Gallbladder Cancer Risk Calculator
Estimate Your Risk
Key Takeaways
- Gallstones increase the odds of gallbladder cancer, especially large or long‑standing stones.
- Cholesterol stones carry a higher cancer risk than pigment stones.
- Regular imaging (ultrasound or CT) can spot high‑risk stones before symptoms appear.
- Elective cholecystectomy reduces cancer risk for patients with chronic gallstone disease.
- Know the warning signs - persistent abdominal pain, jaundice, or unexplained weight loss - and seek prompt evaluation.
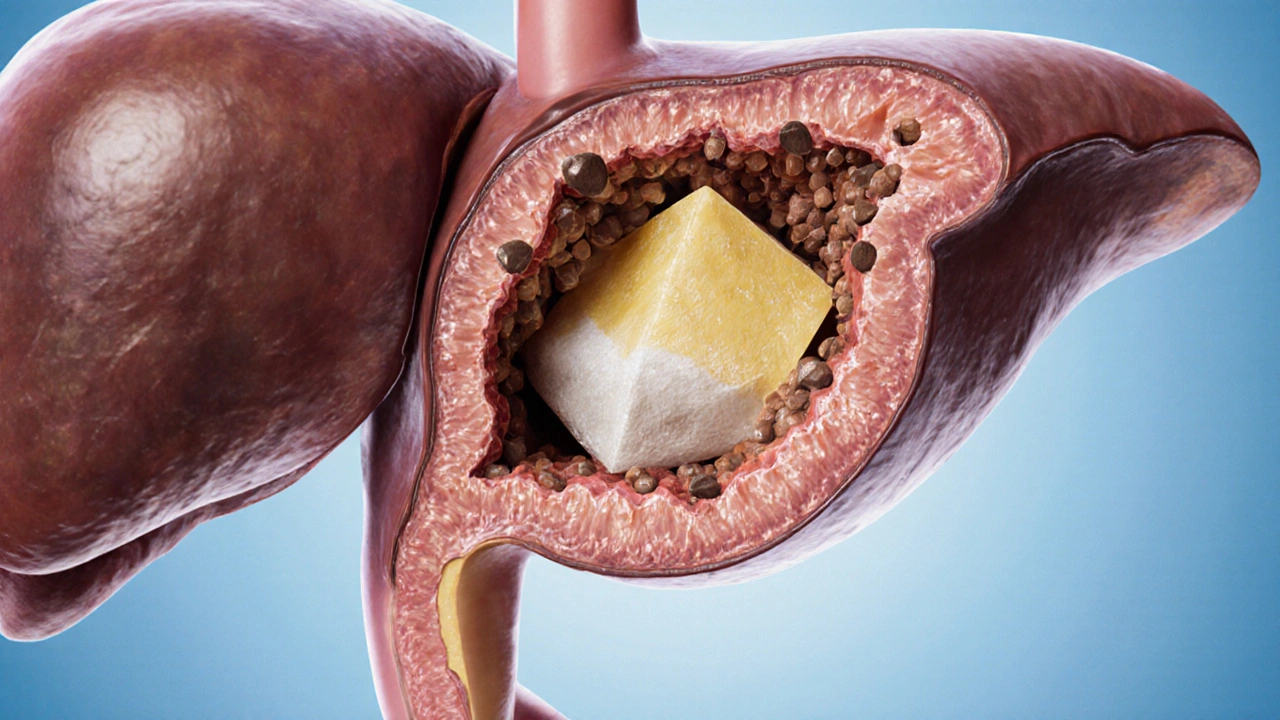
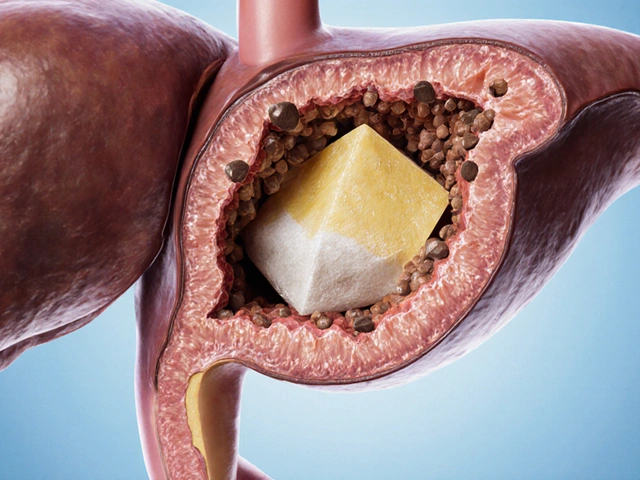
What Are Gallstones?
When gallstones are solid particles that form in the gallbladder from cholesterol, bilirubin, or a mix of both, they can range from tiny sand‑like grains to stones the size of a golf ball. Most people never notice them, but about 10‑15% of adults in Western countries develop stones at some point.
Understanding Gallbladder Cancer
While relatively rare, gallbladder cancer is one of the most aggressive biliary tract cancers. In the UK, the incidence is roughly 1.5 per 100,000 people each year, but mortality remains high because the disease often presents late.
How Gallstones Influence Cancer Risk
Researchers have tracked thousands of patients and found a clear pattern: the longer a stone stays in the gallbladder, the higher the chance that chronic irritation can trigger malignant changes. Key findings include:
- Patients with stones larger than 3cm have a 4‑6× higher risk of cancer compared with stone‑free individuals.
- Stone duration over 10years raises the risk by roughly 3×.
- Mixed‑type stones (cholesterol + pigment) sit in the middle of the risk spectrum.
This relationship is driven by chronic inflammation, bacterial overgrowth, and bile‑acid alterations that can damage the gallbladder lining.
Types of Gallstones and Their Cancer Profiles
Not all stones behave the same. Below is a quick comparison of the most common categories.
| Stone Type | Typical Composition | Average Size | Relative Cancer Risk |
|---|---|---|---|
| Cholesterol stones | 80‑90% cholesterol, some calcium bilirubinate | 0.5‑2cm (can grow >3cm) | High - up to 6× baseline |
| Pigment stones | Calcium bilirubinate, often black or brown | 0.2‑1cm | Low - 1‑2× baseline |
| Mixed stones | Combination of cholesterol and pigment | 1‑3cm | Moderate - 2‑3× baseline |
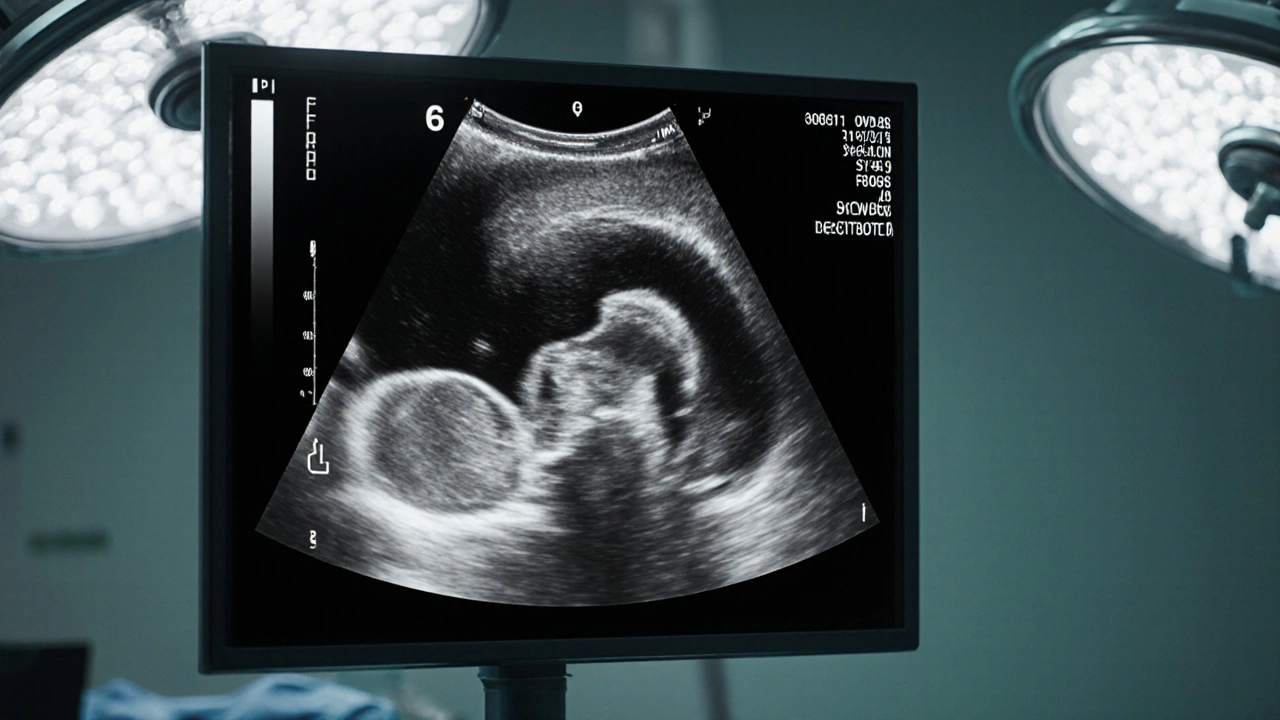
Diagnosing High‑Risk Gallstones
Early detection hinges on imaging. The two most common tools are:
- Ultrasound - a non‑invasive, bedside test that identifies stones, wall thickening, and polyps.
- CT scan - offers detailed cross‑sectional views, useful when ultrasound results are ambiguous or when complications are suspected.
When imaging shows stones larger than 3cm, gallbladder wall nodularity, or polyps over 1cm, clinicians often recommend further evaluation with magnetic resonance cholangiopancreatography (MRCP) or even diagnostic laparoscopy.
Managing Gallstones to Lower Cancer Risk
There are three main strategies:
- Watchful waiting - suitable for small, asymptomatic stones. Regular ultrasound every 1‑2years helps track growth.
- Medical dissolution - oral ursodeoxycholic acid can shrink cholesterol stones, but success rates hover around 40% and treatment may last 6‑24months.
- Surgical removal (cholecystectomy) - the definitive cure. Laparoscopic cholecystectomy reduces the long‑term cancer risk by up to 80% in patients with chronic stones.
For patients with risk factors such as diabetes, obesity (BMI>30), or a family history of gallbladder cancer, many surgeons advocate elective removal even if symptoms are mild.
Risk Factors Beyond the Stones Themselves
While stones are the primary trigger, several other elements heighten cancer odds:
- Gender - women are three‑times more likely than men.
- Age over 60years.
- Chronic infections with Salmonella or Helicobacter pylori.
- Genetic mutations in KRAS or TP53 pathways.
- High‑fat diet leading to supersaturated bile.
Addressing these factors-through weight management, smoking cessation, and controlling diabetes-complements any stone‑focused treatment plan.
When to See a Doctor
If you notice any of the following, schedule an appointment promptly:
- Persistent right‑upper‑quadrant pain lasting more than a few hours.
- Jaundice or dark urine.
- Unexplained weight loss or loss of appetite.
- Fever combined with abdominal pain (possible cholecystitis).
Early intervention can prevent the progression from benign stones to malignant disease.
Frequently Asked Questions
Do all gallstones lead to gallbladder cancer?
No. Most stones never cause cancer. The risk climbs with stone size, duration, and certain stone types-especially large cholesterol stones.
How often should someone with asymptomatic stones get screened?
A yearly or biennial ultrasound is generally advised for stones larger than 1cm, or for patients with additional risk factors like obesity or a family history of cancer.
Can lifestyle changes lower the chance of cancer if I already have stones?
Yes. Maintaining a healthy weight, eating a high‑fiber, low‑fat diet, and avoiding rapid weight‑loss diets can reduce bile supersaturation and inflammation, thereby lowering cancer risk.
Is laparoscopic cholecystectomy safe for older adults?
In most cases, yes. Modern minimally invasive techniques have low complication rates (<2%) even for patients over 70, and the procedure markedly cuts long‑term cancer risk.
What symptoms suggest a gallstone has become cancerous?
New‑onset jaundice, sudden weight loss, persistent pain that no longer follows meals, and a palpable gallbladder mass are red‑flag signs that warrant immediate imaging and specialist referral.





Ashika Amirta varsha Balasubramanian
October 14, 2025 AT 13:04Think of your gallbladder as a humble altar where bile rituals occur; when those stones accumulate, the altar becomes desecrated. I urge you to respect your body's signs and consider preventive checks before things spiral. Large cholesterol stones are like stubborn traditions that need breaking. Remember, proactive surgery can be a noble offering to your future self. Stay vigilant, stay healthy.
Jacqueline von Zwehl
October 15, 2025 AT 05:46It's essential to monitor stone size and duration; regular ultrasounds can catch changes early. Including everyone in these health conversations makes the journey less intimidating.
kathy v
October 16, 2025 AT 09:33Our great nation has always prided itself on robust health, yet we neglect the silent threat of gallstones that lurk within. The data is crystal clear: stones larger than three centimeters multiply cancer risk by up to six times, a statistic no patriot can ignore. When these formidable stones persist for a decade, the inflammatory cascade becomes a battlefield, eroding the gallbladder's defenses. Cholesterol stones, the most prevalent, embody this menace, demanding our immediate attention. While pigment stones pose a lesser threat, they are not innocuous and deserve scrutiny. The United States, with its cutting‑edge medical infrastructure, is uniquely positioned to implement nationwide screening initiatives. An annual ultrasound for high‑risk demographics could drastically reduce late‑stage diagnoses. Moreover, elective cholecystectomy-once viewed as a drastic step-now stands as a preventive triumph, slashing cancer odds by up to eighty percent. Yet, some still cling to the myth that “no symptoms, no problem,” a dangerous fallacy that fuels complacency. The modern diet, rich in saturated fats, worsens bile supersaturation, encouraging stone formation; we must champion dietary reforms alongside medical interventions. Obesity, diabetes, and familial cancer history amplify the peril, forming a trifecta of risk that cannot be dismissed. If we, as a society, prioritize weight management and glycemic control, we strike at the root of stone genesis. Let us also remember that early signs-persistent RUQ pain, jaundice, unexplained weight loss-are not mere inconveniences but urgent alarms. Prompt gastroenterology referrals upon these warnings can turn the tide. In sum, a coordinated effort blending lifestyle changes, vigilant imaging, and timely surgery will safeguard our populace from this stealthy adversary.
Jorge Hernandez
October 17, 2025 AT 13:20Yo fam 🙌 check those stone stats and don’t wait till you feel like a ticking bomb 😂 get an ultrasound and if it’s big go for the cholecystectomy 👍 stay safe
Michael Dion
October 18, 2025 AT 17:06Sounds like a waste of time
josh Furley
October 19, 2025 AT 20:53Look, the risk calculus is just a fancy way of saying “don’t be lazy”. Simple math: bigger stone = higher risk, longer exposure = higher risk. If you’re into jargon, think of it as an incremental hazard coefficient. So unless you enjoy gambling with your gallbladder, get it removed. 🤷♂️
Jacob Smith
October 21, 2025 AT 00:40Hey guys, this is super important! If u have big stones, u should def think bout getting it out. I mean, who wants cancer, right? Keep an eye on ur health and don’t ignore the signs.
sara vargas martinez
October 22, 2025 AT 04:26From a clinical perspective, the correlation between stone characteristics and malignancy is well‑documented. Larger stones (>3 cm) exert chronic mechanical irritation, promoting epithelial dysplasia. Prolonged stone presence (>10 years) amplifies inflammatory cytokine release, further destabilizing cellular homeostasis. Cholesterol‑rich stones harbor bile‑acid alterations that favor mutagenic pathways, whereas pigment stones, while less risky, still contribute to oxidative stress. Imaging modalities, particularly high‑resolution ultrasound, can quantify stone dimensions and monitor growth trajectories. When imaging reveals progressive enlargement or wall thickening, surgical consultation becomes imperative. Laparoscopic cholecystectomy, now a routine procedure, offers a definitive risk reduction, with meta‑analyses indicating up to an 80 % decrease in cancer incidence post‑removal. Lifestyle interventions-weight loss, reduced saturated fat intake, and glycemic control-serve as adjunctive measures to diminish stone formation. Patients with comorbidities such as diabetes or obesity should adopt a more aggressive surveillance schedule, ideally annual imaging. Early symptom recognition-persistent right‑upper‑quadrant discomfort, jaundice, or unexplained weight loss-should trigger immediate gastroenterological evaluation. Ultimately, a multidisciplinary approach integrating preventive imaging, surgical management, and lifestyle modification yields the best outcomes.
Amy Carpenetti
October 23, 2025 AT 08:13I think it’s wise to keep a balanced view; regular check‑ups are helpful, but not everyone needs surgery right away. Let’s support each other in making informed choices without fear‑mongering.
Carissa Engle
October 24, 2025 AT 12:00Frankly, this article suffers from a lack of precision; the risk factors are presented in a mélange of vague statements and half‑baked statistics. The stone‑size multiplier of “4‑6×” is thrown in without citation, and the duration factor is similarly nebulous. Moreover, the language vacillates between clinical jargon and layman explanations, betraying a lack of editorial rigor. The reader is left to decipher ambiguous risk thresholds, which is unacceptable in medical communication. It would be prudent to reference peer‑reviewed studies and provide confidence intervals rather than blanket multipliers. Also, the suggestion that “elective cholecystectomy reduces risk by up to 80%” requires a citation; otherwise, it reads as anecdotal hype. Overall, the piece needs a thorough rewrite, tightened structure, and evidence‑backed claims to be credible.
Mary Cautionary
October 25, 2025 AT 15:46Whilst the exposition is ostensibly comprehensive, one must lament the paucity of epistemological substantiation accompanying the purported risk coefficients. A scrupulous scholar would demand rigorous meta‑analytic corroboration before espousing such definitive clinical guidance.
Crystal Newgen
October 26, 2025 AT 18:33Interesting overview; I’ll keep it in mind.
Hannah Dawson
October 27, 2025 AT 22:20Let’s cut to the chase: the article’s over‑optimistic tone masks the harsh reality that many patients dismiss early symptoms until it’s too late. By downplaying the urgency of imaging for stones >1 cm, it indirectly encourages complacency. A more forthright approach would stress that proactive cholecystectomy isn’t merely an option but a necessity for high‑risk cohorts. Otherwise, we risk normalizing a dangerous delay.
Julie Gray
October 29, 2025 AT 02:06One cannot ignore the covert agenda behind the promotion of routine ultrasounds; hidden entities profit from the proliferation of diagnostic equipment. The emphasis on surgical removal conveniently aligns with pharmaceutical interests seeking post‑operative prescriptions. It is imperative to scrutinize these narratives and question who truly benefits from the purported health recommendations.
Victoria Guldenstern
October 30, 2025 AT 05:53Ah, the gallbladder saga-another fine illustration of how modern medicine loves to turn a simple pebble into a monster. One would think that a stone the size of a marble is a trivial inconvenience, yet the literature insists it’s a ticking time‑bomb awaiting a dramatic cancer debut. The supposed “risk calculator” sounds more like a carnival game than a scientific tool, sprinkling percentages with the same reckless abandon as a chef seasoning a stew. And let’s not forget the endless parade of lifestyle advice-cut the butter, jog more, pray harder-each dressed up as gospel truth. Meanwhile, the real culprit, the commercial interests behind imaging machines, sit back and smile. So, dear readers, perhaps the best advice is to keep a skeptical eye on every glossy recommendation and remember that sometimes, less is more, especially when it comes to unnecessary interventions.