Medication Safety Checker
Check Your Medication Safety
This tool helps you understand potential interactions between common medications. It's not medical advice—always consult your healthcare team.
Results
Dangerous Interaction Detected
This combination may cause:
- • Increased bleeding risk
- • Reduced effectiveness
- • Severe side effects
Next Steps
- • Contact your healthcare team within 24 hours
- • Ask about alternative medications
- • Request a medication therapy management session
No Serious Interactions Detected
This combination is generally safe when taken as prescribed.
Recommended Action
Continue your current regimen and schedule a routine medication review with your healthcare team.
Please Select Both Medications
To see potential interactions, please select two medications from the dropdown menus above.
When you’re taking multiple medications for chronic conditions, side effects don’t just happen in isolation-they stack up, overlap, and sometimes turn into emergencies. A dizziness from blood pressure medicine combined with fatigue from diabetes drugs can leave you falling at home. A stomach ache from an NSAID mixed with a blood thinner could mean internal bleeding. These aren’t rare cases. Medication side effect management is one of the most critical, yet overlooked, parts of modern healthcare. And it’s not something one doctor can fix alone.
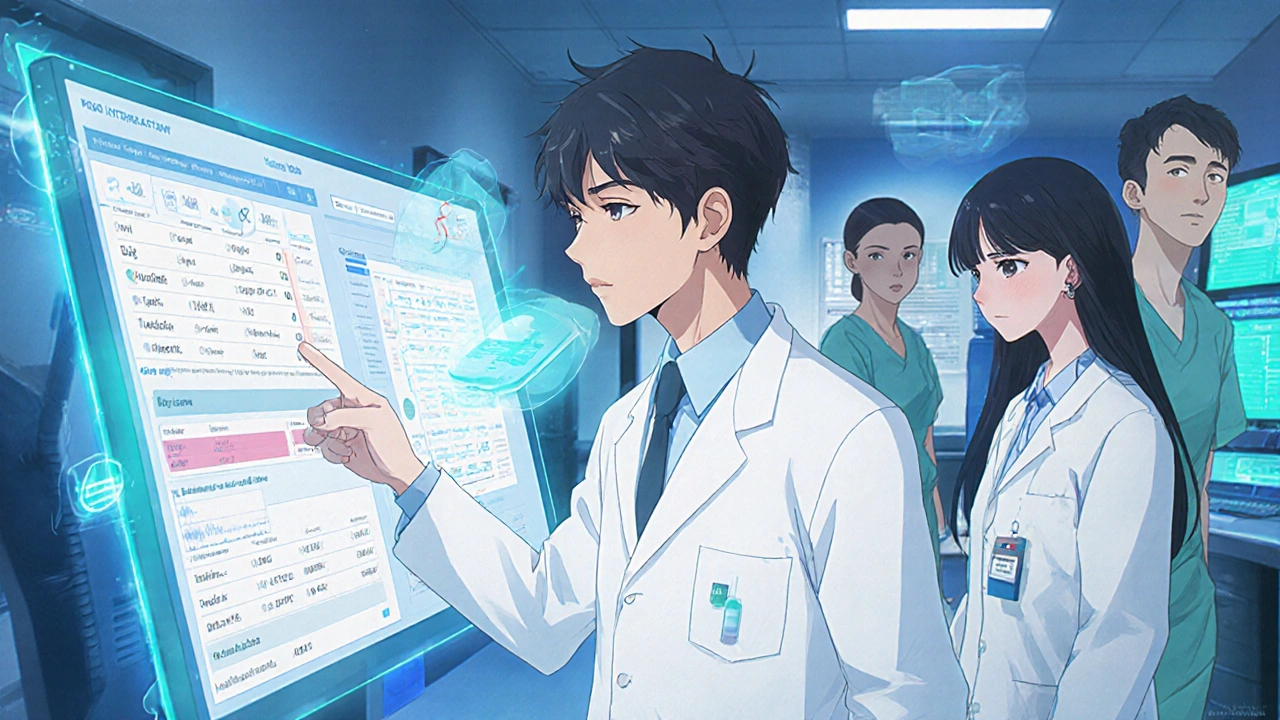
Why One Provider Can’t Handle It All
Think of your meds like a puzzle. Each pill has a purpose, but they also interact. A 2022 JAMA Internal Medicine study found that 67% of medication errors in hospitals were preventable-and nearly half of those came from missed drug interactions. That’s not because doctors are careless. It’s because no single provider has the time, training, or access to see the full picture. Doctors focus on diagnosis and treatment goals. Pharmacists? They live in the details of dosing, timing, interactions, and side effect profiles. Specialists bring in organ-specific risks-like how kidney function changes how you metabolize a drug, or how heart failure affects fluid balance with diuretics. When these roles work in silos, gaps open up. When they work together, those gaps close.How the Team Actually Works-Day to Day
In a well-run collaborative care model, pharmacists aren’t just filling prescriptions. They’re part of the care team. In U.S. hospitals, 78% of patients now have pharmacists joining daily rounds with doctors and nurses. That means the pharmacist walks into the room, sees your chart, and says: “This 72-year-old on warfarin just started amiodarone. That combo triples his bleeding risk. We need to switch to apixaban.” In primary care clinics, embedded pharmacists review every new prescription before it’s sent to the pharmacy. They flag things like:- Drug interactions (43% of patients on five or more meds have at least one high-risk interaction)
- Duplicate therapies (two different pills doing the same thing)
- Dosing errors in elderly patients
- Side effects that haven’t been reported by the patient
The Real Impact: Numbers That Matter
The data doesn’t lie. When pharmacists work directly with doctors and specialists:- Blood pressure control in high-risk groups jumped from 29% to 94% in a landmark NEJM study
- Hospital readmissions dropped by 23.1%
- Emergency visits fell by 15.7%
- Medication adherence improved by 22% because pharmacists asked patients: “What’s stopping you from taking this?” not “Why didn’t you take it?”
Where It’s Working Best
This isn’t theory. It’s happening right now-in integrated health systems, accountable care organizations, and even in CVS and Walgreens clinics. In 2024, 1,247 community pharmacies had pharmacists embedded in primary care teams. These aren’t just retail pharmacies-they’re clinical hubs. The strongest results come in managing:- Anticoagulants (warfarin, DOACs)
- Diabetes medications
- Heart failure drugs
- Psychiatric meds with complex side effects
What’s Holding It Back
It’s not a lack of evidence. It’s a lack of systems. Many doctors still see pharmacists as “pill counters.” Some pharmacists feel undertrained to speak up in clinical meetings. And reimbursement? A mess. Only 28 states reimburse Medicaid for pharmacist services. Medicare only started paying for comprehensive medication reviews in team-based settings in 2022. Most private insurers still don’t cover it. There’s also paperwork. One pharmacist in Ohio told me she spends 2.5 hours a day documenting interactions-time that could be spent talking to patients. “I saved a man from a GI bleed,” she said, “but I had to spend three hours just filling out forms to prove it.” And then there’s culture. A 2021 ASHP survey found 37% of pharmacists reported resistance from physicians. One doctor said, “I don’t need someone telling me how to prescribe.” But when that same doctor saw a pharmacist catch a dangerous interaction before the patient left the clinic, he changed his mind.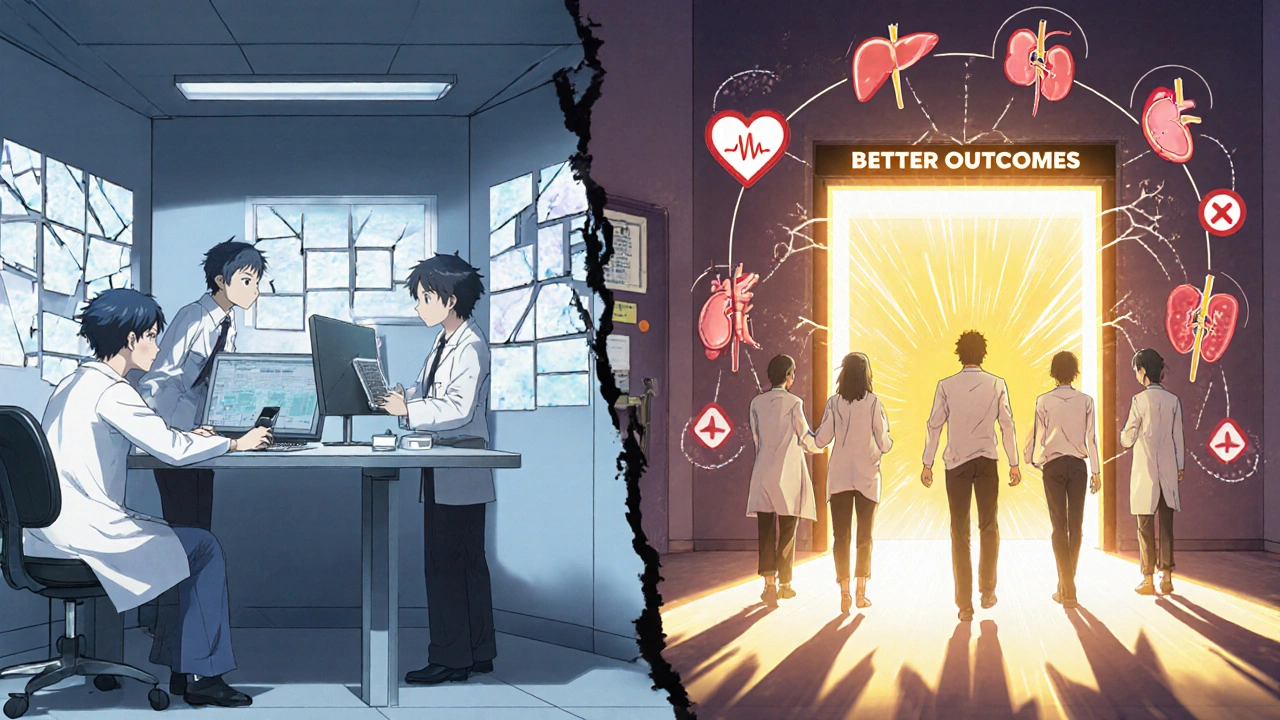
What Patients Can Do
You don’t have to wait for your clinic to adopt this model. You can push for it:- Ask your doctor: “Can I meet with the pharmacist to review all my meds?”
- Bring a full list of everything you take-including vitamins, supplements, and over-the-counter painkillers
- Ask: “Are any of these drugs known to cause dizziness, confusion, or fatigue together?”
- Request a medication therapy management (MTM) session. It’s free under Medicare Part D if you qualify.
The Future Is Team-Based
By 2030, 75% of U.S. primary care will likely use team-based models, according to the Institute for Healthcare Improvement. That’s not a prediction-it’s a necessity. With aging populations, more complex meds, and rising costs, we can’t afford to keep treating patients one pill at a time. The real win isn’t just fewer side effects. It’s better quality of life. Patients in collaborative care models report 18.7% higher satisfaction. They feel heard. They feel safe. They know someone is watching out for the hidden dangers between their prescriptions. This isn’t about replacing doctors. It’s about giving them the right partner. And that partner? Often, it’s the pharmacist standing at the counter-not just handing out pills, but helping you live better.Can pharmacists really change my medication without my doctor’s approval?
In most cases, no-unless they have a formal collaborative practice agreement (CPA) with your doctor. These agreements, now legal in 48 states, let pharmacists adjust doses, switch meds, or order labs under specific conditions. But even without a CPA, pharmacists can recommend changes to your doctor. Many clinics now have standing orders where the pharmacist’s suggestion goes directly to the doctor’s inbox for approval within 24 hours.
What if my doctor doesn’t want to work with a pharmacist?
You can still ask for a medication review. Many community pharmacies offer free Medication Therapy Management (MTM) sessions under Medicare Part D. You can also request a referral to a clinical pharmacist through your insurance. If your doctor resists, ask for a second opinion or look for a clinic that already has pharmacists embedded-many ACOs and VA facilities do. Your safety matters more than tradition.
Are pharmacist-led side effect interventions proven to work?
Yes. A 2019 NEJM study showed pharmacist-led care improved blood pressure control from 29% to 94% in African-American men with uncontrolled hypertension. Another study in Diabetes Care found collaborative teams improved HbA1c by 1.2% more than standard care. In anticoagulation clinics, pharmacist management reduced major bleeding events by 31%. These aren’t small gains-they’re life-saving.
Do I need to pay extra for pharmacist collaboration?
Not if you’re on Medicare Part D-you’re entitled to a free Medication Therapy Management session if you take multiple chronic disease meds. Many private insurers now cover pharmacist services under value-based care contracts. In states with Medicaid reimbursement, services are free. Even in places without direct billing, community pharmacies often offer free reviews as part of their clinical services. Ask before you assume it costs money.
How do I find a clinic with a collaborative care team?
Look for clinics affiliated with hospitals, accountable care organizations (ACOs), or large pharmacy chains like CVS MinuteClinic or Walgreens Healthcare Clinics. These places are far more likely to have embedded pharmacists. You can also call your local pharmacy and ask: “Do you have a clinical pharmacist who works with doctors on medication reviews?” If they say yes, schedule a time. If they say no, ask if they plan to start. Demand creates change.





Robin Johnson
November 24, 2025 AT 03:12My grandma was on seven meds and kept falling. No one ever connected the dots until her pharmacist sat down with her and said, 'You're on three drugs that make you dizzy.' They swapped one out, cut the dose on another, and now she walks without a cane. This isn't rocket science-it's basic care.
Latonya Elarms-Radford
November 25, 2025 AT 14:09Let’s be real-modern medicine has become a grotesque symphony of pharmaceutical band-aids, each one playing a different note in a dissonant, profit-driven orchestra. The doctor, the pharmacist, the specialist-they’re all just cogs in a machine that treats symptoms like inventory and patients like data points with a pulse. We’ve outsourced healing to algorithms and formularies, and now we’re surprised when the body rebels? The real tragedy isn’t the side effects-it’s that we’ve stopped seeing the human behind the prescription.
Mark Williams
November 26, 2025 AT 18:30HL7 FHIR integration is the unsung hero here. Real-time EHR interoperability enables pharmacists to detect polypharmacy risks with >90% accuracy in high-risk cohorts. The 22% adherence bump? That’s not motivational talking-it’s structured MTM with behavioral nudges tied to refill patterns and lab trends. We’re talking clinical decision support at the point of dispensing, not just pill counting.
David Cunningham
November 28, 2025 AT 02:36Aussie pharmacies have been doing this for years. My old man’s on warfarin and his pharmacist calls him every week to check INR, adjusts dose if needed, and texts him if his meds run low. No drama. No waiting. Just good care. Why can’t the US just copy this?
luke young
November 29, 2025 AT 12:46I love this. My mom’s doctor finally let the pharmacist tweak her diabetes meds after she kept fainting. Turned out it was the combo with her blood pressure pill. They switched her to something gentler and now she’s got energy again. Just needed someone to listen.
james lucas
December 1, 2025 AT 08:11soooo many people dont even know their meds are interacting and its crazy. i had a friend who was on 8 pills and she thought her brain fog was just stress. pharmacist found she was double-dosing on benzos and her kidney was failing. she cried. we all cried. this needs to be standard. not a luxury.
Jessica Correa
December 3, 2025 AT 05:18My dad’s pharmacist noticed he wasn’t taking his statin because it gave him muscle pain so they switched him to ezetimibe and now he’s fine. No hospital stay. No drama. Just someone who actually asked him how he felt. Why isn’t this normal everywhere
manish chaturvedi
December 3, 2025 AT 06:57In India, we often rely on pharmacists for basic medical advice because doctors are overburdened. A trained pharmacist can catch a dangerous interaction before it harms a patient. This model is not just effective-it is essential, especially in resource-constrained settings. The West is catching up to what many developing nations have practiced out of necessity.
Michael Fitzpatrick
December 5, 2025 AT 05:20I used to think pharmacists just handed out pills. Then my sister got hospitalized from a drug interaction no one caught. Now I make sure every time she gets a new script, we sit down with the pharmacist. They see things doctors don’t have time for. It’s not magic-it’s just care. And honestly, it’s the most important part of the whole system.
Justin Daniel
December 5, 2025 AT 12:40Oh cool, so now the pharmacist is the new doctor? Next they’ll be doing surgeries and writing prescriptions. Just kidding. But seriously, if your doctor thinks they know everything about your meds without talking to the pharmacist who actually knows the pharmacokinetics, maybe you need a new doctor.
Melvina Zelee
December 6, 2025 AT 15:38my pharmacist once asked me why i skipped my med and i said i was scared of the side effects and she just smiled and said 'lets fix that' not 'why didnt you take it' like my doc does. that one conversation changed everything. i feel seen now. like my fears matter. not just my numbers.