When you’ve been on a biologic drug for years-maybe infliximab or adalimumab-to manage rheumatoid arthritis, Crohn’s disease, or psoriasis, your body knows it. You’ve found the right dose. You’ve settled into a routine. Then your doctor says: we’re switching you to a biosimilar. It’s cheaper. It’s approved. It’s the same. But is it?
What exactly is a biosimilar?
A biosimilar isn’t a generic. That’s the first thing to understand. Generics are exact copies of small-molecule drugs, like aspirin or metformin. Biosimilars are copies of biological drugs-complex proteins made from living cells. Think of it like trying to recreate a handmade quilt. You can match the pattern, the thread, even the stitching. But no two quilts are identical. That’s why biosimilars are highly similar, not identical.The U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) require biosimilars to go through rigorous testing. They must show no clinically meaningful differences in safety, purity, or potency compared to the original biologic. That means if you’re stable on Humira (adalimumab), switching to its biosimilar-say, Cyltezo or Adalimumab-adbm-shouldn’t change how you feel or how well your disease is controlled.
The first biosimilar approved in the U.S. was Zarxio (filgrastim-sndz) in 2015. Since then, 37 biosimilars have been approved, mostly targeting tumor necrosis factor (TNF) inhibitors. These are the most common biologics used for autoimmune diseases. By 2022, about 70% of all biosimilar use in the U.S. was for TNF blockers like infliximab and adalimumab.
What happens when you switch?
Switching can happen for two reasons: medical or non-medical. Medical switching means your doctor changes your drug because your current one isn’t working well enough. Non-medical switching is when the change is made for cost reasons-your insurer wants to save money, or your hospital is pushing for budget efficiency.Studies show that in medical switching, patients do just fine. The NOR-Switch study, which tracked 481 patients with inflammatory arthritis or IBD, found that switching from originator infliximab to its biosimilar CT-P13 resulted in similar retention rates: 60% stayed on the originator, 52.6% stayed on the biosimilar after a year. The difference wasn’t statistically significant.
In real-world settings, over 85% of patients stay on their new biosimilar after 12 months. That’s a strong signal that most people adapt without issue. A 2021 study in inflammatory bowel disease patients switching from CT-P13 to another biosimilar, SB2, showed 90.6% maintained remission. Fecal calprotectin levels-a marker of gut inflammation-stayed nearly identical before and after the switch.
Even when patients switch between biosimilars, the data holds up. A 2020 study in 100 patients who switched from one biosimilar to another (SB4 to GP2015) found 90% retained response. Trough levels-the amount of drug in your blood-remained stable. Immunogenicity (the body making antibodies against the drug) stayed low: only about 3 cases per 100 patient-years across multiple switches.
Why do some people stop?
Not everyone has a smooth transition. About 4% to 18% of patients discontinue after a non-medical switch. But here’s the key: most of those drops aren’t because the drug stopped working.A 2021 study in Frontiers in Psychology found that 32.7% of patients reported new or worsening symptoms after switching-even when lab tests showed no change in disease activity. This is called the nocebo effect. It’s the opposite of the placebo effect. If you believe a cheaper drug won’t work as well, your brain can make you feel worse.
Reddit threads from patients with rheumatoid arthritis tell the same story. One user wrote: “I felt like I was back to square one after the switch. My joints ached. I was exhausted. My doctor said my bloodwork was fine. But I didn’t feel fine.” That’s not a failure of the biosimilar. That’s the power of perception.
Other reasons for stopping include injection-site reactions (7.8% in some adalimumab biosimilar studies) or a perceived loss of control. When patients aren’t involved in the decision, they’re more likely to discontinue. A 2023 study called PERFUSE showed that when doctors spent 20+ minutes explaining the switch, offering shared decision-making tools, and scheduling follow-ups, discontinuation dropped from 18% to just 6.4%.

Is it safe?
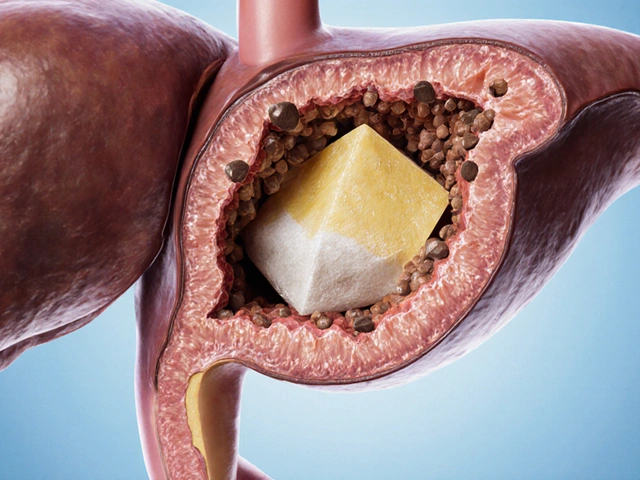
The short answer: yes. The FDA analyzed 22 switching studies involving over 5,700 patients and found no increased risk of death, serious side effects, or treatment discontinuation. The EMA’s 2022 position paper concluded: “Switching between reference medicine and biosimilar… is not expected to compromise safety or efficacy.”Immunogenicity is the biggest concern. Biologics can trigger your immune system to make anti-drug antibodies. That can make the drug less effective-or cause allergic reactions. But data shows biosimilars don’t increase this risk. In a 2022 study of 140 patients who switched from originator infliximab to CT-P13, then to SB2, immunogenicity rates were unchanged. Trough levels stayed steady at around 4.1-4.3 μg/mL.
Even in high-risk groups like inflammatory bowel disease, switching doesn’t appear to trigger flares. A 2023 report from the Center for Biosimilars noted that while 9.4% of IBD patients stopped after a biosimilar-to-biosimilar switch, the reason was rarely confirmed immunogenicity. Most were attributed to patient anxiety or coincidental disease activity.
Cost and access
Biosimilars cost 15% to 35% less than originators. When Humira biosimilars launched in the U.S. in 2023, they entered the market at a 35% discount. That’s billions saved for insurers, hospitals, and taxpayers.By 2023, 85% of U.S. health plans had mandatory switch policies for biologics. In Europe, biosimilar adoption is even higher-67% of filgrastim prescriptions are for biosimilars. But in the U.S., uptake lags because of complex rebate systems and patent protections that delay competition.
That’s changing. In 2024, the FDA approved the first interchangeable adalimumab biosimilar, Cyltezo. That means pharmacists can substitute it for Humira without needing a new prescription. This is a game-changer. It’s like switching from brand-name Advil to generic ibuprofen-but for complex biologics.

Who should avoid switching?
Switching isn’t right for everyone. Experts agree it’s safest for patients with stable, low-activity disease. If your DAS28 score (a measure of rheumatoid arthritis activity) is below 3.2, you’re a good candidate. If your Crohn’s disease is in deep remission, with normal calprotectin and no recent hospitalizations, switching is low-risk.But if you’re actively flaring, recently changed doses, or have had multiple drug failures, hold off. The Arthritis Foundation warns against switching during unstable periods. Case reports in the FDA’s adverse event database show rare flare-ups after switches-but these are outliers, not trends.
Also, avoid multiple switches. While switching once is safe, switching three or four times in a short time increases uncertainty. There’s no data yet on long-term effects of repeated switches. Stick to one biosimilar unless there’s a clear medical reason to change again.
What should you do if you’re being switched?
You don’t have to accept a switch silently. Here’s what works:- Ask why. Is this a cost decision? Or is your current drug failing? Know the reason.
- Ask for time. Request a 20-30 minute appointment to discuss. Bring a list of questions.
- Ask for data. “What studies show this switch is safe for someone like me?”
- Ask for monitoring. Request follow-up blood tests at 3 months. Check your disease activity score and drug levels.
- Speak up if you feel different. Don’t wait. Report new symptoms-even if you think it’s “all in your head.”
Most patients who switch with support do fine. The DANBIO registry surveyed 1,200 patients who switched to infliximab biosimilars. 68% reported no issues. The rest? Many were reassured after a few weeks. Their symptoms improved as their anxiety faded.
What’s next?
The biosimilar market is growing fast-projected to hit $100 billion by 2030. More biologics are coming off patent. By 2025, over $178 billion in biologic sales will be up for competition.That means more choices. More savings. More access for patients who couldn’t afford these drugs before.
But the real win isn’t just cost. It’s control. When patients are included in the decision, when they understand the science, when they’re monitored closely-they feel safer. And that’s what matters most.




Hannah Gliane
February 2, 2026 AT 06:39Murarikar Satishwar
February 3, 2026 AT 20:50Dan Pearson
February 5, 2026 AT 08:00Nick Flake
February 5, 2026 AT 08:49Brett MacDonald
February 7, 2026 AT 03:48Sandeep Kumar
February 8, 2026 AT 17:26Gary Mitts
February 9, 2026 AT 00:57clarissa sulio
February 9, 2026 AT 03:00Bridget Molokomme
February 10, 2026 AT 02:41Vatsal Srivastava
February 10, 2026 AT 22:25Brittany Marioni
February 12, 2026 AT 07:09Monica Slypig
February 14, 2026 AT 00:18Becky M.
February 14, 2026 AT 14:40