When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version-and you expect it to be safe. But how does the FDA make sure that’s true after the drug hits the market? The answer isn’t simple. It’s not just a one-time approval. It’s an ongoing, high-stakes watch system that tracks millions of patients, analyzes hundreds of thousands of reports, and digs into manufacturing details-all to catch problems before they hurt people.
Why Safety Monitoring Matters More for Generics
Generic drugs make up 90% of all prescriptions filled in the U.S. But they’re not tested the same way as brand-name drugs before they’re approved. Brand-name drugs go through years of clinical trials with thousands of patients. Generics? They’re approved based on bioequivalence studies-usually with just 24 to 36 healthy volunteers. That’s enough to prove the drug works the same way in the body. But it’s not enough to catch every possible side effect.Here’s the problem: a rare allergic reaction, a weird interaction with another medication, or a slow buildup of a toxic impurity might not show up in a small, short-term study. Those risks only appear when thousands, even millions, of people take the drug over months or years. That’s why the FDA doesn’t stop watching once the pill hits the shelf. The real job begins after approval.
The FDA’s Safety Network: FAERS, Sentinel, and More
The FDA doesn’t rely on one tool. It uses a whole system. The biggest piece is the FDA Adverse Event Reporting System (FAERS). This is a giant database where doctors, pharmacists, patients, and drug companies report side effects, allergic reactions, or unexpected outcomes. In 2022, FAERS received over 2 million reports. Not all of them are about generics-but the FDA pulls out the ones that are.But reports alone aren’t enough. People don’t always report side effects. Studies suggest only 1% to 10% of serious reactions ever make it into FAERS. That’s why the FDA also runs the Sentinel Initiative. Launched in 2008 and expanded under the 21st Century Cures Act, Sentinel taps into real-time health data from over 100 million patients across hospitals, clinics, and insurance systems. It doesn’t wait for someone to file a report. It scans electronic records for patterns-like a sudden spike in kidney problems among people taking a specific generic blood pressure drug.
Then there’s the Office of Generic Drugs (OGD) and the Office of Pharmaceutical Quality (OPQ). These teams don’t just sit back. They actively dig into data. They look at manufacturing changes, impurity levels, and even tiny differences in inactive ingredients. A generic drug might have a different dye or filler than the brand version. Most of the time, it doesn’t matter. But sometimes, it does. A patient with a rare allergy to a specific dye might react only to one generic version-and not the others. Sentinel and FAERS help catch those signals.
Manufacturing Checks: The Hidden Layer of Safety
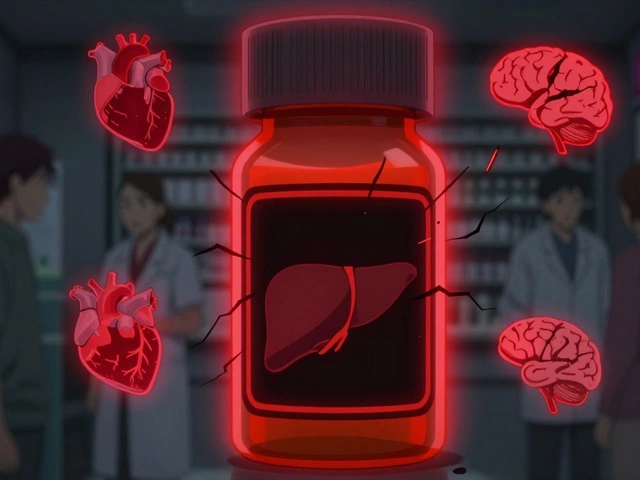
A drug can be perfectly formulated, but if it’s made in a dirty factory, it’s dangerous. That’s why the FDA inspects drug plants-both in the U.S. and overseas. In 2022, they conducted about 1,200 inspections in the U.S. and 600 abroad. Many are unannounced. Inspectors don’t just check paperwork. They look at how raw materials are stored, how equipment is cleaned, and whether quality control tests are accurate.One big concern: impurities. Even tiny amounts of unwanted chemicals can build up over time. The FDA sets strict limits. If a generic manufacturer’s drug has a new impurity that wasn’t in the brand version, the FDA can demand changes-or pull the product. The Office of Pharmaceutical Quality handles this. They work with toxicologists and chemists to evaluate whether an impurity is safe, using lab studies, computer models, and published research.
This is especially critical for complex generics-like inhalers, injectables, or long-acting pills. A small change in how the drug is released can affect how it works in the body. The FDA has been tightening its rules on these since GDUFA III took effect in 2023.
How the FDA Decides When to Act
Finding a signal is just the first step. The FDA has to decide if it’s real-and serious enough to act. Their team meets regularly in the OGD Clinical Safety and Surveillance Committee. Doctors, pharmacists, data scientists, and chemists review all the evidence: FAERS reports, Sentinel alerts, inspection findings, and even patient complaints on social media.If they find a pattern-say, three times more liver damage than expected with a specific generic statin-they dig deeper. They might ask the manufacturer for more data. They might order a new study. Or they might just flag it for closer monitoring.
If the risk is confirmed, the FDA has tools:
- Update the drug’s label to warn doctors and patients
- Send a “Dear Healthcare Provider” letter alerting prescribers
- Require the manufacturer to change the formula or manufacturing process
- Issue a voluntary recall
- In rare cases, pull the drug off the market
Since 2016, the 21st Century Cures Act made this process more formal. The FDA now has legal requirements to monitor safety after approval-not just as a best practice, but as a duty.
What’s Still Missing
The system works better than it did 20 years ago. But it’s not perfect. Experts point to two big gaps.First, underreporting. If a patient feels dizzy after taking a generic and doesn’t tell their doctor, it never gets recorded. If a doctor assumes it’s just aging and not the drug, it gets missed. The FDA knows this. That’s why they use data mining to find hidden patterns-not just wait for reports.
Second, complex generics. Inhalers, nasal sprays, topical creams-these are harder to prove are truly equivalent. A tiny difference in how the drug is delivered can change how much gets into the bloodstream. The FDA is working on better testing methods, but it’s slow. The Pew Charitable Trusts found in 2021 that monitoring for these products still lags behind simple pills.
And then there’s the sheer volume. About 1,000 new generic drugs get approved each year. That’s a lot of new products to track. The FDA’s user fee system, funded by generic manufacturers, brings in about $65 million a year to help pay for this work. But as more complex drugs enter the market, the demand for better data tools keeps growing.
What You Can Do
You don’t need to be a scientist to help. If you notice something unusual after starting a new generic drug-like unexplained fatigue, rash, or mood changes-tell your doctor. Ask if it could be related to the medication. If your doctor doesn’t know, ask them to report it through MedWatch, the FDA’s reporting portal.And if you’re switching between generic brands and notice a difference in how you feel, write it down. Note the name of the manufacturer on the bottle. That detail matters. The FDA can’t fix a problem if they don’t know which version caused it.
Most generics are safe. They’ve saved billions in healthcare costs and helped millions get the medicine they need. But safety isn’t a one-time check. It’s a constant conversation between patients, doctors, manufacturers, and regulators. The FDA doesn’t just approve drugs. It watches them-every day, every week, every year.
Are generic drugs less safe than brand-name drugs?
No, generic drugs are not less safe. The FDA requires them to be bioequivalent to the brand-name version and to meet the same strict manufacturing standards. The main difference is that generics aren’t tested on thousands of patients before approval. Instead, the FDA uses post-market systems like FAERS and Sentinel to catch rare or long-term side effects after the drug is widely used. The safety profile of a generic drug is monitored just as closely as a brand-name drug-just in a different way.
Can different generic brands of the same drug cause different side effects?
Yes, sometimes. While all generics must contain the same active ingredient in the same amount, they can use different inactive ingredients-like fillers, dyes, or coatings. For most people, this doesn’t matter. But for someone with a rare allergy or sensitivity, one brand might cause a reaction while another doesn’t. If you notice a change in how you feel after switching generic brands, note the manufacturer’s name and tell your doctor. This helps the FDA identify patterns and take action if needed.
How does the FDA know if a generic drug has a safety problem?
The FDA uses multiple sources: reports from patients and doctors through MedWatch/FAERS, real-time health data from the Sentinel Initiative, inspections of manufacturing plants, and data mining for unusual patterns. If a specific generic drug shows a spike in liver damage, kidney issues, or allergic reactions compared to others in its class, the FDA investigates. They look at the manufacturer, the formulation, and whether the problem is isolated or widespread.
What happens if a generic drug is found to be unsafe?
If a safety issue is confirmed, the FDA can require the manufacturer to update the drug’s label with new warnings, send a letter to doctors alerting them to the risk, or ask the company to change how the drug is made. In serious cases, the FDA can order a voluntary recall. Very rarely, if the risks outweigh the benefits, the drug is pulled from the market entirely. These actions are rare-most issues are caught early and fixed before they affect many people.
How often does the FDA inspect generic drug factories?
The FDA inspects about 1,200 domestic and 600 foreign generic drug factories each year. Many inspections are unannounced to catch real-world conditions. Inspectors check everything from how raw materials are stored to whether lab tests are accurate. These inspections are a key part of ensuring quality and safety-not just for the active ingredient, but for the entire manufacturing process.
What’s Next for Generic Drug Safety
The FDA’s goal is to cover 100 million patient records with Sentinel by 2025. That means even rarer side effects will be easier to spot. They’re also improving how they analyze data-using AI to find hidden patterns in millions of reports faster than humans can. And with more complex generics entering the market, the agency is developing new testing methods to ensure these drugs work the same way every time.The system isn’t perfect. But it’s far more advanced than it was a decade ago. And it’s the reason millions of Americans can trust their generic prescriptions-whether they’re taking a $5 blood pressure pill or a $100 cancer treatment.




Oladeji Omobolaji
January 22, 2026 AT 16:07Been on a generic statin for years. Never had an issue, but I did switch brands once and felt weirdly tired for a week. Didn’t think much of it till I read this. Now I check the manufacturer on the bottle like it’s a barcode. Weird how something so small can make a difference.
Janet King
January 24, 2026 AT 15:05The FDA’s post-market surveillance system is a critical component of public health infrastructure. While generic drugs are required to demonstrate bioequivalence, the reliance on passive reporting systems such as FAERS is inherently limited by underreporting. The Sentinel Initiative represents a significant advancement in proactive pharmacovigilance through real-world data aggregation. Continued investment in these systems is essential to maintain public trust.
Andrew Smirnykh
January 26, 2026 AT 10:52I’ve lived in three countries and taken generics everywhere. In the U.S., I trust them. In India, I was nervous. In Germany, they were almost brand-name in packaging. It’s not just about the science-it’s about culture, regulation, and history. The FDA’s system is one of the best, but it’s not the only way. Other countries do it differently. Maybe we can learn from them.
Sue Stone
January 28, 2026 AT 09:14My grandma switched to a new generic blood pressure med and started falling. Not because it didn’t work-because she got dizzy. She didn’t tell anyone till she almost broke her hip. Then we found out the new version had a different filler. Now she only takes the one with the blue cap. Simple stuff, but it matters.
Vanessa Barber
January 29, 2026 AT 10:39Yeah right, the FDA’s got this under control. Tell that to the guy who got liver damage from a generic version and got told it was ‘probably stress.’ They’re understaffed, underfunded, and still relying on people to voluntarily report side effects like it’s 1998. Meanwhile, big pharma is laughing all the way to the bank.
Stacy Thomes
January 30, 2026 AT 11:51THIS IS SO IMPORTANT!! I didn’t realize how much goes into making sure your $5 pill doesn’t kill you. The inspections, the data mining, the unannounced factory visits-it’s like a superhero movie but with lab coats and spreadsheets. We take this for granted. Please, if you notice something weird-REPORT IT. It could save someone’s life.
dana torgersen
January 31, 2026 AT 17:18you know... the real issue isn't even the FDA... it's that we've been conditioned to think 'generic' means 'cheap'... but what if... what if the real danger isn't the drug... but our own assumptions? I mean... think about it... we trust brand names because of marketing... but the science... the science says they're the same... and yet... we still fear the little blue pill with the weird logo... maybe... maybe the problem isn't the manufacturing... it's the mind?
Dawson Taylor
January 31, 2026 AT 22:53Post-market surveillance is not a backup system. It is the primary safety mechanism for generics. The clinical trial model is insufficient for rare, delayed, or population-specific adverse events. The integration of real-world data, manufacturing oversight, and regulatory responsiveness constitutes a robust, adaptive framework. Continued vigilance is non-negotiable.