Antipsychotic Decision Aid Tool
Patient Assessment
Key Takeaways
- Clozapine is the most effective drug for treatment‑resistant schizophrenia but requires strict blood monitoring.
- Risperidone, Olanzapine, Quetiapine and Aripiprazole are commonly used first‑line alternatives with easier safety profiles.
- Each drug balances efficacy against side‑effects like metabolic syndrome, extrapyramidal symptoms, or agranulocytosis.
- Choosing the right antipsychotic depends on prior treatment response, comorbid health issues, and patient preference.
- Regular labs, dose titration, and patient education are essential no matter which medication you start.
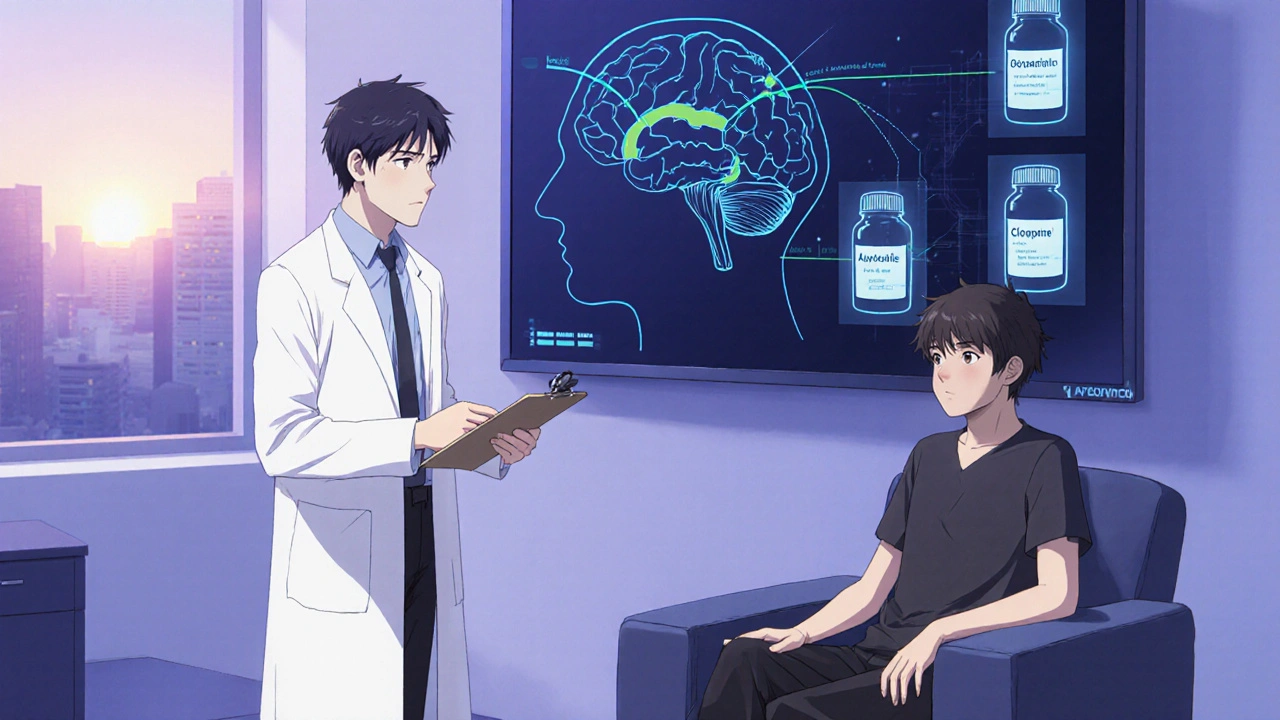
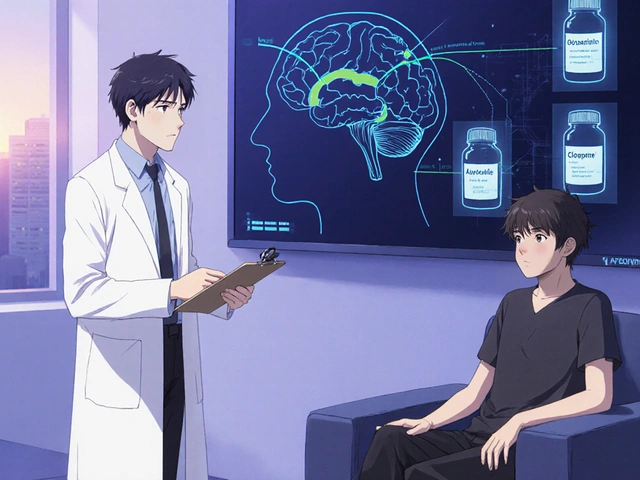
When a psychiatrist says, “You need a stronger pill,” they’re usually referring to patients whose schizophrenia hasn’t improved after two or three standard antipsychotics. Clozapine is a second‑generation antipsychotic that shines in this tough‑to‑treat group, but it’s not the only option on the table. This guide walks through the science, safety, and practical steps for comparing Clozapine with its most popular alternatives - Risperidone, Olanzapine, Quetiapine and Aripiprazole - so you can decide which drug fits a given clinical picture.
What Makes Clozapine Unique?
Clozapine was approved in the 1970s and earned a reputation as the go‑to treatment for Treatment‑Resistant Schizophrenia (TRS). Its strengths lie in:
- High affinity for dopamine D2 receptors combined with serotonin 5‑HT2A antagonism, delivering robust symptom control.
- Proven superiority in reducing suicidal behavior in schizophrenia patients.
- Effectiveness against both positive (hallucinations, delusions) and negative (flat affect, social withdrawal) symptom clusters.
But the drug carries a serious safety signal: agranulocytosis - a potentially fatal drop in white blood cells. Because of this, patients must enroll in a mandatory blood‑monitoring program, checking weekly for the first six months, then bi‑weekly, and eventually monthly if counts stay stable.
First‑Line Alternatives: An Overview
Before moving to Clozapine, most clinicians try one of the following newer atypical antipsychotics. They share a similar mechanism - blocking dopamine and serotonin receptors - but differ in potency, tolerability, and metabolic impact.
Risperidone is often the first choice for acute psychosis because it works quickly and has a relatively clean metabolic profile.
Olanzapine offers strong symptom relief but is notorious for weight gain and lipid rise.
Quetiapine is praised for its sedative effect, making it useful when insomnia co‑exists.
Aripiprazole works as a dopamine partial agonist, reducing the risk of movement disorders while still controlling psychosis.
Side‑Effect Profiles at a Glance
| Drug | Typical Dose (mg/day) | Key Efficacy | Major Safety Concerns | Monitoring Needs |
|---|---|---|---|---|
| Clozapine | 200‑600 | Best for TRS, reduces suicidality | Agranulocytosis, myocarditis, metabolic syndrome | Weekly CBC ×6 mo, then bi‑weekly/monthly |
| Risperidone | 2‑6 | Rapid control of positive symptoms | Prolactin elevation, EPS (high dose) | Baseline labs; prolactin if symptoms |
| Olanzapine | 10‑20 | Strong overall symptom reduction | Weight gain, diabetes, dyslipidemia | Weight/BMI, fasting glucose, lipids every 3 mo |
| Quetiapine | 300‑800 | Good for agitation, sleep disturbances | Sedation, orthostatic hypotension | Blood pressure, sedation scale |
| Aripiprazole | 10‑30 | Effective with low EPS risk | Akathisia, insomnia | Monitor for restlessness, sleep pattern |

How to Choose: Decision Factors for Clinicians and Patients
Picking the right antipsychotic isn’t a one‑size‑fits‑all exercise. Consider these five dimensions:
- Prior Treatment Response: If two different atypicals have already failed, Clozapine becomes the evidence‑based next step.
- Medical Comorbidities: Diabetes or heart disease tips the scale toward drugs with lighter metabolic impact (e.g., Aripiprazole).
- Side‑Effect Tolerance: Patients who hate weight gain may avoid Olanzapine, while those sensitive to sedation might skip Quetiapine.
- Monitoring Capacity: Clozapine’s blood work demands a clinic with lab access; rural settings might favor Risperidone.
- Patient Preference: Engaging the individual in shared decision‑making improves adherence, regardless of drug choice.
Practical Steps to Initiate Clozapine Safely
Because of the agranulocytosis risk, Clozapine initiation follows a strict protocol. Below is a concise checklist.
- Confirm diagnosis of Treatment‑Resistant Schizophrenia (failure of ≥2 antipsychotics at adequate dose/duration).
- Obtain baseline CBC, liver function, cardiac exam, and fasting glucose.
- Enroll the patient in a certified Clozapine registry (e.g., UK’s Clozapine Monitoring Service).
- Start at 12.5 mg once or twice daily; increase by 25‑50 mg every other day to target 300‑450 mg, adjusting for tolerability.
- Monitor CBC weekly for the first 6 months; hold dose if absolute neutrophil count (ANC) < 1500/mm³.
- Educate patient on infection signs, fever, and the need for immediate medical attention.
Switching From an Alternative to Clozapine (or Vice‑versa)
Transitioning between antipsychotics requires overlap to prevent relapse.
- Maintain current drug at therapeutic dose.
- Introduce Clozapine at low dose while gradually tapering the previous medication over 1‑2 weeks.
- Watch for additive side‑effects (e.g., excessive sedation when combining Quetiapine with Clozapine).
- Re‑assess labs 1 week after each dose increase.
- Document any emergent symptoms and adjust titration speed accordingly.

When Alternatives May Outperform Clozapine
Even though Clozapine holds the efficacy crown for TRS, real‑world scenarios sometimes favor a different drug.
- Short‑Term Acute Crisis: Rapid‑acting Risperidone or Olanzapine IM/IV formulations can calm severe agitation faster than titrating Clozapine.
- Pregnancy: Data on Clozapine’s safety in pregnancy remain limited; many clinicians opt for Quetiapine, which has more pregnancy‑category data.
- Severe Metabolic Risk: Patients with pre‑existing obesity or diabetes may benefit from Aripiprazole’s neutral weight profile.
Real‑World Patient Stories (Illustrative)
Case 1 - Sarah, 28, TRS: After failing Risperidone, Olanzapine, and Quetiapine, her psychiatrist started Clozapine. Within 8 weeks, her PANSS score dropped 30 %, and she reported fewer auditory hallucinations. Weekly CBCs were uneventful, and she now enjoys stable employment.
Case 2 - Mark, 45, early‑stage schizophrenia: He presented with mild psychosis and a history of type 2 diabetes. The team chose Aripiprazole, avoiding further metabolic strain. Six months later his HbA1c remained unchanged, and his symptoms were well‑controlled.
Bottom Line: Matching Drug to Patient
Think of antipsychotic selection as a balance sheet. Clozapine offers the highest efficacy for those who truly need it, but the bookkeeping includes weekly blood tests and vigilant monitoring. First‑line alternatives provide easier logistics and fewer severe adverse events, making them the default for most patients.
When you sit down with a patient, run through the five decision factors, weigh the pros and cons in a simple table, and involve the person in the choice. That collaborative approach leads to better adherence, fewer relapses, and ultimately a higher quality of life.
What is the main advantage of Clozapine over other antipsychotics?
Clozapine is the only medication that consistently improves symptoms in patients who have not responded to at least two other antipsychotics, and it uniquely reduces suicide risk in schizophrenia.
How often does a patient need blood work while on Clozapine?
Weekly complete blood counts (CBC) are required for the first six months, then every two weeks for the next six months, and finally monthly if the absolute neutrophil count stays above 1500 /mm³.
Which alternative antipsychotic has the lowest risk of weight gain?
Aripiprazole typically has a neutral impact on weight and metabolic markers, making it the preferred option for patients with obesity or diabetes.
Can Clozapine be used during pregnancy?
Evidence is limited, and the drug is classified as a pregnancy‑category C medication. Most clinicians avoid it unless the benefits clearly outweigh the potential risks.
What should I do if my patient develops a fever while on Clozapine?
A fever could signal agranulocytosis or myocarditis. Stop Clozapine immediately, obtain an urgent CBC and cardiac enzymes, and refer to emergency care.





Kathrynne Krause
October 21, 2025 AT 17:21Picture this: a patient finally finds relief after months of dead‑end meds – that’s the Clozapine story in a nutshell. It’s the gold standard for those stubborn cases, cutting hallucinations like a hot knife through butter, while also lowering the risk of suicide. Think of it as the superhero cape of antipsychotics, but it demands a secret identity: weekly blood draws. The trade‑off is worth it when the alternative is perpetual psychosis. 🌈
Chirag Muthoo
October 23, 2025 AT 19:21According to the established protocol, a baseline complete blood count, liver function tests, and fasting glucose must be obtained prior to initiation. The patient should then be enrolled in a certified monitoring registry, with weekly CBCs for six months, followed by bi‑weekly assessments, and ultimately monthly surveillance provided counts remain stable. Documentation of informed consent is essential, as is patient education regarding signs of infection.
Ivan Laney
October 26, 2025 AT 02:54When deliberating the optimal antipsychotic regimen, one must first acknowledge the heterogeneity of schizophrenia phenotypes, which range from predominantly positive symptomatology to a blend of negative and cognitive deficits. Clozapine, possessing a unique receptor affinity profile, penetrates this spectrum with unparalleled efficacy, yet its pharmacodynamic complexity mandates a rigorous safety net. The agranulocytosis risk, while statistically low, presents a non‑negligible mortality hazard, compelling clinicians to implement a tiered monitoring schedule that escalates in frequency during the induction phase. Simultaneously, metabolic sequelae such as weight gain and dyslipidemia require periodic anthropometric and laboratory evaluations, lest the therapeutic gains be offset by cardiovascular compromise. In contrast, risperidone offers a rapid onset of action with a modest metabolic footprint, though its propensity for prolactin elevation can precipitate galactorrhea or sexual dysfunction in susceptible individuals. Olanzapine, while delivering robust symptom control, is notorious for inducing profound adiposity and insulin resistance, thereby necessitating lifestyle counseling and periodic HbA1c monitoring. Quetiapine’s sedative properties render it advantageous for comorbid insomnia, yet orthostatic hypotension can be problematic in older adults, demanding careful titration and positional awareness. Aripiprazole’s partial dopamine agonism confers a lower extrapyramidal symptom burden, but clinicians must remain vigilant for emergent akathisia, which can be distressing if unaddressed. Moreover, the pharmacokinetic interactions of each agent with concurrent medications, such as CYP450 inducers or inhibitors, must be charted meticulously to avoid subtherapeutic exposure or toxicity. Patient preference, an often underappreciated variable, should be integrated through shared decision‑making, acknowledging concerns about weight, bloodwork, and dosing frequency. Accessibility to reliable laboratory services further stratifies drug choice; rural settings may favor agents with minimal monitoring requirements. Economic considerations, including insurance formularies and out‑of‑pocket costs, also influence adherence and long‑term outcomes. Ultimately, the clinician’s role is to synthesize these multidimensional factors-efficacy, safety, comorbidity, logistics, and patient values-into a personalized treatment algorithm that maximizes functional recovery while minimizing adverse effects.
John Price
October 27, 2025 AT 19:34That’s a solid overview, keep the first dose low and go slow.
Jake Hayes
October 29, 2025 AT 04:54While the summary is thorough, oversimplifying dose titration often leads to unnecessary side‑effects; precision matters.
Vivian Annastasia
October 31, 2025 AT 06:54Oh great, another drug that promises miracles but comes with a side‑effect package that could rival a fast‑food menu.
Dana Yonce
November 1, 2025 AT 10:41Totally get you 😅 some meds do feel like a trade‑off but the right balance can really help.
Lolita Gaela
November 3, 2025 AT 04:21From a pharmacodynamic standpoint, clozapine’s high affinity for D2, 5‑HT2A, and α1‑adrenergic receptors underpins its superior efficacy in treatment‑resistant schizophrenia, yet its propensity to induce agranulocytosis is mediated by nitrenium ion formation and subsequent neutrophil apoptosis. Consequently, the implementation of a robust hematologic surveillance protocol is non‑negotiable to mitigate idiosyncratic neutropenia.
Casey Cloud
November 4, 2025 AT 16:27Here’s a quick cheat sheet for starting clozapine first get CBC baseline then enroll patient in a monitoring program weekly labs for six months then biweekly up to a year and monthly after stable keep an eye on weight lipids glucose and watch for fever or signs of infection stop the drug if ANC drops below 1500
parbat parbatzapada
November 5, 2025 AT 23:01Yo man u think they just wanna keep us on cheap pills while they hide the real cure lol the pharma bigshots dont want u to know aboot the secret protocol they silencd the docs who speak truth
Giusto Madison
November 7, 2025 AT 19:27Listen up, teammate – the key to staying on track is consistency. Set a weekly reminder for your labs, log any side‑effects in a journal, and bring that notebook to every appointment. If you feel shaky or notice a fever, call your doc immediately. You’ve got this, and we’ll fine‑tune the dose together.
Xavier Lusky
November 9, 2025 AT 10:21Don't be fooled by the "coach" narrative; the monitoring system is a front for data collection and control, and any delay in reporting could be used against you.