Quick Summary
- ocular hypertension is high intraocular pressure without detectable eye damage.
- Common causes include genetics, steroid use, and systemic hypertension.
- Most people feel no symptoms; regular eye exams catch it early.
- Treatment ranges from daily eye‑drops to laser therapy and surgery.
- Monitoring IOP and lifestyle tweaks can keep the pressure in check.
What Is Ocular Hypertension?
Ocular hypertension is a condition where the intraocular pressure (IOP) exceeds the normal range (typically >21 mmHg), but without any measurable damage to the optic nerve or visual field loss.
It’s often called a “silent pressure rise” because most people don’t notice any change in vision. The key concern is that untreated ocular hypertension can progress to primary open‑angle glaucoma, the leading cause of irreversible blindness worldwide.
How Intraocular Pressure Works
Intraocular pressure is the fluid pressure inside the eye, maintained by the production and drainage of aqueous humor.
Aqueous humor is produced by the ciliary body at a rate of about 2.5µL/min and drains through the trabecular meshwork into Schlemm’s canal. When drainage is impaired or production is excessive, pressure builds up.
Normal IOP hovers between 10-21mmHg. Values above this threshold, especially sustained elevations, increase stress on the optic nerve head.
Primary Causes and Risk Factors
Several factors can push the pressure up:
- Genetic predisposition: Family history triples the risk of developing ocular hypertension.
- Steroid exposure: Topical, inhaled or systemic steroids raise IOP in up to 30% of users.
- Thin corneas: Central corneal thickness below 520µm can mask true IOP readings.
- Age: Prevalence climbs from 2% in people under 40 to 7% after age 70.
- Systemic hypertension and diabetes both correlate with higher ocular pressures.
Other contributors include certain eye‑drop preservatives, eye trauma, and anatomical variations like a crowded anterior chamber angle.
Symptoms-or Lack of Them
Because the optic nerve is still intact, ocular hypertension rarely produces noticeable symptoms. Some patients report occasional eye discomfort, halos around lights, or mild headache, but these are nonspecific.
The absence of symptoms underscores why routine eye exams are essential. Detecting the pressure rise early gives you a chance to intervene before any irreversible damage occurs.
How It’s Diagnosed
Diagnosis combines pressure measurement with structural and functional testing.
- Tonometry measures IOP. The Goldmann applanation tonometer remains the gold standard, reading pressure in mmHg.
- Visual field test (standard automated perimetry) checks for blind spots that would signal early glaucoma.
- Retinal nerve fiber layer (RNFL) imaging, often via OCT, assesses the thickness of nerve fibers around the optic disc.
If IOP is high but visual fields and RNFL are normal, the clinician records ocular hypertension and schedules follow‑up monitoring.

When Ocular Hypertension Becomes Glaucoma
Glaucoma is a group of eye diseases characterized by progressive optic nerve damage, often linked to elevated IOP.
Primary open‑angle glaucoma (POAG) is the most common form and typically follows a long‑standing ocular hypertension. In contrast, angle‑closure glaucoma involves a sudden blockage of aqueous outflow and requires emergency care.
Understanding the transition helps you appreciate why controlling pressure early matters.
Treatment Options: From drops to surgery
Therapy aims to lower IOP to a safe target-usually 20% below the baseline reading, or under 18mmHg for high‑risk patients.
| Treatment | Mechanism | Typical IOP Reduction | Key Considerations |
|---|---|---|---|
| Prostaglandin analogs | Increase uveoscleral outflow | 20‑30% | Once‑daily, may cause iris darkening |
| Beta‑blocker drops | Reduce aqueous production | 15‑25% | Contra‑indicated in asthma, bradycardia |
| Selective laser trabeculoplasty (SLT) | Enhances trabecular meshwork drainage | 25‑35% | Outpatient, effect lasts 3‑5years |
| Trabeculectomy | Creates a new drainage pathway | 30‑50% | Invasive, risk of infection & bleb failure |
**Prostaglandin analogs** (e.g., latanoprost) are usually first‑line because of strong efficacy and simple dosing. If drops aren’t enough or cause side effects, doctors may recommend SLT, a quick laser session that avoids daily medication.
When medication and laser fail to reach target pressure, surgical options like trabeculectomy become necessary. Newer minimally invasive glaucoma surgeries (MIGS) are also emerging but are less common for pure ocular hypertension.
Monitoring and Lifestyle Adjustments
Even after treatment starts, ongoing monitoring is crucial.
- Schedule IOP checks every 3-6months, more often if pressure fluctuates.
- Annual visual field and RNFL scans help catch early glaucomatous changes.
- Stay consistent with eye‑drop schedules; missing doses can cause pressure spikes.
Lifestyle tweaks can complement medical therapy:
- Regular aerobic exercise (e.g., brisk walking) may lower IOP by 2-4mmHg.
- Limit caffeine to under 200mg per day; high intake can temporarily raise pressure.
- Protect eyes from trauma-use safety glasses during sports.
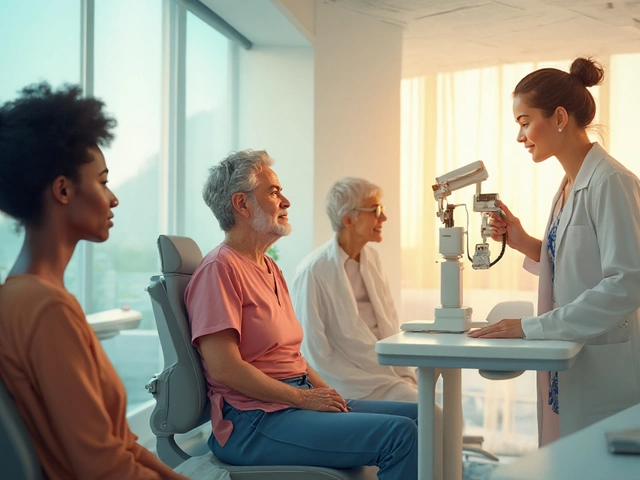
Where to Get Help
Early detection hinges on professional eye care.
Optometrist is often the first point of contact, performing routine screenings and referring high‑risk patients to an ophthalmologist for advanced testing.
Choosing an experienced ophthalmologist-especially one specializing in glaucoma-ensures you receive up‑to‑date treatment options.
Next Steps for Readers
If you’re over 40, have a family history of glaucoma, or use steroid medications, book a comprehensive eye exam within the next month.
During the visit, ask the clinician to:
- Measure your intraocular pressure with Goldmann applanation tonometry. \n
- Perform an OCT scan of the retinal nerve fiber layer.
- Discuss whether prophylactic eye‑drops or laser therapy is appropriate for your risk profile.
Staying informed and proactive is the best defense against vision loss.
Frequently Asked Questions
Can ocular hypertension cause any pain?
Usually no. Most people feel nothing at all. If you experience persistent eye pain, redness or halos, it could indicate a different issue like angle‑closure glaucoma and you should seek urgent care.
How often should I have my eye pressure checked?
If you’ve been diagnosed with ocular hypertension, aim for every 3-6months. If you’re at low risk and have normal readings, an annual exam is usually sufficient.
Are eye drops the only treatment?
No. While prostaglandin analogs are first‑line, laser trabeculoplasty and surgical options like trabeculectomy are viable when drops don’t achieve target pressure or cause side effects.
Can lifestyle changes lower my eye pressure?
Yes. Regular aerobic exercise, moderate caffeine intake, and maintaining a healthy weight have all been shown to modestly reduce IOP. However, lifestyle alone rarely replaces medication or laser therapy for high pressures.
Is there a genetic test for ocular hypertension?
Research is ongoing, but no single commercial genetic test reliably predicts ocular hypertension. Family history remains the strongest hereditary indicator.
Will my eyesight improve if I lower my eye pressure?
Lowering pressure can halt further damage, but it won’t restore vision already lost to glaucoma. Early treatment aims to preserve the vision you still have.





Rene Lacey
September 24, 2025 AT 07:54Ocular hypertension, while often overlooked, provides a fascinating case study in how subtle physiological imbalances can presage more serious neuro-ophthalmic conditions.
When intraocular pressure creeps above the conventional threshold of 21 mmHg, the aqueous humor dynamics reveal a delicate equilibrium between production and outflow that is easily perturbed.
Genetics, steroid exposure, and even systemic hypertension each tilt this balance, and the literature suggests a polygenic component that we are only beginning to decode.
The silent nature of the disease underscores the epistemological lesson that absence of evidence is not evidence of absence, particularly in sensory organs shielded from conscious perception.
From a clinical perspective, the Goldmann applanation tonometer remains the gold standard, yet newer non-contact methods challenge its supremacy in certain populations.
Researchers have documented that corneal thickness can mask true pressure readings, prompting a reevaluation of diagnostic cutoffs for individuals with pachymetry anomalies.
Moreover, the correlation between ocular hypertension and primary open-angle glaucoma is not deterministic; longitudinal studies reveal a conversion rate that varies widely with age, ethnicity, and baseline IOP.
Consequently, the decision to initiate prophylactic therapy should be grounded in a risk calculus that incorporates optic nerve head imaging and visual field stability.
Prostaglandin analogs, with their once-daily dosing and robust efficacy, exemplify how pharmacodynamics can be harnessed to augment uveoscleral outflow.
Yet, the side‑effect profile-including iris pigmentation changes-reminds us that therapeutic interventions are never without trade‑offs.
Laser trabeculoplasty offers a non‑pharmacologic alternative, delivering a modest IOP reduction that can persist for several years, though patient selection remains key.
In cases refractory to drops and laser, surgical avenues such as trabeculectomy or minimally invasive glaucoma surgeries provide substantial pressure drops but demand meticulous postoperative care.
Lifestyle modifications, such as regular aerobic exercise and caffeine moderation, have been shown to produce modest IOP reductions, reinforcing the biopsychosocial model of disease management.
Ultimately, the prudent clinician must adopt a vigilant monitoring schedule-ideally every three to six months-to detect any insidious progression toward glaucomatous damage.
In sum, ocular hypertension serves as a microcosm of preventive medicine: early detection, individualized risk assessment, and a balanced therapeutic armamentarium together safeguard visual function.
OKORIE JOSEPH
October 4, 2025 AT 17:54If you think high eye pressure is harmless you’re dead wrong
Lucy Pittendreigh
October 15, 2025 AT 03:54People should stop ignoring silent diseases and actually go for regular exams
Nikita Warner
October 25, 2025 AT 13:54Regarding the points raised earlier, it is advisable to schedule tonometry and OCT imaging at least twice a year for patients with IOP consistently above 22 mmHg.
Annual visual field testing helps catch early glaucomatous changes that might otherwise be missed.
If the patient is using topical steroids, a taper or substitution with non‑steroidal anti‑inflammatory agents can mitigate pressure spikes.
In cases where prostaglandin analogs provoke ocular surface irritation, switching to a preservative‑free formulation often restores comfort while maintaining efficacy.
Finally, patient education on the importance of adherence cannot be overstated; missed doses are a common cause of unexpected pressure elevations.
Liam Mahoney
November 4, 2025 AT 22:54Look you think a one‑sentence warning is enough? Get real and see a doc before your eyes start ringing
surender kumar
November 15, 2025 AT 08:54Oh great, another post telling us to walk more. As if a daily jog will magically fix a pressure problem that’s rooted in genetics and steroids.
Justin Ornellas
November 25, 2025 AT 18:54Actually, the sentence you just wrote contains a subject‑verb agreement error – “walk more” should be followed by “will” not “will magically”. Proper grammar matters even in casual discourse.
JOJO Yang
December 6, 2025 AT 04:54They don’t tell you that the government hides the real cure for eye pressure and pushes expensive drops just to make money!!
Faith Leach
December 16, 2025 AT 14:54Exactly, the pharma giants are in cahoots with the health agencies – the “laser” they promote is just a distraction while the real solution is a simple herbal rinse they suppress.
Eric Appiah Tano
December 27, 2025 AT 00:54Everyone, keep in mind that staying informed, following up with your eye doctor, and supporting each other makes the journey easier. You’ve got this!