When you’re tossing and turning every night, waking up exhausted even after eight hours in bed, it’s not just bad sleep-it might be something deeper. That’s where polysomnography comes in. This isn’t a simple snore tracker or a wearable that guesses your sleep quality. It’s the full medical sleep exam, done in a lab, with wires, sensors, and trained technicians watching every move you make while you sleep. And if you’ve been told you need one, it’s normal to feel nervous. But here’s the truth: most people find it easier than they expect. The goal isn’t to catch you being perfect-it’s to understand what’s really happening in your brain and body when you’re asleep.
What Exactly Is a Polysomnography?
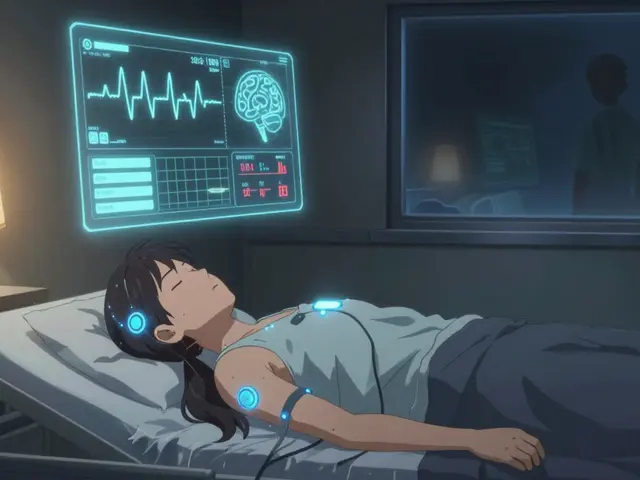
Polysomnography, often called a sleep study, is a multi-parameter test that records your brain waves, eye movements, heart rate, breathing, muscle activity, and oxygen levels-all at the same time. The word itself breaks down to “poly” (many), “somno” (sleep), and “graphy” (recording). It’s not just about counting how many times you stop breathing. It’s about mapping out your entire sleep cycle: how long you spend in each stage, whether you’re entering REM sleep too early, if your legs twitch uncontrollably, or if your heart skips beats during deep sleep.
This test is the gold standard because it captures what home devices can’t. A home sleep apnea test might check your breathing and oxygen, but it doesn’t know if you’re in deep sleep or REM. It can’t tell if you’re having night terrors, sleepwalking, or periodic limb movements. Polysomnography can. That’s why doctors don’t just rely on symptoms like snoring or daytime fatigue-they need the full picture.
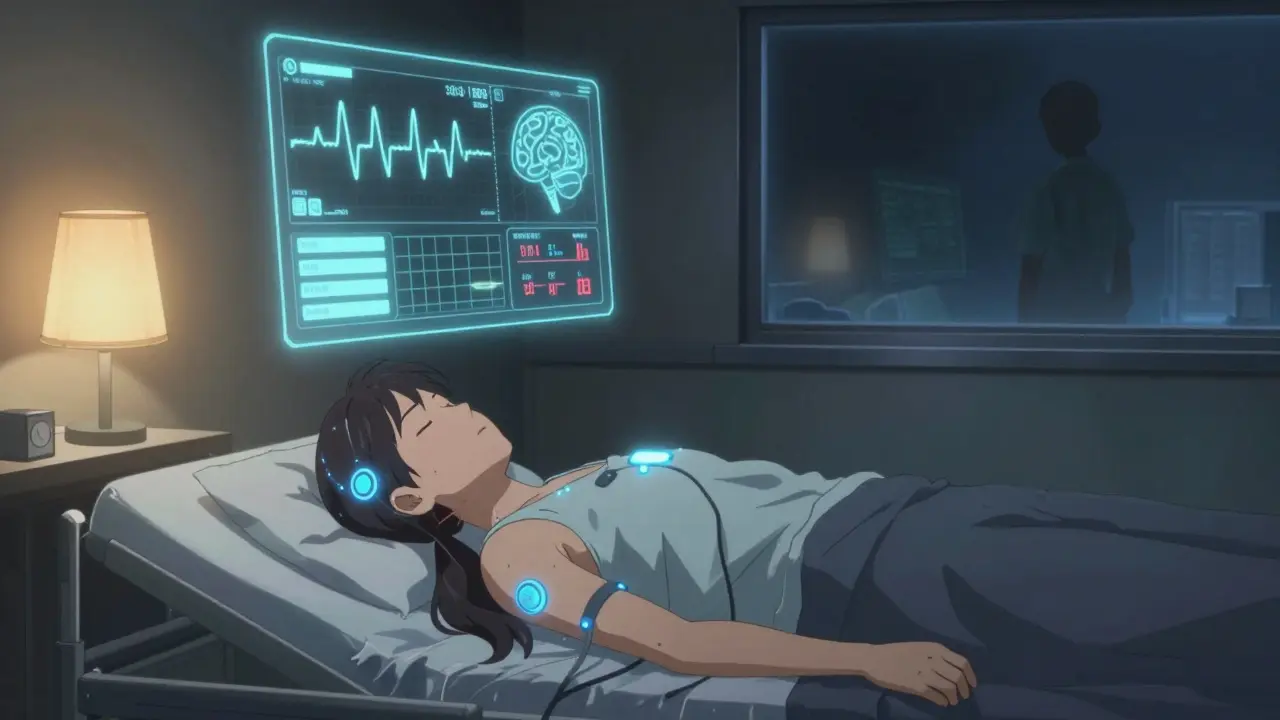
What Happens During the Study?
You’ll arrive at a sleep center about an hour before your usual bedtime. The room looks like a hotel room-private, quiet, with a comfortable bed. No hospital gowns, no IVs. Just a technician who’ll gently attach sensors to your scalp, face, chest, legs, and fingers. There are usually 20 to 22 sensors, but newer wireless systems are cutting that down to under 10. You’ll feel a little strange at first, like wearing a headband and a belt around your chest, but most people get used to it quickly.
The technician will check your signals in real time from another room. They can talk to you through an intercom if you need to use the bathroom or if a sensor falls off. The lights go out at your usual bedtime. You’re encouraged to sleep normally-no forced routines, no caffeine after noon the day before, no naps. The goal is to capture your real sleep, not a version you think you should have.
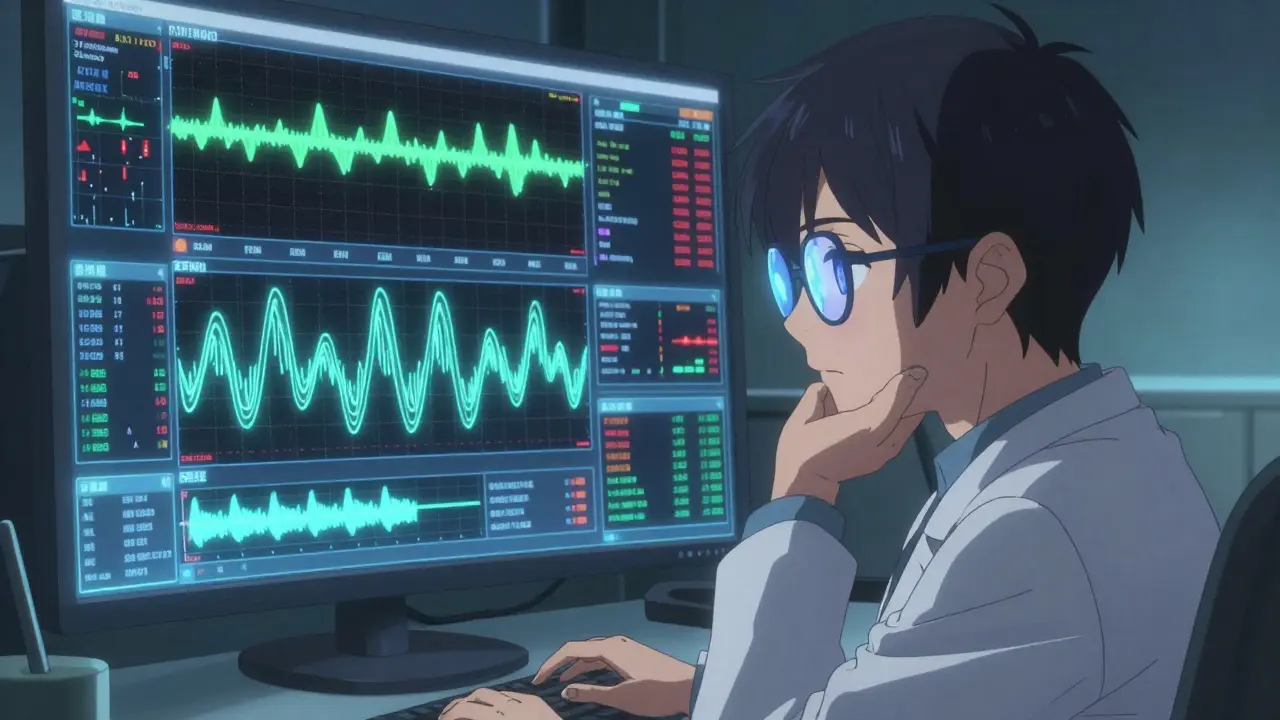
Throughout the night, the machine records:
- EEG (brain waves) - To track sleep stages: light sleep, deep sleep, and REM.
- EOG (eye movements) - To spot when you enter REM sleep, where dreaming happens.
- EMG (muscle activity) - On your chin and legs to catch restless legs or muscle jerks.
- ECG (heart rhythm) - To see if your heart is struggling during apneas.
- Respiratory effort - Belts around your chest and belly to measure if you’re trying to breathe.
- Airflow - Sensors near your nose to detect if air is moving in and out.
- Oxygen levels - A clip on your finger to measure how much oxygen your blood is carrying.
- Body position and sound - Video and audio to catch sleepwalking, talking, or snoring.
The whole thing lasts 6 to 8 hours. Most people sleep enough-about 4 to 5 hours of actual sleep is enough for a diagnosis. Even if you don’t sleep like you do at home, the data still works. The technicians aren’t judging you. They’re just collecting clues.
How Is It Different From Home Sleep Tests?
Home sleep tests are cheaper and more convenient, but they’re also limited. They usually only track three to four things: airflow, oxygen, breathing effort, and heart rate. That’s fine if you’re a 55-year-old man with loud snoring and daytime sleepiness. But if you’re a 30-year-old woman with sudden muscle jerks at night, or someone with unexplained fatigue and no snoring, a home test will miss it.
Polysomnography can diagnose:
- Obstructive sleep apnea (blocked airway)
- Central sleep apnea (brain stops telling muscles to breathe)
- Narcolepsy (falling into REM too fast)
- Restless legs syndrome
- Periodic limb movement disorder
- Night terrors and sleepwalking
- Nocturnal seizures
Home tests can’t diagnose any of these except obstructive sleep apnea-and even then, they fail in 15% to 20% of cases because people don’t sleep well at home, or the device falls off. In-lab polysomnography fails less than 5% of the time. That’s why insurance often requires a lab test before approving treatment for anything beyond basic sleep apnea.
What Do the Results Show?
After your study, a sleep specialist spends 2 to 3 hours reviewing over 1,000 pages of data. They look for patterns:
- Apnea-hypopnea index (AHI) - How many times per hour you stop or reduce breathing. Over 5 is abnormal. Over 30 is severe.
- Oxygen drop index - How often your blood oxygen falls below 90%. Frequent drops mean your body is under stress.
- Sleep efficiency - Percentage of time you were actually asleep vs. lying in bed. Below 85% suggests trouble staying asleep.
- REM latency - How long it takes to enter REM sleep. In narcolepsy, it’s under 15 minutes. Normally, it’s 70-100 minutes.
- Limb movements - Are your legs jerking every 20 seconds? That’s periodic limb movement disorder.
- Body position - Are apneas worse when you’re on your back? That’s positional sleep apnea.
For example, if your AHI is 40, your oxygen drops to 80% every few minutes, and your brain shows you’re not entering deep sleep, you likely have severe obstructive sleep apnea. If your AHI is low but you’re falling into REM within 10 minutes and suddenly collapsing during the day, it’s probably narcolepsy. The data doesn’t lie-it tells the story.
What Happens After the Test?
You’ll get your results in 1 to 2 weeks. The report will say whether you have a sleep disorder, how severe it is, and what kind. If you have sleep apnea, the next step might be a CPAP titration study-another overnight test where you wear a mask and the machine adjusts pressure to find the right setting. Sometimes, this is done in the same night as your original study. That’s called a split-night study. About 35% of polysomnography tests now include this, saving you a second trip.
If you have narcolepsy or parasomnias, you might need a Multiple Sleep Latency Test (MSLT) the next day. That’s a series of naps every two hours to see how fast you fall asleep and whether you enter REM during them.
Treatment depends on the diagnosis. For sleep apnea, it’s CPAP, oral devices, or surgery. For restless legs, it’s iron supplements or medication. For narcolepsy, it’s stimulants and scheduled naps. The right treatment starts with the right test.
Who Needs a Polysomnography?
You might need one if you have:
- Loud snoring with pauses in breathing (witnessed by a partner)
- Daytime sleepiness that interferes with work or driving
- Sudden muscle weakness or collapse when emotional (a sign of narcolepsy)
- Repetitive leg movements or jerks during sleep
- Confusion or violent behavior during sleep
- Unrefreshing sleep despite enough time in bed
- High blood pressure that won’t improve with medication
It’s not just for older adults. Young people with unexplained fatigue, shift workers, and even children with behavioral issues can benefit. Insurance usually covers it if your doctor documents symptoms and rules out other causes.

What About Comfort and Anxiety?
It’s normal to worry about sleeping with wires on. But here’s what most people don’t expect: the technicians are there to help. They’ll explain everything, adjust sensors if they’re uncomfortable, and even turn down the room temperature if you’re too warm. The environment is designed to feel like home-soft lighting, quiet, no alarms.
Most people sleep enough to get a diagnosis. Studies show over 85% of patients complete the test successfully. If you’re anxious, ask for a pre-test tour of the lab. Some centers let you visit the room ahead of time. Others offer a trial night with just a few sensors to get used to the feeling.
And yes, you might not sleep as well as you do at home. But that’s okay. The goal isn’t perfect sleep-it’s enough sleep to see the patterns. Even fragmented sleep gives doctors the data they need.
What’s New in Sleep Study Tech?
Wireless sensors are making the experience less clunky. Older studies used 20+ wires; newer ones use Bluetooth-enabled patches. Some labs now use AI to help flag abnormal events faster, reducing analysis time. Video-EEG is being used more often to catch seizures disguised as sleepwalking. And while home-based polysomnography is being researched, it’s not yet reliable enough to replace the lab version.
The American Academy of Sleep Medicine updated its standards in 2020 to make scoring more consistent across labs. That means your results will be more accurate, no matter where you go.
Final Thoughts
Polysomnography isn’t glamorous. It’s not a quick app or a smartwatch. But if you’ve been struggling with sleep for months-or years-it’s the most powerful tool you have. It turns vague symptoms into clear answers. It gives you a name for what’s been keeping you tired. And once you have that, you can finally fix it.
Don’t let fear of the wires stop you. The real discomfort isn’t the sensors-it’s waking up exhausted every day, knowing something’s wrong but not knowing what. That’s what the test is here to end.
Is a polysomnography painful?
No, it’s not painful. Sensors are taped or clipped to your skin-they don’t pierce or shock you. You might feel slight pressure from the chest belt or a small clip on your finger, but most people say the discomfort is minor and fades once they fall asleep.
Can I use the bathroom during the study?
Yes. Each sensor has a quick-release button. The technician will help you disconnect and reconnect everything so you can go to the bathroom without damaging the equipment.
How long does it take to get results?
Results usually take 1 to 2 weeks. A sleep specialist reviews over 1,000 pages of data, which takes 2 to 3 hours of focused analysis. Your doctor will schedule a follow-up to explain the findings and next steps.
Will insurance cover it?
Most insurance plans, including Medicare, cover polysomnography if your doctor documents symptoms like snoring, daytime sleepiness, or witnessed apneas. Prior authorization is often required, but the test is considered medically necessary for diagnosing sleep disorders.
Can I bring my own pillow or blanket?
Yes. Most sleep centers encourage you to bring your own pillow, blanket, or even pajamas to help you feel more at home. It’s one small thing that can make a big difference in how well you sleep.
What if I don’t sleep at all during the study?
Even if you sleep less than usual, you usually get enough data for a diagnosis. Most sleep disorders show patterns even in partial sleep. If the study is truly unusable-which is rare-the lab will let you know and schedule a repeat.
Are there alternatives to in-lab polysomnography?
Home sleep apnea tests are available for people with high suspicion of obstructive sleep apnea and no other sleep disorders. But they can’t diagnose narcolepsy, parasomnias, or central sleep apnea. If your symptoms are complex, in-lab testing is still the best option.



Katherine Carlock
January 12, 2026 AT 18:58Sona Chandra
January 14, 2026 AT 03:25Jennifer Phelps
January 15, 2026 AT 12:39beth cordell
January 17, 2026 AT 03:31Lauren Warner
January 18, 2026 AT 16:01Craig Wright
January 18, 2026 AT 22:49Lelia Battle
January 20, 2026 AT 02:53Monica Puglia
January 20, 2026 AT 12:24