomach - like celecoxib (a COX-2 inhibitor) - don’t offer safety. A 2020 meta-analysis showed they increase gastrointestinal bleeding risk by nearly 2-fold, just like traditional NSAIDs. The idea that selective COX-2 drugs are safer with anticoagulants is a myth.
Where Bleeding Happens - And How Bad It Gets
Bleeding isn’t just a nosebleed or a bruise. With warfarin and NSAIDs together, the risks turn serious:- Gastrointestinal bleeding - 2.24 times more likely. This is the most common, accounting for over 60% of cases in hospital records.
- Intracranial bleeding - 3.22 times higher risk. A bleed in the brain can be fatal or cause permanent disability.
- Urinary tract bleeding - 1.57 times more common, sometimes mistaken for a UTI or kidney stone.
- Pulmonary bleeding - less frequent but still 36% more likely, leading to coughing up blood.
Real-world data from the FDA’s adverse event database shows 1,842 bleeding events linked to this combo between 2015 and 2020. Nearly 80% of patients who bled while taking both drugs ended up hospitalized. One Reddit user shared: "Took ibuprofen for a headache. My hemoglobin dropped from 14 to 8 in 24 hours. ER visit. Transfusion. I was lucky I didn’t die."
NOACs Aren’t a Safe Alternative
Many patients assume switching from warfarin to a newer anticoagulant like apixaban, rivaroxaban, or dabigatran makes them safe to take NSAIDs. That’s a dangerous misunderstanding.Studies show NSAIDs increase bleeding risk with all oral anticoagulants. The ARISTOTLE trial found apixaban users on NSAIDs still had significantly higher bleeding rates than those not taking them. While some data suggests dabigatran might carry slightly less risk than warfarin when combined with NSAIDs, the difference is small - and nowhere near safe. A 2023 study in Circulation: Cardiovascular Quality and Outcomes found that while warfarin-NSAID co-prescribing dropped by 27% between 2015 and 2022, NSAID use with NOACs actually rose by 35%. People think they’re safer - but they’re not.
Who’s at Highest Risk?
Some people are far more vulnerable:- Those on high-dose warfarin (>40 mg/week)
- People with low baseline INR (meaning their blood clots too easily before the NSAID is added)
- Patients over 75 - they face 3.7 times higher bleeding risk than younger users
- Anyone taking other medications that affect bleeding - like SSRIs, aspirin, or corticosteroids
A 2010 study of 98 warfarin users found that 40% saw their INR jump by 15% or more after adding an NSAID. That’s enough to push someone from a safe range (INR 2-3) into dangerous territory (INR 5+), where spontaneous bleeding becomes a real threat.
What Should You Do Instead?
The best solution? Avoid NSAIDs entirely if you’re on warfarin or any other anticoagulant. Here’s what works better:- Acetaminophen (paracetamol) - the top alternative. Used by 23.5% of warfarin patients. It doesn’t affect platelets or the stomach lining. Stick to 3,000 mg/day max to avoid liver damage.
- Topical pain relievers - gels and patches with menthol, capsaicin, or diclofenac (applied to skin, not swallowed). These have minimal systemic absorption and are much safer.
- Physical therapy, heat/cold therapy, or acupuncture - for chronic pain like arthritis. No drugs needed.
- Low-dose, short-term NSAID use only if absolutely necessary - and only under close medical supervision.
What to Do If You Must Take an NSAID
Sometimes, pain is too severe to avoid. If your doctor agrees you need an NSAID for a few days:- Choose the lowest possible dose - ibuprofen 200 mg once daily, not 400 mg twice.
- Avoid naproxen, diclofenac, and meloxicam. If you must use one, ibuprofen is the least risky.
- Get your INR checked 3-5 days after starting the NSAID - and again weekly while taking it.
- Ask for a proton pump inhibitor (like omeprazole) to protect your stomach.
- Tell every doctor, pharmacist, and ER staff you’re on warfarin - even if you’re just picking up a cold medicine.
- Know the warning signs: unusual bruising, blood in stool or urine, black tarry stools, severe headaches, dizziness, vomiting blood.
Many patients don’t realize that even a single dose of an OTC NSAID can trigger a dangerous INR spike. A 2021 University of Michigan study found that in 68% of warfarin-related bleeding cases, the patient hadn’t told their doctor they were taking ibuprofen or naproxen.
Why This Problem Persists
Despite decades of warnings, this interaction is still common. Why?- Patients don’t think OTC drugs "count" as medications.
- Many NSAID labels only say "may increase bleeding risk" - no mention of warfarin.
- Electronic health records in 42% of U.S. hospitals still don’t flag this combo.
- Doctors sometimes assume the patient already knows, or they forget to check.
The economic cost is staggering: $1.87 billion a year in the U.S. alone for hospital stays, transfusions, and emergency care. And it’s preventable.
The Bottom Line
There is no safe way to combine warfarin and NSAIDs. The risk isn’t theoretical - it’s proven, documented, and deadly. Even short-term use can cause major bleeding. Acetaminophen is your best friend. Topical treatments are your next best option. If you’re on warfarin, treat NSAIDs like you would a loaded gun: keep them far away unless you’re prepared for serious consequences.Don’t assume your doctor knows you’re taking ibuprofen. Don’t assume your pharmacist will catch it. Don’t assume it’s "just one pill." Your blood is thin - don’t let a painkiller make it thinner.
Can I take ibuprofen with warfarin if I only use it once in a while?
No. Even a single dose of ibuprofen can raise your INR and increase bleeding risk. Studies show a spike in INR within 2-3 days of starting even low-dose ibuprofen. The risk isn’t about frequency - it’s about the drug’s effect on platelets and stomach lining. Acetaminophen is the only safe OTC pain reliever for people on warfarin.
Is naproxen worse than ibuprofen with warfarin?
Yes, significantly. Naproxen increases bleeding risk 4.1 times compared to warfarin alone, while ibuprofen increases it 1.79 times. Naproxen also has a longer half-life, meaning it stays in your system longer and continues to interfere with clotting. It’s one of the most dangerous NSAIDs to combine with warfarin.
Do newer blood thinners like Eliquis or Xarelto have fewer interactions with NSAIDs?
No. While NOACs like apixaban and rivaroxaban don’t interact with vitamin K or require regular INR checks, they still carry a high bleeding risk when combined with NSAIDs. Studies confirm NSAIDs increase bleeding risk with all oral anticoagulants - the mechanism is different, but the outcome is just as dangerous. Don’t assume switching anticoagulants gives you permission to use NSAIDs.
What should I do if I accidentally took ibuprofen while on warfarin?
Stop taking the NSAID immediately. Contact your anticoagulation clinic or doctor within 24 hours to get your INR checked. Watch for signs of bleeding: unusual bruising, dark stools, blood in urine, severe headache, dizziness, or vomiting blood. If any of these occur, go to the ER. Don’t wait - bleeding can escalate quickly.
Can I use topical NSAIDs like Voltaren gel with warfarin?
Yes, topical NSAIDs like diclofenac gel are generally safe with warfarin. Only about 6% of the drug gets absorbed into your bloodstream, which is not enough to affect platelets or INR significantly. They’re a good option for localized pain like arthritis in the knee or elbow. But avoid applying them over large areas or under occlusive dressings - that can increase absorption.
How often should I check my INR if I’m on warfarin and need pain relief?
If you must take an NSAID - and you shouldn’t - get your INR checked 3-5 days after starting it, then weekly while taking it. After stopping the NSAID, check INR again in 3-5 days, since levels can drop back down. Never assume your INR is stable if you’ve added or changed any medication, even something you bought over the counter.
For anyone on warfarin, the message is clear: pain relief doesn’t have to come at the cost of your safety. There are safer options. Use them.







Skye Kooyman
January 25, 2026 AT 23:11Just took ibuprofen for my headache yesterday. Still alive. Probably fine.
Karen Droege
January 27, 2026 AT 02:33This is one of the most important public health warnings I've seen in years. I'm a pharmacist in Vancouver and I've seen patients bleed out from 'just one pill.' The myth that OTC means 'safe with everything' is lethal. I hand out printed flyers in the anticoagulation clinic. Every. Single. Day. Acetaminophen isn't perfect, but it's the only OTC option that doesn't turn your blood into tap water. Topical diclofenac gel? Game-changer for knee arthritis. And yes, NOACs are NOT safer. Stop believing marketing. This isn't a suggestion-it's a survival guide.
Peter Sharplin
January 28, 2026 AT 03:44As a nurse who works in cardiology, I've had to explain this to dozens of patients. The worst case? A 78-year-old man who took naproxen for his back pain, didn't tell his doctor, and ended up with a subdural hematoma. He survived, but lost 30% of his vision. He didn't even know NSAIDs could do that. The real tragedy? This is 100% preventable. If you're on warfarin, treat ibuprofen like it's cyanide. Not because it's scary-it's because it's predictable. Acetaminophen works. Topical creams work. Ice packs work. Don't gamble with your clotting system. Your body doesn't have a reset button.
Kipper Pickens
January 28, 2026 AT 11:43From a clinical pharmacology standpoint, the pharmacokinetic interaction is secondary to the pharmacodynamic synergy. Warfarin inhibits VKORC1, reducing functional vitamin K-dependent coagulation factors (II, VII, IX, X). NSAIDs inhibit COX-1, suppressing thromboxane A2 synthesis in platelets, impairing aggregation. Concurrent use creates a dual-hit hemostatic failure. The GI mucosal damage from NSAIDs further exacerbates this by creating a physical breach in vascular integrity. The Aarhus study's OR of 2.1 is conservative-real-world data from the FDA FAERS shows a 3.2-fold increase in major bleeding events when controlling for age and INR variability. The COX-2 inhibitor myth persists due to cognitive bias in patient education materials. Bottom line: no NSAID is safe with any anticoagulant. Period.
Faisal Mohamed
January 29, 2026 AT 08:35We live in a world where pain is treated as a moral failing. You're not weak if you can't endure discomfort-you're human. But we've been conditioned to swallow solutions without asking what they're doing to our biology. Warfarin isn't just a drug-it's a surrender to the inevitability of clotting. NSAIDs are the rebellion against that surrender. But rebellion without wisdom is suicide. The real question isn't 'can I take ibuprofen?' It's 'why do I feel I must?' Maybe the answer isn't in a pill, but in a massage, in stillness, in listening to your body instead of silencing it. The body doesn't lie. The pharmaceutical industry does.
eric fert
January 30, 2026 AT 20:46Let’s be real-this whole thing is fearmongering dressed up as medical advice. I’ve been on warfarin for 12 years. I take ibuprofen every other weekend for my gym soreness. My INR? Stable. My doctor? Says I’m fine. Meanwhile, you people are acting like one pill is going to turn you into a human blood fountain. Where’s the data on the millions who do this without incident? You’re ignoring the actual risk profile. The real danger is anxiety-induced overtesting and unnecessary drug avoidance. Acetaminophen isn’t harmless either-liver failure is a thing. And don’t get me started on how many people die from falling because they’re too scared to take pain meds and end up breaking their hip. This post reads like a PSA written by someone who’s never met a real patient. Chill out. Your blood isn’t that thin.
Allie Lehto
February 1, 2026 AT 12:31why do people keep thinking they know better than doctors?? i took naproxen for 3 days last month and my INR went to 6.7. i was in the er for 12 hours. i had black stools and thought it was just my diet. i’m so mad at myself. i thought it was ‘just a little’ and now i’m terrified to take anything. why is this not on the bottle?? why?? i feel so stupid. i’m not even mad at the drug, i’m mad at the system. nobody warned me. nobody. and now i’m scared to even take tylenol. what if that’s bad too??
Rakesh Kakkad
February 2, 2026 AT 16:45As a physician practicing in Mumbai, I have seen this exact scenario repeat itself with alarming frequency. Patients, particularly those with atrial fibrillation post-valve replacement, self-medicate with NSAIDs due to cultural norms around pain tolerance and limited access to specialist care. The problem is compounded by the widespread belief that 'Western medicine' is inherently dangerous, leading to reliance on unregulated herbal alternatives that may interact unpredictably. This post is not alarmist-it is a necessary intervention. The solution lies not only in patient education but in integrating pharmacovigilance into primary care workflows. We need community health workers trained to flag these interactions during home visits. The cost of inaction is measured not in dollars, but in lives lost before their time.
Suresh Kumar Govindan
February 4, 2026 AT 14:49Did you know that 92% of NSAID labels in the U.S. omit any mention of anticoagulants? This is not negligence-it’s corporate design. The FDA has known since 1998. The pharmaceutical industry profits from chronic use, not patient safety. The fact that NOAC usage increased alongside NSAID use by 35%? That’s not a coincidence. That’s a calculated shift in marketing. They replaced warfarin with a more expensive drug and kept the same deadly combo. The real conspiracy? They want you to believe you’re safer now. You’re not. You’re just paying more to die the same way.
Simran Kaur
February 4, 2026 AT 22:21I’m from Delhi and my mom has AFib and takes warfarin. She used to take diclofenac for her knees. I found this article and showed it to her in Hindi. She cried. Not because she was scared-but because she realized she’d been risking her life for years thinking she was being careful. We switched to topical gel and heat packs. Her pain is still there, but she’s alive. I wish every family had access to this kind of clear, compassionate info. Thank you for writing this. Not everyone in India has a doctor they trust. This is the kind of thing that saves lives when the system fails.
Dan Nichols
February 6, 2026 AT 02:31You're all missing the point. The real issue is that doctors are lazy. If they spent 2 minutes explaining this to patients instead of writing a script, none of this would happen. Also, acetaminophen isn't a magic bullet-it's hepatotoxic at high doses. So now you're trading GI bleeding for liver failure? Brilliant. And what about patients with chronic pain who need daily relief? Are they just supposed to suffer? This post reads like a pamphlet from a medical school that never treated a real patient with arthritis. There's nuance. There's context. There's individual risk. You're reducing complex clinical decisions to a fear-based meme. That's not helpful. That's dangerous too.
Renia Pyles
February 7, 2026 AT 03:16Wow. So I’m just supposed to suffer through my arthritis pain because some guy on the internet says ibuprofen might kill me? What if I can’t walk? What if I can’t work? What if I’m 65 and my only relief is a pill I’ve taken for 20 years? You’re not a doctor. You’re not my mom. You’re not even real. This post is emotional terrorism. I’ve had my INR checked every week for 8 years. I know my numbers. I know my body. I don’t need a Reddit sermon. I need pain relief. And I’m taking it. If I die? Fine. But don’t act like your fear is a moral victory.