Splitting or crushing pills might seem like a simple fix-maybe you need half a dose, or a loved one can’t swallow whole tablets. But what looks like a quick solution can turn into a serious health risk if done wrong. Cross-contamination, uneven doses, and exposure to dangerous chemicals aren’t just theoretical dangers-they happen every day in homes and care facilities. In fact, improper pill splitting contributes to over 8% of medication errors in long-term care, according to the Agency for Healthcare Research and Quality. And it’s not just about mistakes. Some pills aren’t meant to be split or crushed at all. If you’re doing this regularly, you need to know how to do it safely-or better yet, when not to do it at all.
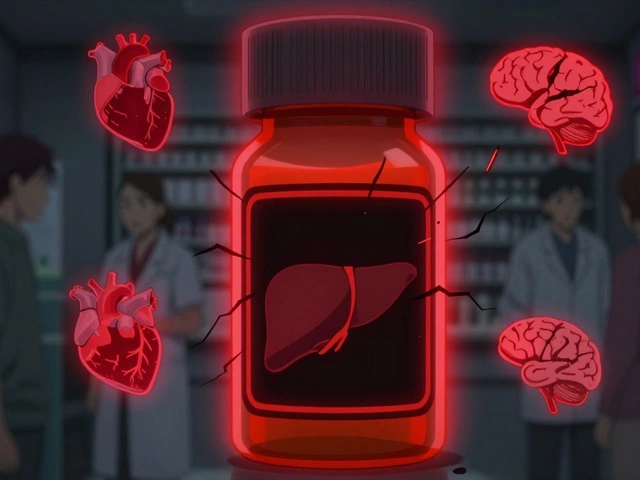
Not All Pills Can Be Split or Crushed
The first rule is simple: check the label. Many medications are designed to release slowly over time, protect the stomach lining, or shield the drug from air and moisture. Crushing or splitting these can destroy that design-and turn a safe medicine into a harmful one.
Enteric-coated pills, like some aspirin or omeprazole, have a special coating that prevents them from dissolving in the stomach. Crush them, and the drug hits your stomach too early, causing irritation or reducing effectiveness. Sustained-release tablets, such as metformin ER or oxycodone OROS, are built to release medication over hours. Splitting them releases the full dose all at once, which can lead to overdose. And then there are hazardous drugs-like chemotherapy agents such as cyclophosphamide or leflunomide. Crushing these can create airborne particles that stick to skin, clothes, or surfaces. Studies have found traces of these drugs on caregivers’ gloves, even after routine handling.
The FDA says 97.8% of enteric-coated, extended-release, or hazardous drugs should never be split or crushed. If the pill doesn’t have a score line (a visible groove down the middle), assume it’s not meant to be split. And if the packaging says “DO NOT CRUSH” or “SWALLOW WHOLE,” don’t ignore it. That warning is there for a reason.
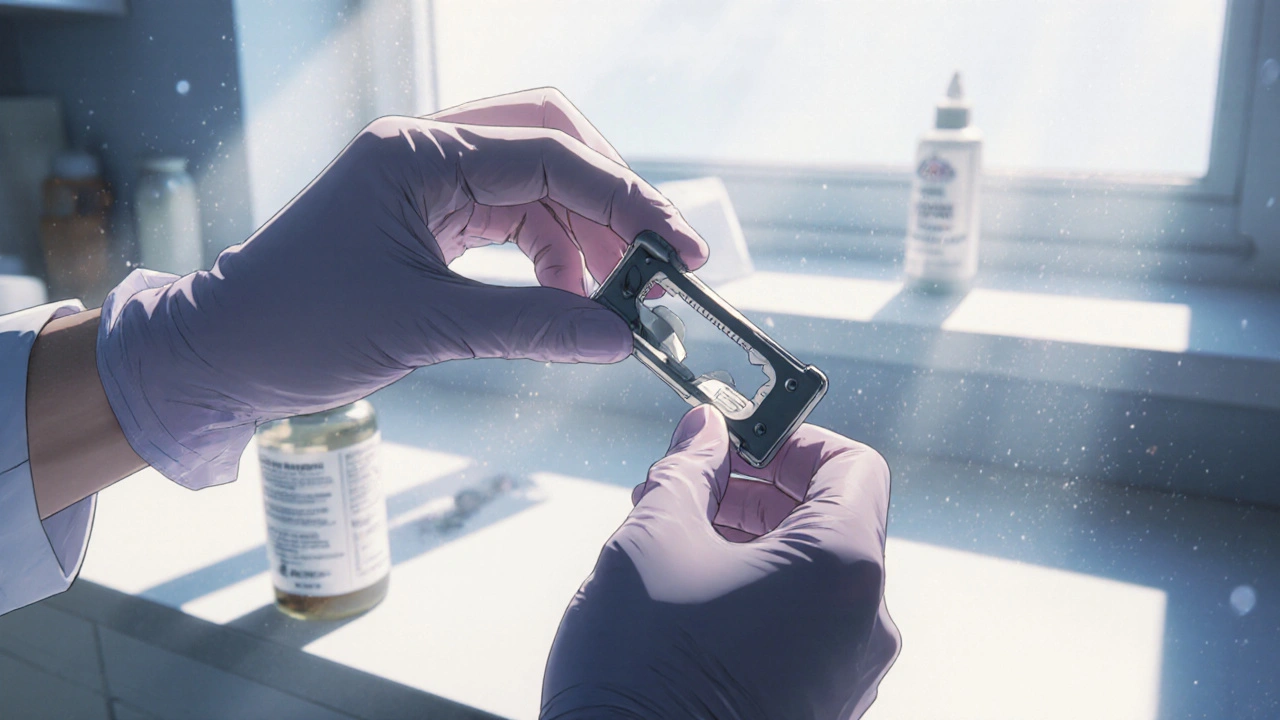
Use the Right Tools-Not Kitchen Scissors
Using a knife, scissors, or your fingers to split a pill is one of the most common-and dangerous-mistakes. A 2021 study from the University of Jordan showed that splitting pills with scissors resulted in dose inaccuracies over 36% of the time. That means one person might get 70% of the dose, another might get 130%. For drugs like warfarin or levothyroxine, where tiny differences matter, that’s life-threatening.
The only tool you should use is a dedicated pill splitter. These aren’t just plastic gadgets-they’re precision devices. Look for one with a stainless steel blade, a v-shaped holder to keep the pill centered, and a retractable blade that lowers cleanly. Models like the Silent Knight or Med-Plus Pro are designed to split pills with a tolerance of just 0.05mm. That’s the difference between getting 5mg and 5.5mg of a critical medication.
And never use the same splitter for different medications without cleaning it. Dust and residue from one pill can mix with another. A 2022 study from a UK care home found that 65% of staff reused splitters between patients without cleaning them. That’s how warfarin contamination happened in Oakwood Care Center, affecting 14 residents. Clean your splitter after every use with a 70% isopropyl alcohol wipe. Let it dry completely before the next use.
Closing the System for Hazardous Drugs
If you’re handling chemotherapy drugs, antivirals, or other hazardous medications, you’re not just dealing with pills-you’re handling potential toxins. The National Institute for Occupational Safety and Health (NIOSH) lists over 100 drugs that require special handling. Crushing these in an open container can release fine powder into the air. Inhaling or touching that dust can cause skin rashes, reproductive harm, or even cancer over time.
The gold standard for crushing hazardous drugs is a closed-system device like the Silent Knight crusher. It seals the pill inside a chamber and crushes it with a rotating blade, trapping over 99.8% of particles. Open crushing-like using a mortar and pestle or a pill crusher with a lid that doesn’t seal-lets up to 28% of the drug escape. That’s why OSHA’s updated Hazardous Drugs Standard (effective January 1, 2025) now requires closed-system crushing for all NIOSH-listed drugs in healthcare settings.
Even at home, if you’re crushing a hazardous drug for a family member, use a sealed system. Wear disposable gloves. Wash your hands thoroughly afterward. Never clean crushed medication residue with your bare hands. And never vacuum or sweep the area-use a damp cloth to wipe down surfaces. If you’re unsure whether a drug is hazardous, ask your pharmacist. They have access to NIOSH’s full list.

Don’t Pre-Split or Store Split Pills
It’s tempting to split a whole month’s supply at once and store the halves. But pills don’t stay stable after being split. Exposure to air, light, and moisture can break down the active ingredient. A 2023 study found that split tablets lost up to 15% of their potency within 7 days when stored at room temperature.
The FDA explicitly says: “Do not split the entire supply at one time and then store them.” Split pills only when you’re ready to take them. If you’re using a pill splitter, do it one pill at a time. If you’re using a crusher, crush just enough for one dose. Store whole pills in their original container, in a cool, dry place. If you must store split pills, use airtight containers and label them with the date and time. Use them within 24 hours, and never use split pills that look discolored, cracked, or dusty.
Hand Hygiene and Personal Protection
Even if you’re using the right tools, contamination can still happen through your hands. A 2024 survey found that while 78% of caregivers washed their hands before handling medication, only 35% used gloves. That’s not enough.
Always wash your hands with soap and water before and after handling pills. If you’re splitting or crushing, wear disposable nitrile gloves. Change them between different medications. Never touch the inside of a pill splitter or crusher with bare hands. After cleaning, rinse your gloves with water and discard them. Don’t reuse them.
And if you’re working in a care home or hospital setting, follow the CDC’s aseptic technique: disinfect the surface you’re working on with alcohol wipes, use single-use equipment for each patient, and never leave tools unattended. These aren’t just best practices-they’re mandatory under Joint Commission standards.

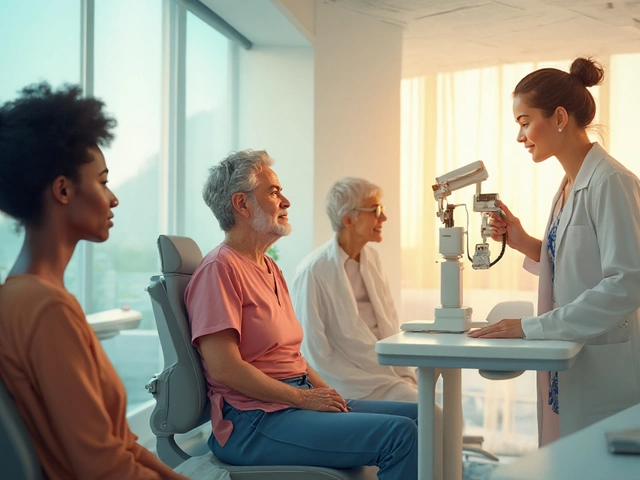
When to Call the Pharmacist
If you’re unsure whether a pill can be split, if you’re having trouble getting the right dose, or if the pill keeps breaking unevenly-call your pharmacist. They’re not just there to fill prescriptions. They’re trained to help you use medications safely.
Many pharmacies now offer free pill-splitting services. They use professional-grade equipment and store split doses properly. Some even provide pre-split doses in labeled blister packs. If cost is a concern, ask if they can switch you to a lower-strength tablet instead of splitting a higher one. For example, instead of splitting a 20mg tablet, you might be able to take a 10mg tablet. That’s safer, more accurate, and often cheaper.
Also, if your medication list has changed recently, ask if any new drugs can’t be crushed or split. Pharmacists can update your medication record with “DO NOT CRUSH” alerts that should appear in your EHR. If you’re a caregiver, make sure the care home or nurse has this information too.
What to Do If You’ve Already Split or Crushed Wrong
If you’ve already split a pill that shouldn’t have been split, or crushed a hazardous drug without protection, don’t panic-but don’t ignore it either.
Stop using that pill. Don’t take it. Don’t flush it. Don’t throw it in the trash. Bring it to your pharmacy. They can safely dispose of it as hazardous waste if needed.
If you think you’ve been exposed to a hazardous drug dust-say, you crushed a chemotherapy pill without a closed system and now have a rash, cough, or eye irritation-see a doctor immediately. Tell them exactly what you did. They can monitor for signs of toxicity.
And if you’re a caregiver, report the incident to your supervisor. Most care homes have medication error reporting systems. These aren’t for blame-they’re for fixing systems so it doesn’t happen again.
Final Checklist: Safe Pill Splitting and Crushing
- ✔ Only split pills with a visible score line and no “DO NOT CRUSH” warning
- ✔ Use a dedicated pill splitter with a stainless steel blade-never scissors or knives
- ✔ Clean the splitter with 70% isopropyl alcohol after every use
- ✔ Never split or crush hazardous drugs without a closed-system crusher
- ✔ Wear gloves when handling any split or crushed medication
- ✔ Split one pill at a time-never pre-split a whole month’s supply
- ✔ Store whole pills only; if you must store split pills, use them within 24 hours
- ✔ Wash hands before and after handling medication
- ✔ Ask your pharmacist if a lower-strength tablet is available instead
- ✔ Report any errors or exposures immediately
Medication safety isn’t about being perfect. It’s about being careful. One wrong split can have real consequences. But with the right tools, knowledge, and habits, you can avoid contamination and keep yourself or your loved one safe.
Can I split pills with a knife or scissors if I don’t have a pill splitter?
No. Using a knife or scissors leads to uneven splits, inaccurate doses, and increases the risk of contamination. A 2021 study found that splitting with scissors resulted in dose errors over 36% of the time. Always use a dedicated pill splitter with a stainless steel blade and v-shaped holder for accurate, safe splitting.
What happens if I crush a time-release pill?
Crushing a time-release pill releases the entire dose at once, which can cause dangerous side effects or overdose. For example, crushing extended-release oxycodone can lead to respiratory depression or death. These pills are designed to release medication slowly over hours-crushing them removes that safety feature.
Is it safe to crush pills for a feeding tube?
Only if the pill is approved for crushing and you use a closed-system crusher. Many medications, especially enteric-coated or extended-release ones, cannot be crushed for feeding tubes. Always check with your pharmacist or doctor first. Some pharmacies offer liquid alternatives or capsules that can be opened safely.
Can I reuse a pill splitter for different medications?
Only if you clean it thoroughly between uses. Residue from one pill can contaminate another, leading to unintended drug interactions or overdoses. Clean the splitter with a 70% isopropyl alcohol wipe after every use and let it dry completely before using it for another medication.
How do I know if a pill is hazardous?
Check the medication label for warnings like “cytotoxic,” “teratogenic,” or “hazardous.” Common examples include chemotherapy drugs (cyclophosphamide), antivirals (ganciclovir), and some hormonal treatments. Your pharmacist can tell you if a drug is on the NIOSH Hazardous Drug List. If in doubt, assume it’s hazardous and use a closed-system crusher with gloves.
Should I split pills to save money?
It can be cost-effective, but only if done safely. Splitting a 40mg tablet into two 20mg doses can save money-but only if the pill is approved for splitting and you use the right tools. Ask your pharmacist if a lower-strength tablet is available. Sometimes, buying two 10mg tablets is cheaper and safer than splitting a 20mg one.
How long can I store split pills?
The FDA recommends splitting pills only when you’re ready to take them. If you must store them, use airtight containers and keep them in a cool, dry place. Split pills lose potency over time-up to 15% in 7 days. Use them within 24 hours if possible. Never use split pills that look discolored, dusty, or cracked.
Can I crush pills for children or elderly people who can’t swallow them?
Only if the pill is safe to crush and you use a closed-system device. Many medications for children and seniors are designed to be swallowed whole. Crushing without knowing the formulation can be dangerous. Always consult your pharmacist. They may offer liquid versions, chewable tablets, or capsules that can be opened safely.



Mike Rothschild
November 28, 2025 AT 21:47Used to split my mom's blood pressure pills with a knife until I read this. Now I use a Silent Knight. No more guessing if she got half or three-quarters. Small tool, huge difference.
Wash it with alcohol after every use. Simple. Non-negotiable.
Ron Prince
November 29, 2025 AT 00:22lol so now we need stainless steel pill splitters and niosh certified crushers just to take a damn pill? next theyll make us wear hazmat suits to swallow ibuprofen. america has officially lost its mind.
my grandpa crushed his meds with a spoon and lived to 92. guess he was just lucky.
King Splinter
November 30, 2025 AT 07:25Let me get this straight. We're treating pill splitting like it's defusing a bomb. You're telling me if I accidentally split a metformin ER with a knife I'm gonna overdose and die? That's the same logic that says you can't cut a banana with a butter knife. It's not ideal, sure. But people have been doing this for decades without turning into human fireworks.
Also who the hell has a Silent Knight in their kitchen? That thing costs more than my first car. And why am I supposed to clean it with alcohol? I'm not sterilizing a surgical tool I'm splitting a 10mg tablet.
There's a reason they don't put warning labels on every pill. Because most of us aren't pharmacists and we're not trying to become one just to take our meds.
Kristy Sanchez
December 1, 2025 AT 16:48Oh wow. So now my grandma’s heart pill is a classified chemical weapon? I guess I should start wearing gloves before I take my vitamin D too.
It’s funny how we’ve turned the most basic human act-swallowing a pill-into a corporate compliance checklist.
Meanwhile, the real problem is that Big Pharma charges $500 for a 30-day supply of a drug that costs 2 cents to make. But nope. Let’s all panic about dust particles instead.
Also, I crushed my Adderall with a spoon last week. Felt like a rebel. Still alive. Still focused. Still not dead. Just saying.
Michael Friend
December 2, 2025 AT 04:23Someone in Oakwood Care Center got contaminated? Oh my god. That’s it. I’m done. This is the end of civilization as we know it.
Imagine if your mom’s aspirin got mixed with chemo dust. That’s not a mistake. That’s a war crime.
And don’t even get me started on people who reuse splitters. That’s not negligence. That’s evil. Pure evil.
I’m not even going to sleep tonight until I’ve sanitized my entire bathroom. I think I touched a pill once with my bare hands. I’m probably dying.
Jerrod Davis
December 3, 2025 AT 18:43It is imperative to underscore that the utilization of non-specialized implements for the partitioning of pharmaceutical dosage forms constitutes a noncompliant deviation from established clinical safety protocols. The documented incidence of dosage inaccuracy exceeds statistically significant thresholds, thereby rendering such practices ethically and clinically indefensible.
Furthermore, the absence of closed-system containment during the comminution of hazardous agents violates OSHA Regulation 1910.1200 and Joint Commission Standard MM.03.01.01.
It is recommended that all laypersons defer such procedures to licensed pharmacy personnel.
Dominic Fuchs
December 3, 2025 AT 23:03There’s a deeper question here isn’t there? Why do we even need to split pills in the first place? Because the system makes us. Because pills come in 20mg and 40mg and no one makes a 15mg version.
It’s not that we’re careless. It’s that the system is broken.
And now we’re supposed to buy a $70 gadget to fix a problem created by drug companies who won’t make the right sizes.
So we’re the ones who have to become pharmacists. And clean our tools with alcohol. And wear gloves.
Meanwhile, the real cost? The emotional toll. The fear. The guilt when you’re not sure if you did it right.
That’s the real contamination.
Asbury (Ash) Taylor
December 5, 2025 AT 01:47Thank you for this. Seriously.
My aunt is in hospice and they gave her a pill that needed to be crushed for her feeding tube. We didn’t know. We used a mortar and pestle. We didn’t wear gloves. We didn’t know it was hazardous.
This post saved us. We called the pharmacist right away. They told us to stop. They gave us a liquid version. They didn’t judge. They just helped.
So if you’re reading this and you’re scared or unsure-call your pharmacist. They’re not there to make you feel stupid. They’re there to make sure you don’t get hurt.
You’re not alone. And you’re doing better than you think.
Kenneth Lewis
December 5, 2025 AT 17:50bro i just use my teeth to split pills lmao its fine
also i reuse my splitter like 3 times before wiping it with a napkin
and yeah i know the guy who crushed his chemo pill without gloves and he’s fine
also i think the FDA is just trying to sell more splitters
also i just ate a split pill that looked kinda dusty
but hey its all good right?
lol
Jim Daly
December 6, 2025 AT 02:04why do we even have to do this at all? why cant the pills just come in the right size? why do i need a whole system just to take my medicine? why am i cleaning a splitter like its a lab tool? this is stupid.
my dog eats my meds sometimes and hes fine so i think its all fake.
also i think the guy who wrote this works for silent knight.
also i crushed my pills with a hammer once. it was kinda fun.
still alive.
still taking meds.
still not dead.
so yk
Mike Rothschild
December 6, 2025 AT 13:19Asbury, you’re right. This isn’t about perfection. It’s about reducing risk.
My mom’s on warfarin. A 0.5mg difference can mean a clot or a bleed.
I used to split hers with my fingers. Now I use the splitter. I clean it. I label the halves. I don’t pre-split.
It’s not hard. It’s not expensive. It’s just a habit.
And if you’re worried about cost? Ask your pharmacist for a lower-dose tablet. They’ll usually say yes.
One less thing to worry about.
That’s what this is really about.