Key Takeaways
- Effective response hinges on rapid surveillance, clear legal authority, and pre‑positioned vaccines and antivirals.
- International coordination with bodies like the World Health Organization the global forum that sets standards for disease reporting and emergency declarations speeds resource sharing.
- Public communication that is transparent, consistent, and culturally tuned reduces panic and improves vaccine uptake.
- Low‑income governments can achieve high impact by focusing on targeted vaccination and leveraging regional stockpiles.
- A ready‑to‑execute checklist cuts decision‑making time from weeks to days.
When a new wave of influenza a respiratory virus that causes seasonal flu and can mutate into pandemic‑capable strains starts to reappear, the pressure on national leaders spikes. The stakes are higher than they were a decade ago: more travel, denser cities, and a broader range of animal reservoirs. This article walks you through what a modern government response influenza looks like, from the first lab signal to the rollout of vaccines, and shows how policies can be fine‑tuned for different resource levels.
Understanding Reemerging Influenza
Reemergence means a strain that was thought to be under control resurfaces with renewed transmissibility. The 2024 H3N2‑like wave in Southeast Asia, for example, combined genetic elements from the 2009 pandemic virus and recent avian isolates, leading to a 15% rise in hospital admissions compared with the prior season. Surveillance data from the surveillance system a network of laboratories, sentinel physicians, and electronic reporting tools that tracks infection rates in near real‑time flagged the surge three weeks before the first deaths were reported.
Why do these spikes happen? Viral drift, changes in animal farming practices, and waning immunity after a quiet season all play a part. Recognizing the biological drivers helps governments decide whether to launch a containment or mitigation strategy.
Core Government Responsibilities
Government the national authority that creates health regulations, allocates funding, and coordinates emergency actions responsibilities fall into six pillars.
- Early Detection. Deploy surveillance system upgrades that integrate genomic sequencing, sewage testing, and syndromic data. Real‑time dashboards cut reporting lag to 48hours.
- Vaccine Procurement & Distribution. Maintain a vaccine stockpile a reserve of seasonal and, when available, matched pandemic influenza vaccines stored under cold‑chain conditions sufficient for at least 20% of the population within the first month of a declared outbreak.
- Antiviral Reserves. Keep an antiviral stockpile pre‑positioned supplies of neuraminidase inhibitors and newer baloxavir formulations that can be dispensed to high‑risk groups quickly with clear guidelines for distribution.
- Legal Framework. Issue emergency health orders that grant authorities the power to enforce quarantine, close schools, or restrict mass gatherings. Laws must be transparent to avoid constitutional challenges.
- Funding Mechanisms. Activate pre‑approved contingency budgets that cover vaccine purchase, laboratory expansion, and public messaging campaigns. Flexible finance reduces the bureaucratic gap between decision and action.
- Public Communication. Launch a centralized information hub that delivers daily updates, explains risk levels, and counters misinformation. Messages should be translated, use trusted spokespersons, and include simple actions such as “wash hands for 20 seconds”.
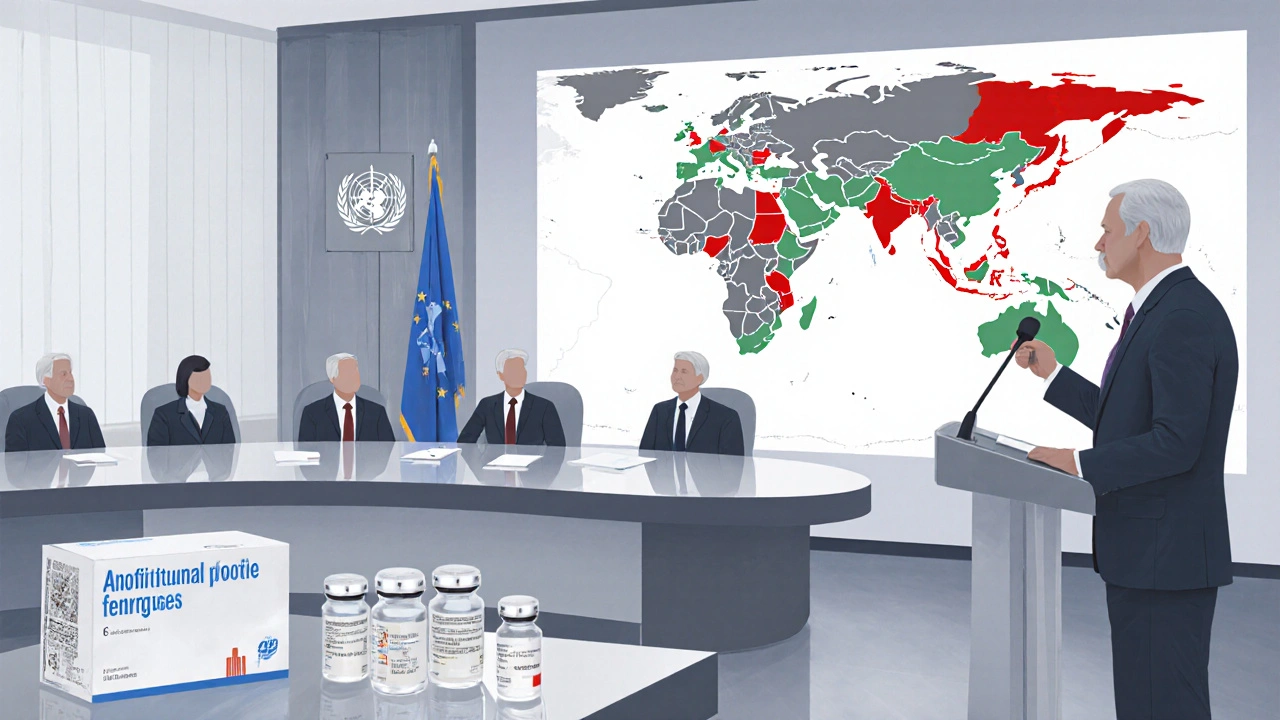
International Coordination
No country fights an influenza resurgence alone. The World Health Organization the United Nations agency that declares Public Health Emergencies of International Concern and coordinates global vaccine allocation issues Situation Reports that guide national thresholds for travel advisories and resource sharing.
Regional alliances, like the European Centre for Disease Prevention and Control (ECDC) or the African Union’s Africa Centres for Disease Control, provide pooled procurement platforms. During the 2023 H5N1 bird‑flu spillover, the EU’s joint procurement secured 40million doses of a candidate vaccine within two months, a speed that single‑nation contracts could not match.
Effective liaison teams should have liaisons stationed at WHO regional offices, maintain a real‑time line of communication with the Centers for Disease Control and Prevention the U.S. federal agency that offers technical guidance, laboratory support, and field epidemiology expertise, and participate in the Global Influenza Surveillance and Response System (GISRS) to share viral isolates.
Case Studies: Lessons from Recent Waves
2009 H1N1 Pandemic - The UK’s fast‑track vaccine approval process cut the rollout time from 6months to 8weeks, but insufficient public communication led to vaccine hesitancy in several regions.
2018 H3N2 Resurgence in South America - A robust surveillance system flagged the strain early, yet limited antiviral stockpiles forced clinicians to rely on supportive care, increasing ICU admissions by 12%.
2023 H5N1 Egg‑Farm Outbreak in the Netherlands - Coordinated travel restrictions, combined with immediate culling and targeted vaccination of poultry workers, prevented human spillover. The rapid legal order to close live‑bird markets was critical.
2025 Reemergence of a drifted H1N2 strain in the United Kingdom - A pre‑approved contingency fund allowed the health ministry to purchase 5million doses of a quadrivalent vaccine within 48hours of WHO’s alert. Transparent daily briefings kept the public calm and vaccine uptake reached 78% among eligible adults.
Practical Checklist for Decision‑Makers
- Activate the national influenza response plan within 24hours of the first laboratory‑confirmed case.
- Verify that the surveillance system is ingesting data from hospitals, primary care, and labs.
- Consult the World Health Organization risk assessment to determine if a Public Health Emergency of International Concern (PHEIC) is declared.
- Mobilize the vaccine stockpile for high‑risk groups (elderly, pregnant women, chronic disease patients).
- Distribute antiviral stockpile to regional hospitals with dosage guidelines.
- Issue a legal order that defines quarantine zones, school closures, and workplace safety standards.
- Release the first public briefing: explain the virus, outline protective steps, and announce vaccine availability dates.
- Unlock contingency funding to cover logistics, communication, and any procurement gaps.
- Schedule a mid‑response review after two weeks to adjust strategies based on case trends.

Comparison of Response Approaches
| Aspect | Containment | Mitigation |
|---|---|---|
| Goal | Stop virus spread at source | Reduce severe outcomes while accepting some spread |
| Key Tools | Strict quarantine, rapid contact tracing, localized school closures | Widespread vaccination, public‑health messaging, antiviral distribution |
| Resource Needs | High staffing for tracing, legal enforcement capacity | Large vaccine & antiviral stockpiles, robust communication channels |
| Typical Use | Early, low‑case numbers, well‑defined clusters | Widespread community transmission, limited tracing ability |
| Economic Impact | Localized but intense short‑term disruptions | Broader but flatter impact over longer period |
Common Pitfalls & Pro Tips
Pitfall 1 - Delayed data sharing. Some regional labs still use paper reports, adding days to the detection timeline. Tip: Mandate electronic reporting with API endpoints linked to the national dashboard.
Pitfall 2 - Legal ambiguity. Vague emergency powers invite court challenges that stall action. Tip: Draft clear, time‑bound statutes that specify conditions for travel bans and school closures.
Pitfall 3 - Vaccine hesitancy. A lack of trusted messengers fuels rumors. Tip: Engage community leaders, faith‑based groups, and local clinicians early in the communication plan.
Pitfall 4 - Funding bottlenecks. Waiting for parliamentary approval can waste weeks. Tip: Set aside a pre‑approved emergency fund that can be accessed with a single ministerial sign‑off.
Frequently Asked Questions
How quickly should a government start vaccinating after an outbreak is detected?
Ideally within 48hours of a WHO PHEIC declaration, targeting high‑risk groups first. Early rollout curbs hospital overload and boosts public confidence.
What legal instruments enable mandatory quarantine?
Most countries rely on public‑health acts that grant ministers power to issue enforceable quarantine orders. The law must specify duration, appeal processes, and compensation for affected individuals.
Can low‑income nations afford a vaccine stockpile?
Pooling resources through regional agreements or the WHO’s COVAX‑like mechanisms allows shared procurement, reducing per‑country costs while ensuring access during emergencies.
What role does travel restriction play in modern influenza control?
Travel bans can delay spread by weeks, buying time for vaccine distribution. However, they must be evidence‑based; blanket bans often cause economic harm without substantial epidemiological benefit.
How should governments handle misinformation during an outbreak?
Deploy a rapid‑response digital team that monitors social platforms, debunks false claims within hours, and partners with trusted media outlets. Transparency about uncertainties reduces speculation.
By treating influenza as a recurring public‑health emergency rather than a seasonal inconvenience, governments can protect lives, keep economies moving, and build trust that lasts beyond the next wave.







Mark Haycox
October 13, 2025 AT 15:28Our gov should put America first in the flue fight, no overseas labs dictating our vaccine strategy.
Michael Taylor
October 13, 2025 AT 16:16The roadmap laid out in this piece shines a hopeful light on what many fear to be an endless battle against ever‑mutating flu strains! By embracing rapid surveillance, governments can catch the tiniest viral whisper before it crescendos into a full‑blown outbreak, and that is something to celebrate. Moreover, the call for pre‑positioned vaccine stockpiles reads like a promise that our most vulnerable citizens will not be left awaiting miracles. When leaders act with clarity, the public feels a reassuring sense of security, and that feeling fuels cooperation on a massive scale. The article’s emphasis on transparent communication means that rumors will drown in facts, which is precisely the kind of narrative we need in today’s information‑driven world. International coordination, as highlighted, turns isolated nations into a united front, and such solidarity can turn the tide of any health crisis. The checklist approach effectively translates lofty policy ideas into actionable steps, ensuring that bureaucratic inertia does not stall progress. Even low‑income countries can achieve impressive outcomes by focusing on targeted vaccination, proving that resource constraints are not an excuse for inaction. Legal authority, when clearly defined, empowers health officials to enact necessary measures without getting tangled in endless court battles. The inclusion of funding mechanisms guarantees that money will flow where it is needed most, bypassing the dreaded budgetary gridlock. Public health messaging that is culturally tuned not only respects diversity but also maximizes uptake, a win‑win for everyone involved. Learning from past case studies, such as the 2009 H1N1 response, provides valuable lessons that can be applied again and again, refining our collective memory. The article wisely points out that travel restrictions can buy precious weeks, and those weeks can be the difference between a manageable surge and a catastrophic overload. Antiviral stockpiles, as described, offer a critical line of defense for high‑risk groups, ensuring that treatment is not delayed until it is too late. Overall, the comprehensive strategy laid out feels like a blueprint for resilience, one that can be adapted to any emerging respiratory threat. So let us rally behind these recommendations, confident that with foresight and cooperation, future flu waves will meet a prepared and steadfast world!
Troy Brandt
October 13, 2025 AT 17:06I really appreciate the optimism in the previous comment, and I wonder how we can translate that energy into concrete training programs for local health workers.
One practical step could be a mentorship model where experienced epidemiologists pair with regional lab technicians, fostering skill transfer.
Another idea is to develop community‑focused simulation drills that rehearse both surveillance reporting and emergency communication.
These drills, if run quarterly, would keep everyone sharp and ready to act before the virus gains momentum.
Moreover, integrating real‑time data dashboards into daily briefings would empower decision‑makers with up‑to‑date information, reducing the lag that often hampers response.
Finally, celebrating small wins-like a rapid detection of a new strain-can boost morale and reinforce the collaborative spirit that underpins a successful outbreak response.
Angelo Truglio
October 13, 2025 AT 18:13Honestly, this whole "global coordination" narrative reeks of complacency-why should we hand over our sovereignty to distant bureaucrats?!
Our nation’s health should never be subjected to the whims of the WHO, whose priorities often mirror political agendas rather than scientific truth.
We must demand that any foreign‑sourced vaccine be subjected to our own rigorous testing before it ever reaches our citizens!
Only then can we claim that we are truly protecting the people, not merely bowing to international pressure.
Do not be fooled by glossy press releases; real safety comes from relentless scrutiny!
And remember, a country that cedes control will inevitably lose its edge in any future pandemic battle :)
Dawn Midnight
October 13, 2025 AT 19:20The previous comment contains several grammatical inaccuracies that need correction.
Firstly, the phrase "why should we hand over our sovereignty" should be followed by a question mark, not an exclamation point.
Secondly, "their" was used where "they're" would be appropriate when referring to the WHO’s priorities.
Finally, the term "glossy press releases" is correct, but the verb "are" should agree with the plural subject "press releases".
These adjustments will enhance clarity and professionalism.
frank hofman
October 13, 2025 AT 20:26yeah, this whole "pre‑positioned stockpile" thing is kinda overrated 🙄
i mean, why lock up doses when you can just order them on the fly? lol
the gov's gotta stop pretending they're the only ones who know how to handle flu 😏
maybe we should just let market forces do their thing, right? 😂
if that means we get the latest meds faster, I'm all for it.
Michael AM
October 13, 2025 AT 21:33I see where you're coming from.
Market forces can be fast, but they also leave gaps.
People need reliable access, not just the cheapest option.
Balancing speed with equity is key.
Erica Ardali
October 13, 2025 AT 22:40What we are witnessing, dear interlocutors, is not merely a procedural checklist but a profound testament to humanity's ceaseless pursuit of existential security.
In the grand tapestry of public health, each thread-be it surveillance, vaccination, or communication-interweaves with philosophical significance, echoing the age‑old dialectic between fate and agency.
To ignore the ethical imperatives embedded within these policies would be to surrender to a nihilistic void where disease reigns unchecked.
Thus, the elegance of a pre‑emptive vaccine stockpile transcends logistics; it becomes a moral monument to foresight, a beacon against the encroaching darkness of pandemics.
When governments articulate transparent narratives, they do more than inform-they sculpt collective consciousness, forging trust as a bulwark against fear.
Consequently, the very act of allocating contingency funds assumes a Platonic form, embodying the ideal of the good within the realm of public policy.
Let us, therefore, elevate our discourse beyond mere proceduralism, embracing the sublime responsibility to steward life itself.
Only then can we claim that we have not merely reacted to influenza, but that we have risen to confront the very notion of vulnerability with dignified resolve.
Justyne Walsh
October 13, 2025 AT 23:46Ah, the lofty rhetoric continues, draped in pseudo‑philosophy as if words alone could inoculate a nation.
Meanwhile, the very same governments parade half‑baked plans while grandstanding on moral high grounds that conveniently align with nationalist fantasies.
One would expect a genuine commitment to public welfare, not a self‑congratulatory parade of buzzwords and empty promises.
Perhaps the next checklist will include a clause for “self‑congratulation” on how well we avoided responsibility.
Ironically, the true patriotism lies in admitting our shortcomings and fixing them, not in shouting about it from the rooftops.
So spare us the dramatics and let the data speak louder than any nationalistic bravado.
Callum Smyth
October 14, 2025 AT 00:53Let's keep the conversation constructive and focus on actionable steps 😊
We can all agree that transparency and rapid response are essential, regardless of rhetoric.
Perhaps a joint working group could blend the philosophical vision with pragmatic implementation.
By combining expertise from diverse regions, we ensure solutions are both inclusive and effective.
Looking forward to collaborative progress!