Metformin B12 Risk Calculator
Your Risk Factors
Risk Results
Many people with type 2 diabetes rely on metformin to keep their blood sugar under control. It’s been the go-to drug for decades-safe, effective, and cheap. But there’s a hidden risk that doesn’t show up on most patient information sheets: metformin can slowly drain your vitamin B12 levels over time. And if left unchecked, that deficiency can lead to serious, sometimes permanent, nerve damage.
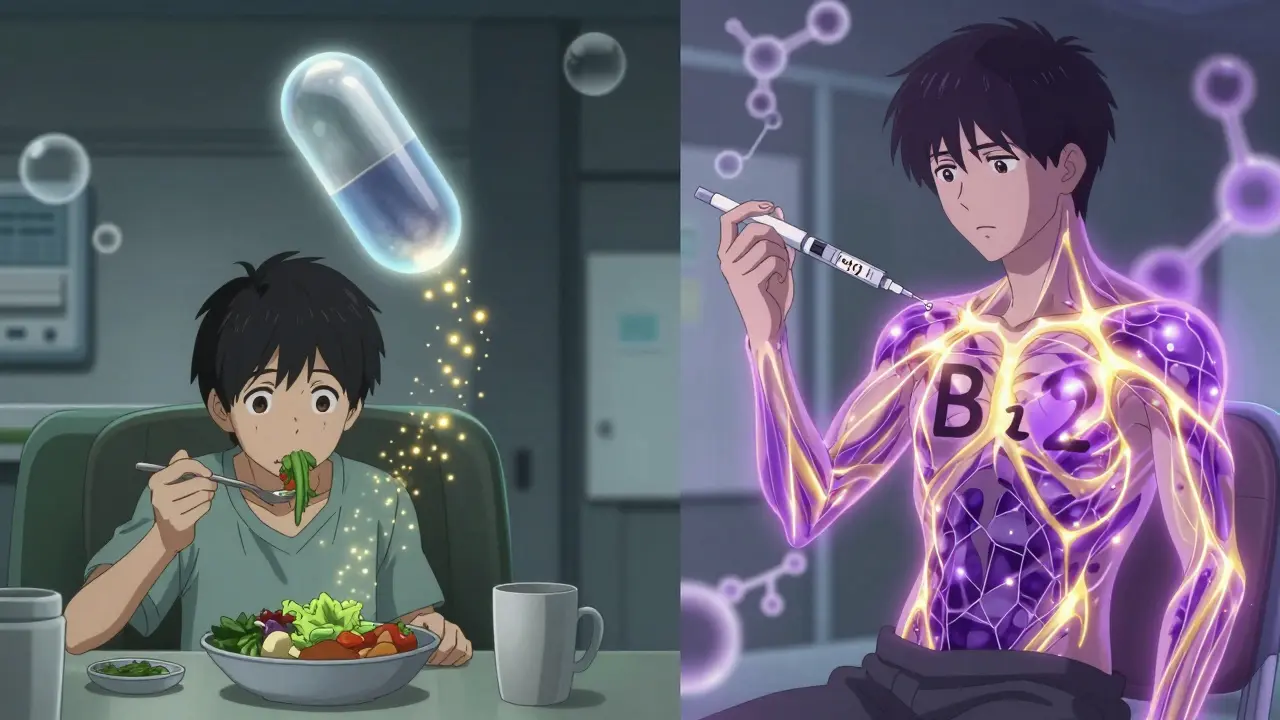
How Metformin Steals Your B12
Metformin doesn’t directly destroy vitamin B12. Instead, it interferes with how your body absorbs it. The drug disrupts a calcium-dependent process in your small intestine, specifically in the terminal ileum, where B12 normally gets pulled into your bloodstream. Studies show this reduces absorption by 25-30%. It’s not a quick problem-it takes years. Your liver stores about 2,500 micrograms of B12, and you only need 2.4 micrograms a day. So depletion happens slowly, often after 4 to 5 years of daily use.
The risk gets worse with higher doses. Every extra 1 gram of metformin per day nearly doubles your chance of becoming deficient. People taking 2,000 mg or more daily are at the highest risk. And if you’re also on a proton-pump inhibitor (PPI) like omeprazole for heartburn, your risk jumps even higher. PPIs reduce stomach acid, which is needed to free B12 from food. So you’ve got two drugs working against your B12 absorption at once.
Why This Is Often Missed
One of the biggest problems is that symptoms look exactly like complications of diabetes. Fatigue? Muscle weakness? Numbness in hands or feet? Tingling? These are common in both diabetic neuropathy and B12 deficiency. Many doctors assume it’s just the diabetes getting worse. But here’s the catch: you can have severe B12 deficiency without anemia. That’s right-no pale skin, no low red blood cell count. Just nerve damage. A landmark study following over 2,000 people for 13 years found that B12 deficiency appeared in patients even when their blood counts were normal.
And it’s not rare. Research shows 10-30% of people on metformin long-term develop deficiency. For those taking it for 12 years or more, that number climbs to over 50%. With over 150 million people worldwide on metformin, we’re talking about millions at risk.
What Symptoms Should You Watch For?
Don’t wait for numbness or tingling to become unbearable. Early signs are subtle but telltale:
- Feeling unusually tired (reported by 72% of deficient patients in long-term studies)
- Muscle weakness, especially in legs
- Sore, red, swollen tongue
- Mouth ulcers that won’t heal
- Pale or slightly yellow skin
- Blurred or double vision
- Memory problems or brain fog
One patient on a UK diabetes forum shared that after 8 years on metformin, she was told her worsening nerve pain was just diabetes progression. Her B12 level was 128 pmol/L-well below the normal range of 221 pmol/L. After six months of B12 injections, her symptoms improved dramatically. That’s not an outlier. It’s a pattern.
Who’s at Highest Risk?
Not everyone on metformin will develop B12 deficiency-but some groups are far more vulnerable:
- Those taking 2,000 mg or more daily
- People on metformin for 5+ years
- Vegetarians and vegans (no dietary B12 sources)
- Those using PPIs or H2 blockers for acid reflux
- Older adults (natural B12 absorption declines with age)
- People with a history of gut surgery or malabsorption
Studies show that vegetarian patients on metformin are at a double disadvantage: no dietary intake + impaired absorption. That’s a recipe for deficiency.
What Doctors Should Be Doing
Guidelines have changed. The UK’s Medicines and Healthcare products Regulatory Agency (MHRA) updated its warning in July 2022, calling B12 deficiency a “common side effect.” The European Association for the Study of Diabetes says: “Routine serum B12 measurement at baseline and every 2-3 years in all patients prescribed metformin.” The American Diabetes Association is more cautious, saying to “consider” testing-but even they now recommend checking levels in patients with anemia or neuropathy.
The National Institute for Health and Care Excellence (NICE) in the UK updated its guidance in January 2023 to recommend testing every 2-3 years for everyone on long-term metformin, and annually for high-risk groups. That’s the standard you should expect.
How It’s Diagnosed
A simple blood test for serum B12 is the first step. But here’s the problem: a “low-normal” result can still mean your body is running on empty. That’s why doctors should also check:
- Methylmalonic acid (MMA)-this rises when your cells lack B12, even if serum levels look okay
- Homocysteine-also elevated in B12 deficiency
If your serum B12 is below 200 pmol/L, treatment is clear. If it’s between 200-300 pmol/L and you have symptoms, test MMA. If MMA is high, you’re deficient-even if your B12 looks “fine.”
How It’s Treated
Good news: B12 deficiency is reversible-if caught early. Treatment depends on severity:
- Severe deficiency or neurological symptoms: 1,000 mcg intramuscular injections weekly for 4 weeks, then monthly
- Mild to moderate deficiency: 1,000-2,000 mcg oral B12 daily (yes, high-dose pills work just as well as injections for most people)
In the DPP/DPPOS study, 89% of patients saw their blood counts normalize within 3 months of starting supplementation. Neurological symptoms took longer-often 6 to 12 months-but improved in most cases.
But here’s the catch: if nerve damage has become permanent-like subacute combined degeneration of the spinal cord-it won’t go away. That’s why early detection matters so much.

Can You Prevent It?
Yes. And it’s easier than you think.
One 2021 trial in Diabetes Care tested adding 1,200 mg of calcium carbonate daily to metformin regimens. The result? A 47% drop in B12 deficiency over two years. Why? Calcium helps restore the absorption process that metformin disrupts. It’s not a magic bullet, but it’s a simple, cheap, safe way to reduce risk.
Other options:
- Take a daily B12 supplement (1,000 mcg) if you’ve been on metformin for more than 3 years
- Choose a B12 form like methylcobalamin or adenosylcobalamin-more bioavailable than cyanocobalamin
- Ask your doctor about enteric-coated metformin (still in trials, but early results show 32% less B12 reduction)
What’s Next?
Research is moving fast. Scientists have identified genetic variants in the CUBN gene that make some people more prone to B12 malabsorption when on metformin. In the future, a simple genetic test might tell you if you’re at high risk before you even start the drug.
By 2025, most major diabetes programs worldwide plan to include routine B12 testing as standard care. The cost? Around $18-25 per patient per year. The savings? Up to $187 per patient in avoided nerve damage, hospital visits, and lost productivity.
Metformin saves lives. But it shouldn’t cost you your nerves. If you’ve been on it for more than 4 years, ask for a B12 test. Don’t wait for symptoms to get bad. That’s how preventable damage becomes permanent.
Frequently Asked Questions
Can metformin cause permanent nerve damage?
Yes-if vitamin B12 deficiency goes undetected for years. Low B12 can lead to subacute combined degeneration of the spinal cord, a type of nerve damage that affects balance, coordination, and sensation. Once this damage becomes severe, it may not fully reverse, even with treatment. That’s why early testing is critical.
Do I need to stop taking metformin if I have low B12?
No. Stopping metformin isn’t usually necessary. Most people can continue taking it while supplementing with B12. The benefits of blood sugar control often outweigh the risk of deficiency, especially since B12 can be easily replaced with supplements or injections. Talk to your doctor about the best balance for your situation.
Can I get enough B12 from food while on metformin?
It’s unlikely. Even if you eat meat, fish, or dairy, metformin blocks up to 30% of absorption. Dietary B12 isn’t enough to compensate for that loss. Supplementing is the only reliable way to prevent deficiency. Vegetarians and vegans are especially at risk because their diets lack natural B12 sources.
How often should I get my B12 levels checked?
If you’ve been on metformin for more than 4 years, get tested every 2-3 years. If you’re in a high-risk group-vegetarian, on PPIs, over 65, or taking high doses-get tested annually. Don’t wait for symptoms. By the time you feel tired or numb, damage may already be underway.
Are B12 injections better than pills?
For severe deficiency or neurological symptoms, injections are faster and more reliable. But for most people with mild to moderate deficiency, high-dose oral B12 (1,000-2,000 mcg daily) works just as well. Studies show oral supplements can raise levels and reverse symptoms without injections. The choice depends on severity, not preference.
Can calcium supplements help prevent B12 deficiency from metformin?
Yes. A 2021 clinical trial found that taking 1,200 mg of calcium carbonate daily reduced the risk of B12 deficiency by 47% over two years. Calcium helps restore the absorption process that metformin disrupts. It’s a simple, low-cost way to protect yourself while continuing metformin.
Next Steps
If you’re on metformin and haven’t had your B12 checked in the last two years, schedule a blood test. Ask for serum B12, MMA, and homocysteine. Don’t settle for just one number. If your levels are low or borderline, start supplementation right away. If you’re vegetarian, vegan, or on acid-reducing meds, don’t wait-start daily B12 supplements now. This isn’t a theory. It’s a proven, preventable risk. And you’re the only one who can act on it.







Madhav Malhotra
January 12, 2026 AT 06:18Man, I’ve been on metformin for 7 years and never knew this. I thought my fatigue was just from working two jobs. Gonna ask my doc for a B12 test this week. Thanks for the heads-up!
Alex Smith
January 12, 2026 AT 17:50Oh wow, so metformin’s just quietly turning us into B12-deficient zombies while we’re busy congratulating ourselves on not needing insulin? Classic pharma move - keep the glucose down, wreck the nerves. Next they’ll tell us aspirin causes ‘subtle vitamin K depletion’ and we’ll all be bleeding out in our sleep. 😏
Roshan Joy
January 12, 2026 AT 19:01Good post! I’m vegetarian and on metformin - this explains why I’ve been so tired lately. I started taking 1000 mcg methylcobalamin daily last month. My brain fog’s already clearing up. 🙌 Also, calcium carbonate tip? Genius. I’m adding it to my routine.
Adewumi Gbotemi
January 14, 2026 AT 12:37Wow. I never thought my tingling feet was from medicine. I thought it was just old age. I will go check my B12 now. Thank you for sharing.
Vincent Clarizio
January 15, 2026 AT 07:53Let’s be real - this isn’t some ‘hidden risk.’ It’s a systemic failure of medical education. Doctors are trained to treat symptoms, not investigate root causes. They see neuropathy? ‘Oh, it’s diabetic.’ They see fatigue? ‘Oh, it’s metabolic syndrome.’ They don’t look at labs unless you beg them to. And even then, they rely on serum B12 alone, ignoring MMA and homocysteine. We’ve turned medicine into a guessing game where the patient is the one who has to do all the homework. And for what? To keep drug sales up? To avoid the 3-minute conversation that could’ve prevented permanent nerve damage? Pathetic.
Jennifer Littler
January 16, 2026 AT 21:34As an endocrinology NP, I see this constantly. Serum B12 <300 pmol/L with elevated MMA = deficiency, period. Yet I still get pushback from primary care docs who say ‘it’s normal’ because it’s ‘not anemic.’ We need better guidelines, better training, and better patient advocacy. This isn’t niche - it’s epidemic. And yes, oral B12 at 2000 mcg daily works just fine for most. No need for injections unless there’s malabsorption or severe neuro symptoms.
Sean Feng
January 18, 2026 AT 15:14So take a pill. Done. Why is this even a post?
Priscilla Kraft
January 19, 2026 AT 17:00YES! I’ve been telling my patients this for years. And the calcium tip? Game-changer. I now recommend 1200 mg calcium carbonate with dinner for everyone on metformin >3 years. It’s cheap, safe, and backed by solid data. Also - if you’re vegan, start B12 supplements NOW. Don’t wait for symptoms. Your nerves will thank you. 💪
Christian Basel
January 20, 2026 AT 08:37Metformin-induced B12 deficiency is well-documented in the literature. The mechanism involves inhibition of the cubilin receptor in the terminal ileum, which is calcium-dependent. The clinical relevance is amplified in populations with pre-existing malabsorption or dietary insufficiency. Screening protocols should be standardized across primary care. The cost-benefit analysis strongly favors routine testing.
Michael Patterson
January 22, 2026 AT 05:56So let me get this straight - you’re saying we’ve been giving millions of people a drug that slowly fries their nerves, and no one noticed for decades? And now we’re just gonna slap on a B12 pill like it’s a band-aid? What about the other 100 side effects they didn’t tell us about? I bet metformin also causes you to forget your own name after 10 years. I’m switching to berberine. At least that’s natural.
Matthew Miller
January 24, 2026 AT 05:47Typical. Another ‘awareness’ post from someone who read one study and thinks they’re a doctor now. You didn’t mention the 40% of people who take metformin and have perfectly normal B12 levels. You didn’t mention that B12 supplements can mask pernicious anemia. You didn’t mention that high-dose oral B12 isn’t regulated and can be contaminated. You’re not helping - you’re scaring people into taking unneeded supplements. Stop the fearmongering.
Priya Patel
January 26, 2026 AT 02:39I’m on metformin and vegan - this hit me right in the feels. My hands have been tingling for months and I thought it was just typing too much. Just got my bloodwork back - B12 at 180. I’m starting injections next week. Thank you for posting this. I feel less alone now 💙
Jason Shriner
January 26, 2026 AT 11:51So metformin = slow nerve death? Cool. So what’s next? Is insulin gonna make you forget your kids’ names? Are statins secretly stealing your dopamine? We’re living in a world where every drug is a villain and every supplement is a savior. I’m just waiting for someone to write a 5000-word essay on how drinking water causes kidney stones. 🤡
Alfred Schmidt
January 28, 2026 AT 00:59THIS IS WHY I HATE MODERN MEDICINE!!! I’ve been on metformin for 9 years and my doctor never tested my B12! I’ve had nerve pain for 3 years and they called it ‘idiopathic neuropathy’!!! I’ve been suffering in silence because NO ONE TOLD ME!!! I’m going to sue my clinic!! I’m going to start a petition!! I’m going to post this on every forum I can find!!! I need a therapist!! I need B12 injections RIGHT NOW!!!