Heart disease isn’t just something that happens to older people. It’s quietly building in your body right now-if you’re ignoring the warning signs. The truth? About 80% of premature heart disease and stroke can be prevented. Not with magic pills. Not with expensive treatments. But by understanding and acting on the real risk factors you can actually change.
Age Isn’t Just a Number-It’s a Signal
You can’t turn back time, but you can stop pretending age doesn’t matter. For men, the risk of heart disease starts climbing noticeably after 45. For women, it’s around 55-right after menopause, when estrogen drops. That’s not coincidence. It’s biology. The Framingham Heart Study shows that by age 40, men have a 50% lifetime chance of developing heart disease. Women? Around 40%. By 70? Those numbers jump to 70% and 60%. Each decade adds about 10% more risk-on top of everything else. But here’s the catch: age doesn’t act alone. It teams up with other factors. A 60-year-old smoker with high blood pressure isn’t just at higher risk-they’re at exponentially higher risk. Age doesn’t cause heart disease. It gives other risks time to do damage.Family History: Your Genetic Blueprint
If your dad had a heart attack at 52, or your mom had blocked arteries before 60, you’re not just unlucky-you’re in a higher-risk group. Having a first-degree relative (parent or sibling) with early heart disease increases your risk by 30% to 75%, depending on how many relatives are affected and how young they were when it happened. Some genetic conditions are even more serious. Familial hypercholesterolemia affects 1 in 250 people. If you have it and don’t treat it, your chance of a heart attack before 50 is nearly 50%. That’s not rare. That’s preventable-if you know. Genetics aren’t destiny, but they’re a loud alarm. If your family has a history of early heart disease, don’t wait for symptoms. Get checked. Get your cholesterol tested. Ask your doctor about genetic screening. Knowing your risk lets you act decades before it’s too late.Smoking: The Single Most Preventable Killer
Smoking isn’t just bad for your lungs. It’s a direct attack on your heart. Current smokers are two to four times more likely to develop coronary heart disease than non-smokers. Even if you only smoke 1 to 5 cigarettes a day? Your risk still goes up by 50%. In the U.S., smoking causes about 1 in every 4 deaths from heart disease. That’s not a guess. That’s data from the CDC. The chemicals in cigarette smoke damage blood vessels, raise blood pressure, lower good cholesterol, and make your blood more likely to clot. One cigarette can trigger a heart rhythm problem. Ten can start a chain reaction. The good news? Quitting works faster than most people think. Within one year of quitting, your heart disease risk drops by half. After 15 years, it’s nearly the same as someone who never smoked. You don’t need to be perfect. Just stop. Every day without a cigarette is a win.High Blood Pressure: The Silent Saboteur
High blood pressure doesn’t hurt. That’s why it’s so dangerous. About 47% of American adults have it-and most don’t know. When your blood pressure stays above 130/80, your arteries stretch and weaken. Your heart has to work harder. Over time, this leads to thickened heart muscle, damaged vessels, and eventually, heart failure or stroke. Uncontrolled high blood pressure can increase your heart disease risk by 300% to 400%. The SPRINT trial showed that lowering systolic pressure to under 120 (instead of the old target of 140) cut cardiovascular events by 25% in high-risk people. That’s huge. You don’t need a fancy device to check it. Most pharmacies have free machines. If your reading is consistently above 130/80, talk to your doctor. Lifestyle changes-like cutting salt, losing weight, and walking daily-can bring numbers down. But sometimes, you need medication. That’s not weakness. It’s smart.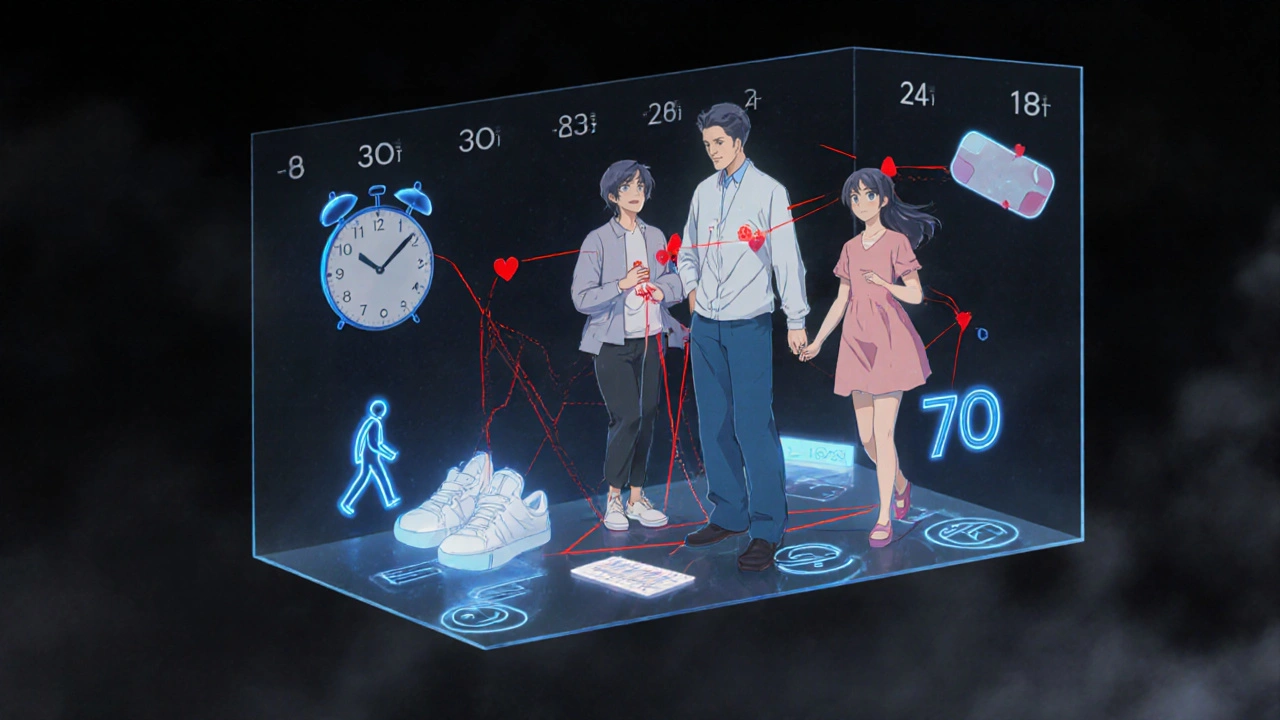
Cholesterol: Not All Fat Is Bad
Cholesterol gets a bad rap. But your body needs it. The problem is when LDL (the “bad” kind) builds up in your arteries. Nearly 94 million U.S. adults have LDL levels too high. That’s 38% of the population. High LDL increases heart disease risk by about 50%. But it’s not just about the number. It’s about size, density, and inflammation. That’s why statins are often prescribed-they don’t just lower cholesterol. They reduce inflammation in artery walls. High-intensity statins (like atorvastatin or rosuvastatin) can cut heart attack risk by 25% to 35% in people who already have heart disease or are at high risk. HDL (“good” cholesterol) helps remove LDL from your blood. But chasing high HDL with supplements doesn’t work. What does? Exercise. Losing belly fat. Quitting smoking. Eating healthy fats (like olive oil, nuts, and fatty fish). Don’t fixate on one number. Look at the whole picture.Diabetes: A Heart Disease Accelerator
If you have diabetes, your heart is already under stress. People with diabetes are two to four times more likely to die from heart disease. And 68% of those over 65 with diabetes will die from heart-related causes. High blood sugar damages blood vessels and nerves that control your heart. It also makes inflammation worse and increases clotting risk. The good news? Managing your blood sugar isn’t just about insulin or pills. It’s about food, movement, and weight. Newer diabetes medications like SGLT2 inhibitors and GLP-1 agonists don’t just lower blood sugar-they directly protect your heart. Studies show they reduce heart failure and heart attack risk by 14% to 26% on top of glucose control. If you have diabetes, ask your doctor if one of these drugs is right for you.Weight, Movement, and Food: The Daily Choices That Matter
Obesity isn’t just about appearance. Excess fat-especially around your waist-triggers inflammation, raises blood pressure, worsens insulin resistance, and pushes cholesterol levels up. A waist measurement over 40 inches for men or 35 for women is a red flag. Physical inactivity is responsible for 6% of global heart disease cases. You don’t need to run a marathon. Just 150 minutes a week of brisk walking-about 30 minutes, five days a week-cuts your risk significantly. Take the stairs. Park farther away. Walk after dinner. These aren’t chores. They’re heart insurance. Diet matters more than you think. The WHO links unhealthy eating to 11 million deaths globally each year. That’s not just junk food. It’s too much salt, too much sugar, too much processed meat, and not enough vegetables, whole grains, nuts, and fish. The Mediterranean diet isn’t a trend. It’s backed by decades of research. Olive oil, beans, leafy greens, berries, fatty fish, and nuts-eaten regularly-lower inflammation, improve cholesterol, and reduce heart attacks. You don’t need to be perfect. Just shift your plate. More plants. Less processed stuff.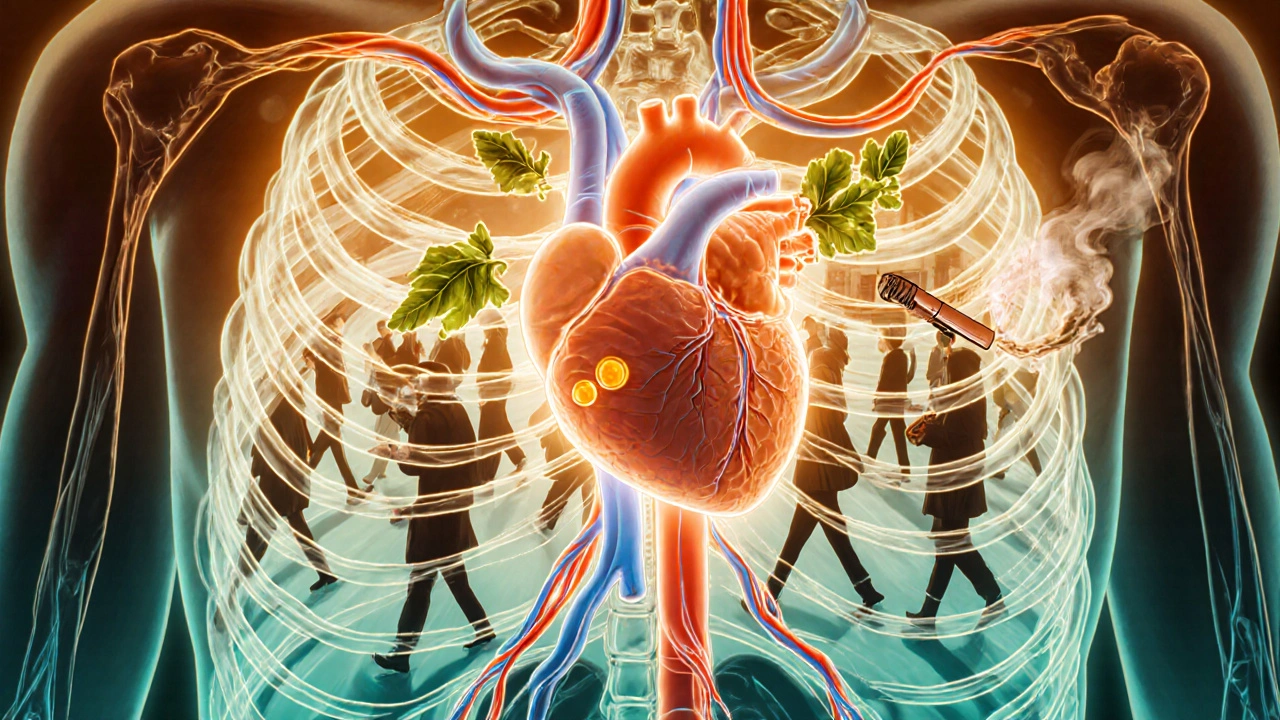
When Risk Factors Multiply
The biggest danger isn’t one risk factor. It’s the combo. High blood pressure + smoking + obesity? That’s not 30% + 50% + 40%. That’s an 8 to 10 times higher risk than having none. Dr. Spencer Kroll, a preventive cardiologist, puts it simply: “It’s not additive. It’s multiplicative.” One bad habit makes you vulnerable. Two? You’re in danger. Three? Your heart is under siege. That’s why comprehensive risk tools like the American College of Cardiology’s Pooled Cohort Equations exist. They don’t just list risks-they calculate your 10-year chance of a heart attack or stroke. If your score is above 20%, you’re in the high-risk zone. That’s when doctors recommend statins, blood pressure meds, and aggressive lifestyle changes.What You Can Do Right Now
You don’t need to fix everything at once. Start with one thing.- If you smoke? Call a quitline. Use nicotine patches. Ask for help. You’re not weak-you’re brave for trying.
- If your blood pressure is high? Get it checked weekly. Cut salt. Walk daily. Track your numbers.
- If you have family history? Get your cholesterol and glucose tested now. Don’t wait.
- If you’re overweight? Lose 5% of your body weight. That’s often enough to lower blood pressure and improve insulin sensitivity.
- If you’re unsure? Ask your doctor for a risk assessment. Bring your family history. Bring your questions.






Pranab Daulagupu
November 29, 2025 AT 23:09LDL particle size matters more than the total number. Most docs still miss this. ApoB testing is the real gold standard-way more predictive than LDL-C. If you're high risk, push for it.
Statins aren't the only game in town. PCSK9 inhibitors? Game-changer for familial hypercholesterolemia. Ask your cardiologist.
Also, don't ignore sleep apnea. It's a silent multiplier for hypertension and arrhythmias.
Matthew Stanford
November 30, 2025 AT 20:51My dad had his first MI at 51. I got my lipid panel at 32. Turned out my LDL was 190. Started on a low-dose statin, switched to Mediterranean diet, walking 6k steps daily.
Two years later? LDL at 78. BP normal. No symptoms. No panic. Just consistent action.
You don't need to be perfect. Just show up.
Olivia Currie
November 30, 2025 AT 21:26OMG I JUST REALIZED I’VE BEEN IGNORING MY BP FOR 3 YEARS 😭
Just checked at the pharmacy-142/91. I’m crying. I’m scared. But also… I’m DONE pretending this isn’t a problem.
Starting tomorrow: no more takeout, daily walks, and I’m booking that doctor’s appointment. I got this 💪❤️
Curtis Ryan
December 1, 2025 AT 16:02so i quit smoking 6 months ago and my doc said my risk is already down 40% like WHAT??
no joke i feel better, breathe better, and my wife says i dont smell like an ashtray anymore lol
if you smoke, just stop. even if you slip, just get back on. every day counts. ❤️
Rajiv Vyas
December 3, 2025 AT 02:09Heart disease? Nah. It's all Big Pharma and the FDA pushing statins so they can sell more pills.
My uncle was 72, never smoked, ate organic kale every day, dropped dead from a 'heart attack'-they never tested his heavy metal levels.
EMF from 5G, glyphosate in your coffee, and cholesterol is actually good for you. They just want you scared and medicated.
Diana Askew
December 3, 2025 AT 03:52Ugh. I knew this was gonna be one of those 'eat quinoa and meditate' posts.
Everyone's so obsessed with cholesterol like it's the devil. Have you heard of inflammation? Or gut health? Or how about just STOP TAKING SUGAR??
My cousin's LDL was 220 but her CRP was normal-she's fine. You people are obsessed with numbers, not health.
PS: If you're not taking magnesium, you're doing it wrong. 😒
King Property
December 5, 2025 AT 03:32You call that a comprehensive breakdown? Pathetic.
Where’s the data on trans fats? You didn’t mention endocrine disruptors in plastics. You skipped the role of chronic stress on cortisol-induced visceral fat. You didn’t even touch on the link between air pollution and endothelial dysfunction.
And you think a 150-minute walk fixes everything? Please. This is why people die-because they trust amateurs with half-baked advice.
Read the 2023 ESC Guidelines. Then come back.
Yash Hemrajani
December 6, 2025 AT 18:06Oh wow, another 'just walk more and eat olive oil' miracle cure. Let me guess-you also think brushing your teeth prevents diabetes?
Fact: 70% of people with heart disease have normal cholesterol.
Fact: The Framingham study was funded by the sugar industry.
Fact: You’re all just chasing numbers while ignoring the real culprit-chronic inflammation from processed carbs.
Try keto. Or fasting. Or just stop listening to cardiologists who get paid by pharma.
Also, your 'Mediterranean diet'? They eat lamb and olive oil. Not kale smoothies. 😏
Pawittar Singh
December 7, 2025 AT 11:10Y’all are overcomplicating this. My grandpa smoked till 80, ate fried chicken daily, never exercised. Lived to 94. So what’s the real story?
But here’s what I know: my mom had diabetes, high BP, and quit sugar. Lost 30 lbs. Now her A1c is 5.2. No meds.
So yes, genetics matter-but your choices matter MORE.
Start small. Drink water instead of soda. Walk after dinner. That’s it. You don’t need a PhD to save your heart. Just start.
And yes, I’m talking to YOU, Rajiv. Put the chips down. 😊❤️
Jacob Keil
December 8, 2025 AT 10:24Reality is a construct. The heart doesn't 'fail'-it surrenders to the illusion of time.
You think cholesterol is bad? It's just your body trying to patch the holes in your soul's architecture.
Statins are a band-aid on a collapsing cathedral.
The real risk? Living in fear of a number you can't even see.
Be still. Breathe. The heart knows what to do. You just stopped listening.
Also, I once ate a whole pizza and my BP dropped. Coincidence? Maybe. Or maybe the universe was whispering.
Trust the silence. Not the lab report.