Ever felt like you’re losing control of your emotions for no reason? One minute you’re fine, the next you’re crying over a spilled coffee or snapping at your partner over something small. If you’re in your late 30s to mid-50s, this isn’t just stress - it could be perimenopause.
What’s Really Happening in Your Brain?
Perimenopause isn’t just about irregular periods or hot flashes. It’s a slow, messy shift in your hormones - especially estrogen, progesterone, and testosterone - that can last 4 to 8 years. And your brain? It’s incredibly sensitive to these changes. Estrogen doesn’t just control your reproductive system. It directly affects serotonin and dopamine - the chemicals that help you feel calm, focused, and happy. When estrogen drops or spikes unpredictably, your brain’s mood regulators go haywire. Progesterone, which helps calm your nervous system by boosting GABA, also declines. That’s why many women report feeling on edge, anxious, or overwhelmed even when life hasn’t changed much. Studies show women have 30-40% more estrogen receptors in their brains than men. That means hormonal shifts hit women harder. During perimenopause, estrogen levels can swing by 50-60% within weeks. One week you’re feeling okay; the next, you’re struggling to get out of bed. It’s not you being dramatic - it’s your neurochemistry rewiring itself.It’s Not Just Sadness - It’s Rage, Irritability, and Emotional Overload
Most people think of depression when they hear “mood changes.” But perimenopause doesn’t always look like sadness. In fact, research from Harvard Health and the Cleveland Clinic shows that irritability and anger are more common than deep sadness. On Reddit’s r/Perimenopause forum, 78% of women reported sudden, intense rage episodes - triggered by things that wouldn’t normally bother them. A Healthline survey found 63% of women said their irritability was damaging relationships. One woman wrote: “I yelled at my 10-year-old for leaving a sock on the floor. Then I sat on the floor and cried because I didn’t recognize myself.” This isn’t “hormonal PMS.” It’s different. Premenstrual dysphoric disorder (PMDD) follows a cycle - symptoms show up 7-10 days before your period and vanish when it starts. Perimenopausal mood swings? They come and go randomly. You might feel fine for weeks, then crash for days. No pattern. No warning.Why Standard Depression Treatments Often Fail
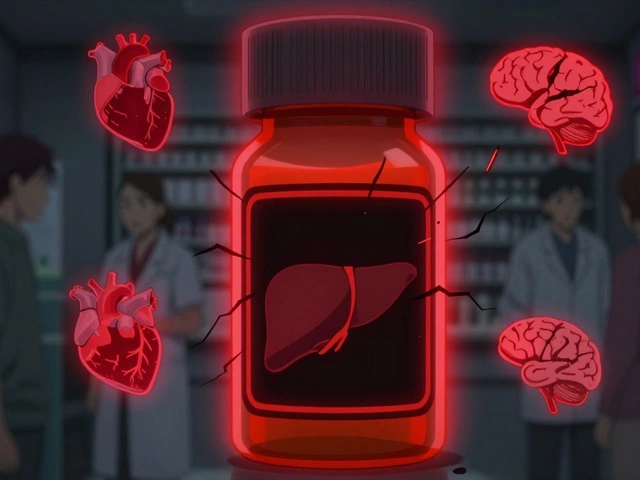
Too many women are told they’re depressed and given SSRIs - and while those can help, they don’t fix the root cause. A 2020 study in the American Journal of Psychiatry found women with perimenopause-related depression are 3.2 times more likely to resist standard antidepressants than those with depression from other causes. Why? Because SSRIs boost serotonin, but they don’t replace estrogen’s role in regulating it. If your brain isn’t getting enough estrogen to make serotonin properly, flooding it with a drug won’t fully fix the problem. Estrogen therapy, on the other hand, helps at the source. Clinical data from My Menopause Centre shows that while SSRIs improve mood in 50-60% of cases, estrogen therapy improves mood in 45-55% - but when used together, success rates jump to over 70%. And here’s the catch: if you’re only treating the mood without addressing sleep or hot flashes, you’re fighting half the battle. Sixty-three percent of perimenopausal women have trouble sleeping. Poor sleep worsens anxiety, lowers frustration tolerance, and makes emotional regulation nearly impossible.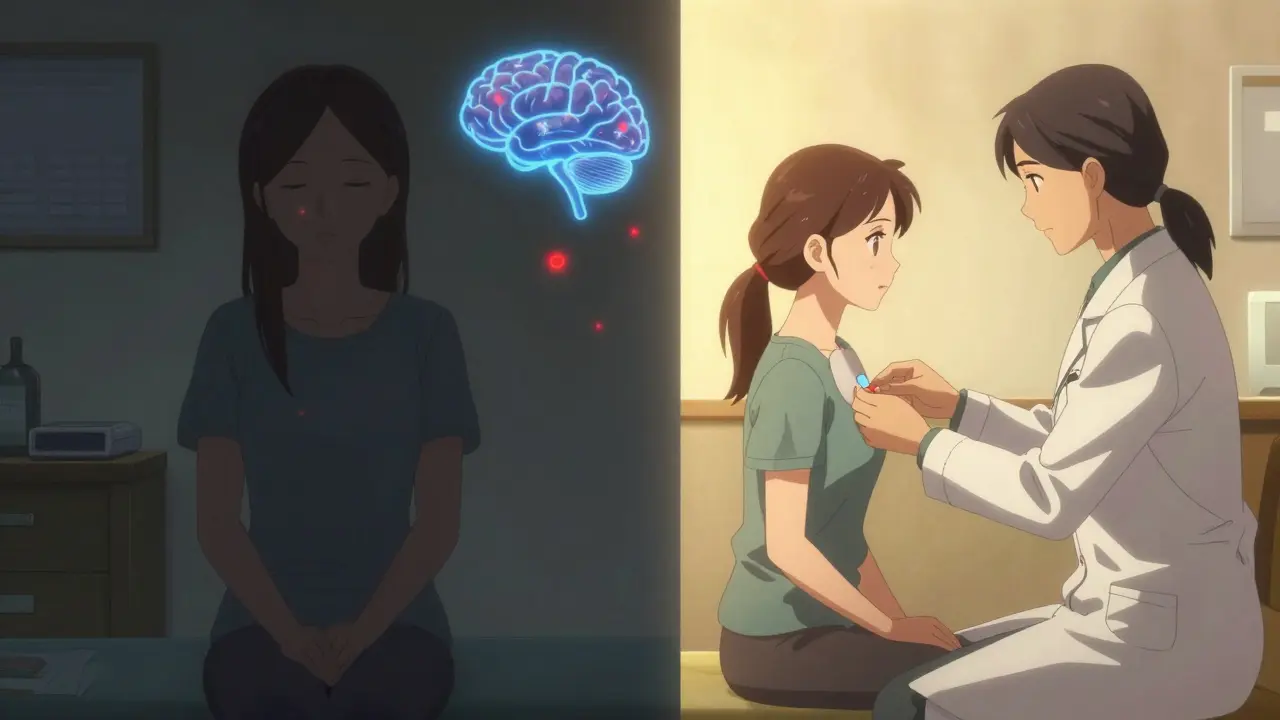
What Actually Works - And What Doesn’t
There’s no one-size-fits-all fix. But here’s what the data says works:- Low-dose estrogen therapy: For women without a history of breast cancer or blood clots, transdermal estrogen (patches or gels) is the most effective for mood and physical symptoms. Doses as low as 0.25 mg daily can make a difference within 6-8 weeks.
- SSRIs or SNRIs: If mood symptoms are severe, low-dose SSRIs like sertraline or escitalopram help - especially when combined with estrogen. They’re not magic, but they’re useful tools.
- Cognitive behavioral therapy (CBT): A 2023 FDA-approved app called MenoMood uses CBT techniques to reduce mood symptoms by 35%. It’s free, accessible, and backed by clinical trials.
- Exercise: Just 30 minutes of brisk walking or strength training 4 times a week improves sleep, reduces stress hormones, and boosts endorphins. It’s not a cure, but it’s a powerful stabilizer.
- Sleep hygiene: Cooling your bedroom, avoiding caffeine after 2 p.m., and using a weighted blanket can cut night sweats and improve deep sleep - which directly improves mood.
How to Know If It’s Perimenopause - Or Something Else
The biggest mistake? Getting misdiagnosed. Cleveland Clinic’s 2022 patient survey found 34% of women were first told they had clinical depression - when it was actually perimenopause. Here’s how to tell the difference:- Perimenopause mood swings: Come with hot flashes, night sweats, irregular periods, brain fog, and sleep issues. They’re unpredictable and last months or years.
- Clinical depression: Lasts longer than two weeks, includes persistent sadness, loss of interest in everything, weight changes, and feelings of worthlessness - without physical hormonal symptoms.
- PMDD: Follows a strict monthly cycle. Symptoms disappear after your period starts.

When to See a Specialist - And Who to Ask For
Not all OB/GYNs are trained in perimenopause. In 2018, only 29% of doctors routinely screened for mood symptoms. By 2023, that number jumped to 54% - but you still need to ask. Look for a certified menopause practitioner. There are about 2,300 in the U.S. and growing. They know the difference between hormone-driven mood changes and other conditions. The North American Menopause Society has a free clinician finder tool. If your doctor says, “It’s all in your head,” or “You’re just stressed,” walk out. That’s outdated thinking. The American College of Obstetricians and Gynecologists confirmed in 2021: hormonal changes during perimenopause can trigger or worsen mood disorders. It’s biology - not weakness.Real Stories, Real Relief
Sarah, 48, from Chester, started feeling like she was “losing her mind” at 44. She was snapping at her husband, crying during TV commercials, and couldn’t focus at work. Her GP prescribed an SSRI. It helped a little - but she still felt off. After six months of tracking symptoms, she found a menopause specialist. They started her on a low-dose estrogen patch and added a low-dose SSRI. Within 10 weeks, her rage episodes dropped by 80%. “I felt like I got myself back,” she said. “Not a better version - just me.” Another woman, 51, started using the MenoMood app after her insurance denied HRT. She did 15 minutes of CBT exercises daily. Within three months, her anxiety scores dropped 40%. “It didn’t fix everything,” she said, “but it gave me back control.”What’s Next? Better Tools Are Coming
The National Institutes of Health just launched a $47 million study tracking 10,000 women over five years to find biological markers for perimenopause-related mood disorders. By 2026, we may have blood tests that can tell if your depression is hormone-driven. New treatments are on the horizon too. Fezolinetant, approved in 2023, helps with hot flashes - and many users report better sleep and mood as a side effect. Gut microbiome therapies are in early trials, aiming to help the body recycle estrogen more efficiently. The bottom line? Perimenopause isn’t something you just endure. It’s a medical phase - and you deserve treatment that addresses your whole self, not just your period.Can perimenopause cause depression?
Yes. Hormonal shifts - especially drops in estrogen - can trigger depression in women with no prior history. About 10%-20% of women experience clinically significant mood disorders during perimenopause. It’s not “just sadness” - it’s a biological response to changing brain chemistry.
Is hormone replacement therapy safe for mood symptoms?
For most healthy women without a history of breast cancer, blood clots, or stroke, low-dose estrogen therapy is safe and effective for mood symptoms. Transdermal patches or gels are preferred over pills because they carry lower risks. Always discuss your personal health history with a specialist.
How long does it take for perimenopause mood symptoms to improve?
It varies. Some women notice improvement in 4-6 weeks with hormone therapy. Others take 3-6 months, especially if combining treatments. Lifestyle changes like sleep, exercise, and stress management can take 8-12 weeks to show noticeable effects. Patience and consistency matter.
Can I treat perimenopause mood swings without medication?
Yes - but only for mild symptoms. Exercise, sleep hygiene, CBT apps, reducing alcohol and caffeine, and mindfulness practices can help stabilize mood. But if symptoms are interfering with work, relationships, or daily life, medication or hormone therapy should be considered. You don’t have to suffer in silence.
Why do some women have severe mood symptoms and others don’t?
It’s a mix of biology and life stress. Women with a history of depression, anxiety, or PMS are five times more likely to have severe mood symptoms. But even women without prior mental health issues can be affected. Genetics, lifestyle, sleep quality, and stress levels all play a role. It’s not about being “stronger” or “weaker” - it’s about individual brain chemistry.






Janette Martens
December 28, 2025 AT 20:02ok but like why are we even talking about this like i got my period at 47 and now its gone and i dont care about serotonin or whatever my brain is fine i just need more coffee and less people asking me if im ok
Marie-Pierre Gonzalez
December 30, 2025 AT 18:48Thank you for this thoughtful, evidence-based overview. As a woman navigating perimenopause while managing a full-time career and two young children, I can attest that the emotional turbulence is often mislabeled as 'stress' or 'burnout.' The distinction between PMDD and perimenopausal mood shifts is critical-and so is the recognition that hormone therapy, when appropriate, is not a 'cure-all' but a legitimate medical intervention. I encourage all clinicians to screen proactively. You are not alone, and you are not 'overreacting.'
Louis Paré
December 31, 2025 AT 18:24Let’s be real-this whole 'perimenopause is a medical crisis' narrative is just capitalism repackaging natural biology as a pathology. You’re telling me a woman’s brain is so fragile that a 50% estrogen swing makes her cry over spilled coffee? That’s not neurochemistry-that’s cultural conditioning. Where’s the data on menopause and male emotional stability? Oh right, because men don’t get to be 'victims' of biology. This is performative victimhood dressed up as science.
Kelsey Youmans
January 1, 2026 AT 00:43Thank you for sharing this with such clarity and compassion. I’ve seen too many women dismissed by their doctors, told to 'take a pill and calm down' when what they really needed was someone to listen and validate their experience. The combination of estrogen therapy and CBT has been life-changing for several patients I’ve worked with. It’s not about weakness-it’s about physiology. And we owe it to every woman to take this seriously.
Sydney Lee
January 1, 2026 AT 21:23...And yet, despite all the 'evidence' cited here, we still live in a world where a woman who expresses anger is labeled 'hormonal'-while a man who does the same is called 'passionate.' This article, while meticulously researched, still operates within the patriarchal framework that pathologizes female emotion. The real solution isn't estrogen patches-it's dismantling the systems that make women feel like they must apologize for their own existence. Also, the 'MenoMood' app? Cute. But it won't fix a culture that tells women to smile and shut up.
oluwarotimi w alaka
January 3, 2026 AT 10:58so u know who really controls the estrogen narrative? big pharma and the WHO they got the whole world scared of natural aging so they can sell u patches and apps and antidepressants… my cousin in lagos she just drinks bitter leaf tea and eats yam and her moods are better than my sister who takes 3 pills a day… this is all a scam to make u pay for normal life
Debra Cagwin
January 4, 2026 AT 09:10To anyone reading this and feeling lost-you’re not broken. You’re not failing. You’re not 'too emotional.' What you’re experiencing is real, valid, and treatable. Start by tracking your symptoms. Talk to a menopause specialist. Try the CBT app-it’s free, it’s science-backed, and it won’t judge you. You don’t have to suffer silently. I’ve walked this path too. You’ve got this.
Hakim Bachiri
January 4, 2026 AT 22:42Wait-so you’re telling me that after 40 years of being told to 'toughen up' and 'stop being so sensitive,' now we’re supposed to believe that women’s brains are biologically wired to be emotionally unstable during perimenopause?!! And the solution is… MORE DRUGS?!?! This isn’t medicine-it’s institutional gaslighting with a side of corporate sponsorship!! The real issue? A society that ignores women’s health until it’s profitable to fix it!! I’m not taking a patch-I’m taking back my narrative!!