When you’re prescribed a combo pill that mixes Olmesartan/Amlodipine is a fixed‑dose antihypertensive that pairs an angiotensin II receptor blocker (ARB) with a calcium‑channel blocker (CCB), it feels like a shortcut to lower blood pressure. The shortcut works, but only if you know what else in your diet or medicine cabinet can throw the mix off balance. Below you’ll find the most common interactions, practical tips, and red‑flag signs that tell you to call your pharmacist or doctor.
Quick Takeaways
- Olmesartan and amlodipine are metabolized differently, so they don’t usually “fight” each other.
- Potassium‑rich supplements, NSAIDs, and strong CYP3A4 inhibitors can raise the risk of low blood pressure or kidney strain.
- Grapefruit juice can boost amlodipine levels, leading to dizziness or swelling.
- Always tell your clinician about over‑the‑counter meds, herbal products, and any changes in diet.
- Know the warning signs: sudden faintness, rapid weight gain, or a persistent cough.
What Is Olmesartan/Amlodipine?
The combination pill is designed for adults with moderate to severe hypertension who need two mechanisms of action in one tablet. Olmesartan blocks the angiotensin II receptor, preventing blood vessels from tightening. Amlodipine relaxes smooth muscle in arterial walls by inhibiting calcium influx, which widens the vessels. The result is a steadier, lower blood pressure with fewer pills to remember.
How Each Component Is Processed in the Body
- Olmesartan - absorbed in the small intestine, reaches peak plasma concentration in 1-2 hours, and is excreted largely unchanged via the kidneys. Its half‑life is about 13 hours.
- Amlodipine - highly lipophilic, it binds to plasma proteins, and is metabolized by the liver enzyme CYP3A4. Peak levels appear in 6-12 hours, and the drug hangs around for up to 50 hours.
Because the two drugs follow separate pathways, most direct drug‑to‑drug clashes are rare. The real risks come from other agents that share the same elimination routes or that amplify the blood‑pressure‑lowering effect.
Common Interaction Categories
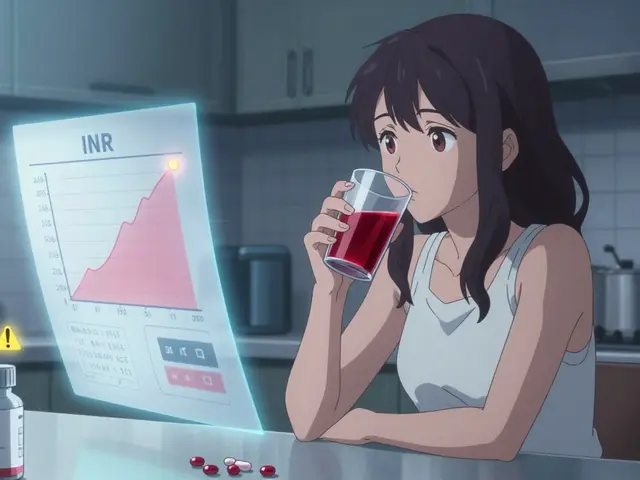
| Interaction | Typical Effect | Severity |
|---|---|---|
| Potassium‑sparing diuretics (e.g., spironolactone) | Increase serum potassium → hyperkalemia | Major |
| Non‑steroidal anti‑inflammatory drugs (NSAIDs) | Reduced renal perfusion → possible AKI | Moderate |
| Strong CYP3A4 inhibitors (ketoconazole, clarithromycin) | Amlodipine levels rise → excessive vasodilation | Moderate |
| Grapefruit juice | Inhibits CYP3A4 → higher amlodipine exposure | Minor‑to‑Moderate |
| ACE inhibitors or other ARBs | Duplicate renin‑angiotensin blockade → hypotension | Major |
| Lithium | Olmesartan reduces renal clearance → lithium toxicity | Major |
| Alcohol (large amounts) | Additive blood‑pressure drop | Minor |
Foods & Beverages That Matter
Most meals won’t interfere, but a few items sit on the same metabolic “highway” as amlodipine.
- Grapefruit and Seville oranges - contain furanocoumarins that block CYP3A4 in the gut. Even a single glass of grapefruit juice can lift amlodipine concentrations by up to 25 %.
- High‑potassium foods (bananas, avocado, spinach) - when you’re also using a potassium‑sparing diuretic, watch your serum potassium labs.
- Salt‑rich dishes - excess sodium counteracts the blood‑pressure‑lowering effect, making you think the combo isn’t working.

Prescription and Over‑the‑Counter Meds to Watch
Below is a quick rundown of drug classes that clinicians usually flag when you’re on Olmesartan/Amlodipine.
- Potassium‑sparing diuretics (e.g., spironolactone, triamterene) - monitor K+ every 1-2 weeks.
- NSAIDs (ibuprofen, naproxen) - use the lowest effective dose, stay hydrated, and consider alternating with acetaminophen.
- CYP3A4 inhibitors (ketoconazole, erythromycin, grapefruit supplements) - either avoid or adjust amlodipine dose under medical supervision.
- Lithium - check lithium serum levels within a week of starting or stopping Olmesartan.
- Other renin‑angiotensin drugs (ACE inhibitors, other ARBs) - concurrent use dramatically raises hypotension risk.
- Diabetes medications (e.g., thiazolidinediones) - may increase fluid retention, counteracting amlodipine’s peripheral edema benefit.
Practical Tips for Managing Interaction Risk
- Keep an up‑to‑date medication list. Write down every prescription, OTC, herb, and supplement. Review it with your pharmacist quarterly.
- Space out doses when possible. If you need an NSAID, take it at least 2 hours after your blood‑pressure pill to lessen kidney stress.
- Watch your labs. Baseline kidney function (eGFR), electrolytes, and lithium levels should be checked within 2 weeks of starting the combo, then every 3-6 months.
- Stay hydrated. Dehydration amplifies the blood‑pressure‑lowering effect of both agents, especially when combined with diuretics.
- Limit grapefruit. If you love it, discuss a possible dose reduction with your clinician rather than quitting cold turkey.
- Report side effects early. Light‑headedness, swelling of the ankles, or a new cough should trigger a call.
Red‑Flag Symptoms That Require Immediate Attention
- Severe dizziness or fainting - could mean dangerous hypotension.
- Sudden swelling in the legs, feet, or face - may signal fluid overload from a drug interaction.
- Persistent dry cough - could indicate a concurrent ACE inhibitor that was added unintentionally.
- Muscle weakness, irregular heartbeat, or palpitations - watch for hyperkalemia.
- Reduced urine output, nausea, or flank pain - possible acute kidney injury.
Checklist Before You Fill the Prescription
- Have you listed all current meds, including vitamins and herbs?
- Is your kidney function normal (eGFR >60 mL/min/1.73 m²)?
- Do you take any NSAIDs more than twice a week?
- Do you drink grapefruit juice daily?
- Is your potassium intake within the recommended 2,500‑3,000 mg/day?
- Do you have a blood‑pressure reading target set by your doctor?
- Do you know the phone number of your pharmacy’s clinical team?
Bottom Line
Olmesartan/Amlodipine is a powerful partnership for tackling high blood pressure, but its safety hinges on what you eat and the other drugs you take. By staying vigilant about potassium, avoiding strong CYP3A4 inhibitors, and keeping regular lab checks, you can reap the full benefit without surprises. When in doubt, a quick chat with your pharmacist can save weeks of trial and error.

Can I take over‑the‑counter cold medicine with Olmesartan/Amlodipine?
Most simple decongestants (like pseudoephedrine) are safe, but multi‑symptom formulas often contain NSAIDs or antihistamines that could raise blood‑pressure or kidney‑risk concerns. Stick to acetaminophen for fever and read the label carefully.
Is it okay to drink alcohol while on this combo?
A moderate amount (one drink for women, two for men) usually won’t cause problems, but heavy drinking can intensify the blood‑pressure drop and increase dizziness. If you notice light‑headedness, cut back and talk to your doctor.
Do I need to adjust my dose if I start a potassium supplement?
Usually, the prescription is left unchanged, but you’ll need more frequent potassium and kidney labs. In some cases, the clinician may reduce the Olmesartan dose or switch to a different ARB.
What should I do if I miss a dose?
Take the missed tablet as soon as you remember unless it’s almost time for the next dose. In that case, skip the missed one and continue with your regular schedule. Never double‑dose.
Are there any herbal supplements I should avoid?
St. John’s wort, licorice root, and certain Chinese herbs can influence CYP enzymes or potassium balance. Discuss any herb you take with your pharmacist before starting Olmesartan/Amlodipine.






sara fanisha
October 23, 2025 AT 19:28Great summary! I’ll keep an eye on my potassium intake.
Tristram Torres
November 5, 2025 AT 20:28Honestly, most people just skim this and miss the obvious warnings about NSAIDs.
Jinny Shin
November 18, 2025 AT 22:28This article reads like a dramatic novella, every interaction painted with the gravitas of a Shakespearean tragedy. The author really knows how to make a simple drug interaction feel like a life‑or‑death saga. Still, the facts are solid and worth a careful read.
deepak tanwar
December 2, 2025 AT 00:28While the overview is thorough, I would caution against over‑reliance on grapefruit avoidance alone; many patients underestimate dietary potassium. A more nuanced protocol would incorporate routine electrolyte monitoring irrespective of diet.
Abhishek Kumar
December 15, 2025 AT 02:28Meh, looks okay.
hema khatri
December 28, 2025 AT 04:28We must follow these guidelines-no excuses!
Jennell Vandermolen
January 10, 2026 AT 06:28Your effort to break down the interactions is commendable and will help many stay safe. Keep sharing these practical checklists.
Mike Peuerböck
January 23, 2026 AT 08:28I appreciate the comprehensive tabulation and the clear action points you provided. Such meticulous guidance is invaluable for both clinicians and patients.
Simon Waters
February 5, 2026 AT 10:28Don’t you think the pharma industry is pushing these combo pills to lock us into more prescriptions? Still, the info here is useful if you read between the lines.
Vikas Kumar
February 18, 2026 AT 12:28These guidelines are just another way to control our health choices.
Celeste Flynn
March 3, 2026 AT 14:28For patients starting Olmesartan/Amlodipine, the first step is to obtain a baseline set of labs, including serum creatinine, eGFR, and a full electrolyte panel, as these values will guide future monitoring intervals. Next, review the patient’s current medication list for any agents that are known CYP3A4 inhibitors, such as azole antifungals or macrolide antibiotics, because these can raise amlodipine concentrations and provoke symptomatic hypotension. If a potassium‑sparing diuretic is already part of their regimen, schedule potassium checks at least every two weeks for the first month, then monthly until stability is confirmed. Education about dietary sources of potassium is equally important; patients should be aware that large quantities of bananas, avocados, and certain leafy greens can tip the balance toward hyperkalemia, especially if renal function is marginal. Grapefruit juice, while often overlooked, contains furanocoumarins that inhibit intestinal CYP3A4, leading to a predictable increase in amlodipine exposure; advise patients to limit consumption to no more than occasional servings. Over‑the‑counter NSAIDs should be used sparingly; if required, they should be spaced at least two hours apart from the antihypertensive dose and taken with adequate hydration to minimize renal vasoconstriction. For those who consume alcohol, counsel that moderate intake (up to one drink per day for women and two for men) is generally safe, but binge drinking can amplify the vasodilatory effect of the combo and precipitate dizziness. Lithium users must have serum lithium levels checked within a week of initiating the ARB component, as reduced renal clearance can rapidly push them into toxicity. Finally, establish a clear plan for patients to report red‑flag symptoms-such as sudden swelling, persistent cough, or unexplained faintness-so that dose adjustments or additional investigations can be undertaken promptly. By integrating these steps into routine practice, clinicians can maximize therapeutic benefit while mitigating the risk of adverse interactions.