Beta-Blockers: What They Are, How They Work, and What You Need to Know
When your heart races too fast or your blood pressure stays too high, beta-blockers, a class of medications that slow heart rate and reduce blood pressure by blocking adrenaline effects. Also known as beta-adrenergic blocking agents, they’re one of the most prescribed drug types for heart conditions, anxiety, and even migraine prevention. Unlike painkillers or antibiotics, beta-blockers don’t fix the problem—they help your body handle it better. They’re not flashy, but millions rely on them daily to avoid heart attacks, strokes, and dangerous spikes in blood pressure.
These drugs work by blocking beta receptors in your heart and blood vessels. When adrenaline hits those receptors, your heart beats harder and faster. Beta-blockers step in and say, "Not today." That’s why they’re used for high blood pressure, a condition where force against artery walls is too strong, increasing risk of heart damage, angina, chest pain caused by reduced blood flow to the heart, and even heart failure, when the heart can’t pump enough blood to meet the body’s needs. They’re also used off-label for tremors, performance anxiety, and migraines—because slowing down the nervous system’s overdrive helps in more ways than one.
But they’re not magic. Some people feel tired, dizzy, or cold in their hands and feet. Others notice their heart rate dropping too low. These aren’t rare side effects—they’re expected for some. That’s why timing matters, why dose adjustments are common, and why you shouldn’t stop them cold turkey. Your body adapts. Abruptly stopping can trigger rebound high blood pressure or even a heart attack. That’s why doctors often taper the dose.
What’s interesting is how beta-blockers fit into bigger health patterns. If you’re on one, you’re likely also managing diet, exercise, or other meds like diuretics or ACE inhibitors. You might be switching from brand to generic versions, dealing with drug shortages, or noticing side effects that don’t match what your doctor told you. That’s normal. The real challenge isn’t just taking the pill—it’s understanding how it fits with everything else in your routine. Timing matters. Food matters. Other drugs matter. And so does your mental health—some people report low mood or sleep issues, which can be mistaken for depression when it’s just the medication.
There’s no one-size-fits-all beta-blocker. Propranolol, metoprolol, atenolol—they all have different strengths, durations, and side effect profiles. One might be better for anxiety. Another for heart rhythm. A third for post-heart attack recovery. The choice depends on your body, your other conditions, and what you can tolerate. And if one doesn’t work, there are alternatives: calcium channel blockers, ACE inhibitors, or newer heart drugs that work differently.
What you’ll find below isn’t just a list of articles. It’s a collection of real-world experiences, safety checks, and practical advice from people who’ve lived with these drugs. You’ll see how timing affects side effects, how pharmacists catch dangerous interactions, and how patients manage long-term use without losing quality of life. These aren’t theoretical guides—they’re the kind of info you wish you’d found before your first prescription.
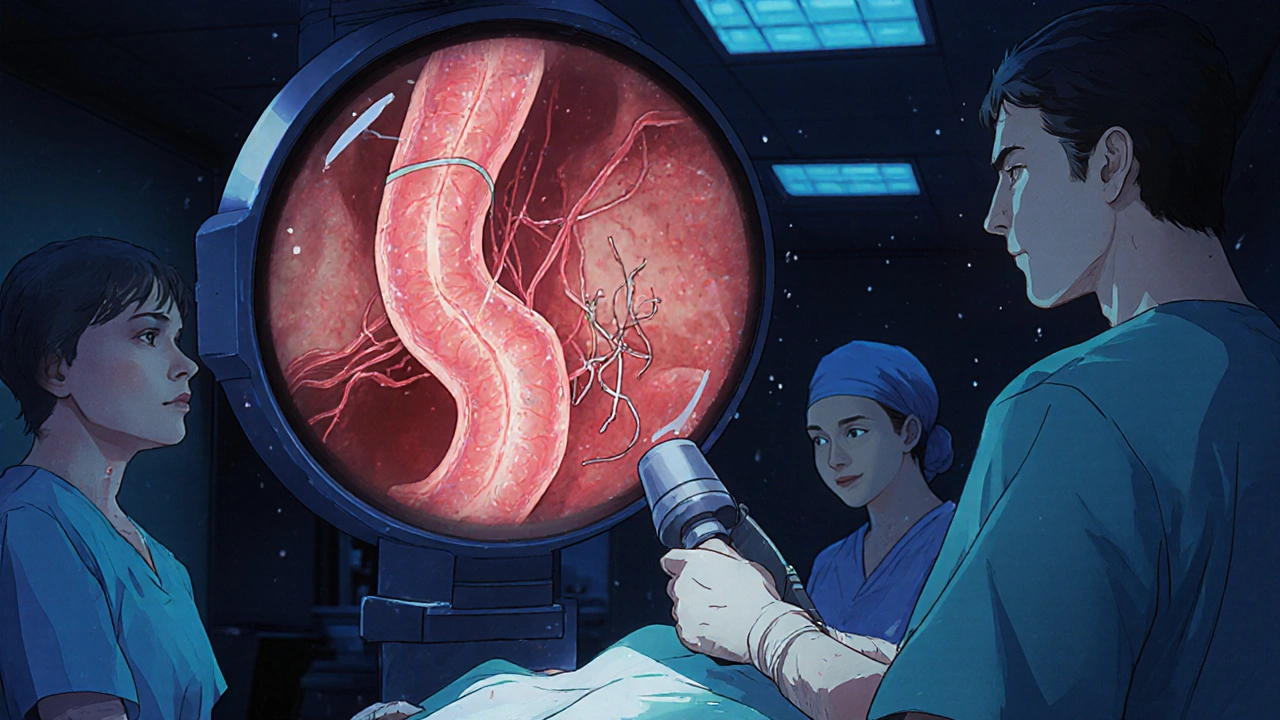
Variceal bleeding is a life-threatening complication of liver cirrhosis. Learn how endoscopic banding, beta-blockers like carvedilol, and prevention strategies can stop bleeding and save lives.
Recent-posts
Categories
Tags
- online pharmacy
- side effects
- drug interactions
- generic drugs
- online pharmacy UK
- drug safety
- opioid side effects
- pill organizer
- Tadalafil
- arthritis medication
- buy medication online
- prescription medication
- quit smoking
- motion sickness
- Sildenafil
- Vardenafil
- ED medication alternatives
- biologics
- medication safety
- generic medication prices