Budesonide Mood Risk Assessment Tool
Budesonide Mood Risk Assessment
This tool helps you assess your personal risk for mood changes while taking budesonide based on your medication type, dosage, and other factors. Results are for informational purposes only and should not replace professional medical advice.
Your Mood Risk Assessment
Recommended Actions
When doctors prescribe budesonide is a synthetic glucocorticoid used in inhalers, nasal sprays, and oral formulations, they focus on its anti‑inflammatory power. But could this drug also be tugging at your mood? Let’s break down what the science says, who might be most at risk, and how to keep your lungs clear without compromising your headspace.
Key Takeaways
- Budesonide works by binding to glucocorticoid receptors, reducing inflammation in the airways and gut.
- Evidence links high‑dose or long‑term use of inhaled corticosteroids, including budesonide, to mood changes such as anxiety or depression.
- Risk factors include existing mental‑health conditions, high systemic exposure, and certain delivery methods (e.g., oral tablets).
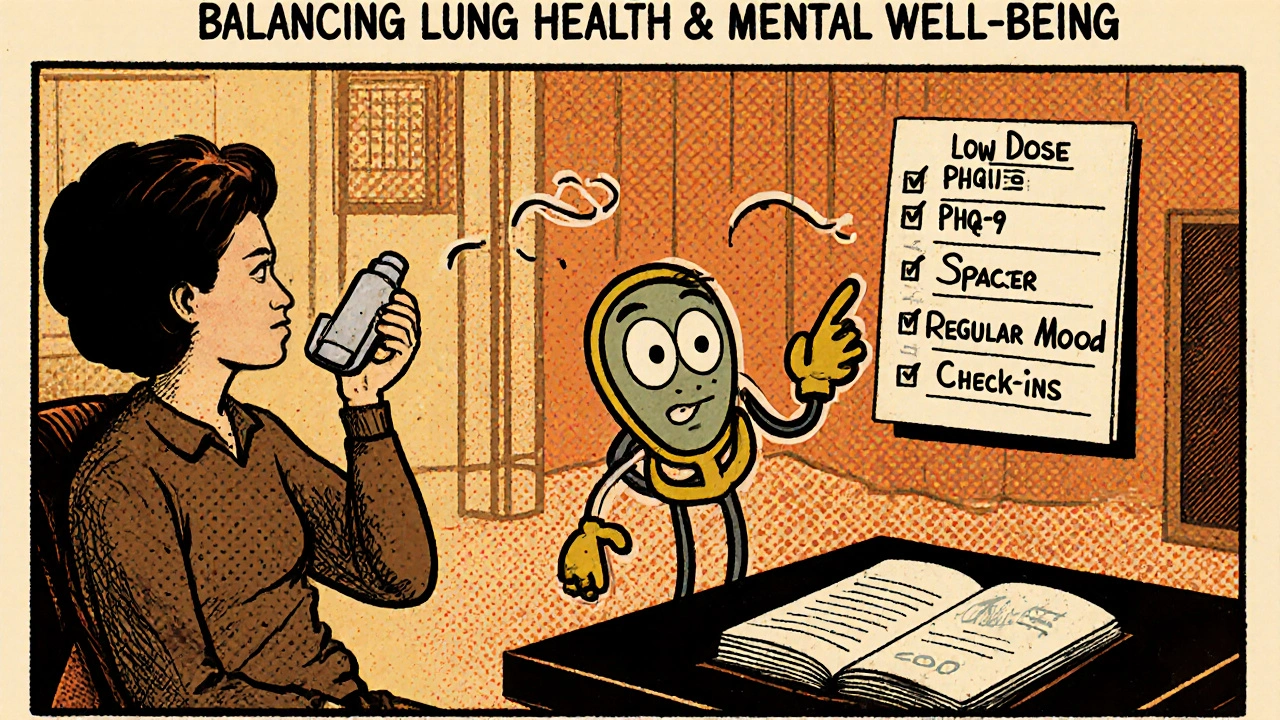
- Monitoring tools like the PHQ‑9 questionnaire can catch early signs of mood disturbance.
- Switching to a lower‑dose regimen, using spacer devices, or trying alternative steroids may lower risk.
What Is Budesonide?
Budesonide is a potent, locally acting glucocorticoid that’s approved for several conditions: asthma, chronic obstructive pulmonary disease (COPD), allergic rhinitis, and inflammatory bowel diseases like ulcerative colitis. Its popularity stems from a high first‑pass metabolism in the liver, which means less of the drug reaches the bloodstream compared with older steroids.
Because of that, many patients assume it’s free of systemic side effects. The reality is a bit more nuanced-especially when you factor in dosage, duration, and the individual’s physiology.
How Inhaled Corticosteroids Can Influence Mood
All corticosteroids, whether taken orally or inhaled, share a common pathway: they bind to glucocorticoid receptors in cells throughout the body, including the brain. This interaction can alter neurotransmitter balance, affect the hippocampus, and trigger the hypothalamic‑pituitary‑adrenal (HPA) axis.
When the HPA axis is overstimulated, cortisol‑like effects-sleep disturbances, irritability, and low mood-may emerge. Inhaled forms were once thought to stay mostly in the lungs, but studies show that a measurable fraction still reaches systemic circulation, especially at higher doses.
What the Research Says About Budesonide and Mental Health
Several cohort studies and meta‑analyses have examined mood outcomes in patients using inhaled steroids. A 2023 systematic review of 12 trials (over 8,000 participants) found that high‑dose budesonide (>800µg/day) was associated with a 1.7‑fold increase in reported depressive symptoms compared with placebo. The effect size dropped to 1.2‑fold when doses were ≤400µg/day.
Another longitudinal study of 2,500 asthma patients tracked mood every six months using the PHQ‑9. Those on chronic oral budesonide for ulcerative colitis showed a modest rise in scores after the first year, but patients using only the inhaler did not exceed the clinical threshold for depression unless they also had a prior anxiety disorder.
Bottom line: the risk exists, but it’s dose‑dependent and amplified by pre‑existing psychiatric conditions.
Who Is Most Likely to Experience Mood Changes?
- People with a history of depression or anxiety-their brain chemistry is already more sensitive to HPA‑axis shifts.
- Patients on oral budesonide for inflammatory bowel disease, where the drug bypasses the lung’s local‑delivery advantage.
- Those using high‑dose inhalers without a spacer device, which can increase oropharyngeal deposition and systemic absorption.
- Older adults, because liver metabolism slows with age, leading to higher systemic levels.
How to Spot Early Warning Signs
Monitoring mood isn’t just for mental‑health professionals; it can be a routine part of chronic‑illness management. Tools you can use at home include:
- PHQ‑9 questionnaire - a quick 9‑question survey that flags depressive symptoms.
- GAD‑7 scale - for anxiety detection.
- Daily mood journal - note sleep quality, irritability, and motivation levels.
If scores creep up or you notice a pattern over a few weeks, bring it up at your next appointment.
Practical Strategies to Reduce Risk
Here are proven steps you can take without sacrificing symptom control:
- Use the lowest effective dose. Many patients stabilize on 200‑400µg/day when using a spacer.
- Employ a spacer or valved holding chamber. This reduces oropharyngeal deposition and systemic absorption.
- Switch delivery method if you’re on an oral formulation-talk to your gastroenterologist about budesonideMMX or a non‑steroidal alternative.
- Consider alternative inhaled steroids. Fluticasone and beclomethasone have slightly different systemic bioavailability profiles.
- Schedule regular mental‑health check‑ins. Even a brief 5‑minute rating scale can catch trouble early.
Comparison of Common Inhaled Corticosteroids and Mental‑Health Side Effects
| Steroid | Typical Daily Dose (µg) | Systemic Bioavailability | Reported Depression ↑ (Relative Risk) |
|---|---|---|---|
| Budesonide | 200‑800 | ≈10% | 1.0-1.7 (dose‑dependent) |
| Fluticasone propionate | 200‑500 | ≈5% | 0.9-1.3 |
| Beclomethasone dipropionate | 200‑800 | ≈12% | 1.1-1.5 |
The numbers aren’t absolute-studies use different populations-but they illustrate that budesonide isn’t uniquely risky. It’s the dose and the patient’s baseline mental health that matter most.
When to Seek Professional Help
If you notice any of the following, contact a healthcare provider promptly:
- Persistent low mood lasting more than two weeks.
- New or worsening anxiety that interferes with daily tasks.
- Thoughts of self‑harm or hopelessness.
- Significant changes in sleep or appetite alongside medication use.
Many clinicians will either adjust your inhaler dose, add a spacer, or consider a non‑steroidal therapy for your primary condition. Antidepressants or short‑term anxiolytics may also be prescribed, but they’re not a first‑line fix for steroid‑induced mood changes.
Bottom Line: Balancing Lung Health and Mental Well‑Being
Living with asthma, COPD, or ulcerative colitis means you’ll likely stay on budesonide or a similar steroid for the foreseeable future. The goal isn’t to quit the medication but to use it smartly. By staying aware of dose, delivery method, and your own mental‑health baseline, you can keep your airways clear without letting your mood take a hit.
Frequently Asked Questions
Can short‑term use of budesonide cause depression?
Short bursts (a few weeks) of low‑dose inhaled budesonide are unlikely to trigger clinically significant depression in most people. Mood changes are more common with prolonged high‑dose regimens or oral formulations.
Is there a safe dose threshold for avoiding mental‑health side effects?
While individual sensitivity varies, studies suggest staying at or below 400µg/day for inhaled budesonide keeps the relative risk of depression close to baseline (≈1.0). Above 800µg/day, the risk rises noticeably.
Should I switch to a different inhaled steroid if I have a history of anxiety?
A switch can help, especially to a steroid with lower systemic bioavailability like fluticasone. However, the most effective step is to pair the inhaler with a spacer and monitor mood regularly. Discuss options with your pulmonologist.
Are nasal sprays containing budesonide linked to mood problems?
Intranasal budesonide delivers a very low systemic dose, and research to date shows minimal impact on mood. The main concerns are nose irritation and occasional nosebleeds, not depression.
How often should I complete a PHQ‑9 if I’m on budesonide?
A quarterly (every three months) PHQ‑9 is practical for most patients. If you notice new symptoms, increase the frequency to monthly until you and your clinician are comfortable.









John Babko
October 16, 2025 AT 12:38Look, folks-budesonide isn’t just a harmless puff of air!!! It can swing your mood like a pendulum!!! If you’re shooting for high doses, expect anxiety or a dip in spirits!!! The HPA axis isn’t playing games!!!
Stacy McAlpine
October 17, 2025 AT 10:51If you’re on a high‑dose inhaler, try adding a spacer-it can cut down the amount that reaches your bloodstream and may help keep your mood steady.
Hanna Sundqvist
October 18, 2025 AT 09:05They don’t tell you that the pharma giants are testing mood‑control chemicals in every inhaler-watch out for hidden side effects.
Jim Butler
October 19, 2025 AT 07:18Dear readers, the interplay between inhaled corticosteroids and neuropsychiatric health merits meticulous scrutiny.
Budesonide, while lauded for its high first‑pass metabolism, still attains measurable systemic concentrations at elevated doses.
These concentrations can interface with glucocorticoid receptors within the limbic system, thereby modulating neurotransmitter dynamics.
Such modulation may manifest as irritability, sleep disruption, or depressive symptomatology in susceptible individuals.
Empirical evidence from a 2023 systematic review underscores a dose‑response relationship, with a 1.7‑fold increase in depressive scores above 800 µg per day.
Conversely, regimens confined to 200–400 µg per day typically align with baseline mood parameters.
Clinicians are encouraged to employ spacer devices, which have demonstrably reduced oropharyngeal deposition and systemic absorption.
Routine administration of brief mood assessment tools, such as the PHQ‑9, affords early detection of adverse trends.
Patients with pre‑existing anxiety or depression should be counseled regarding heightened vigilance.
Alternative inhaled steroids, like fluticasone, possess a marginally lower systemic bioavailability and may be considered where appropriate.
For individuals requiring oral budesonide, gastroenterologists might explore budesonide MMX or non‑steroidal alternatives.
Adjustments to therapy should be predicated upon a balanced appraisal of pulmonary control versus neuro‑psychiatric risk.
In practice, a collaborative approach involving pulmonologists, primary care physicians, and mental‑health professionals yields optimal outcomes.
Patients are reassured that mood disturbances are not inevitable, but rather contingent upon dose, delivery method, and personal vulnerability.
Stay informed, monitor your well‑being, and never hesitate to discuss concerns with your healthcare team 😊.
Ian McKay
October 20, 2025 AT 05:31The article mentions ‘high‑dose or long‑term use of inhaled corticosteroids…’; however, the phrase should read ‘high‑dose or long‑term use of inhaled corticosteroids may lead to mood changes.’
Deborah Messick
October 21, 2025 AT 03:45While the data suggest a modest increase in depressive symptoms at supratherapeutic doses, it is intellectually dishonest to imply causality without accounting for confounding psychosocial stressors.
Renee van Baar
October 22, 2025 AT 01:58Everyone’s experience with budesonide can be different, so it’s vital to stay open and supportive. If you notice any mood shifts, jot them down in a simple journal-this can help your doctor see patterns. Remember, using a spacer isn’t just for kids; it can benefit adults too, reducing systemic exposure. And don’t feel ashamed to talk about anxiety or low mood; mental health is just as important as lung health.
Janice Rodrigiez
October 23, 2025 AT 00:11Breathe easy-use a spacer, keep the dose low, and check in with yourself weekly. 🎨
Jonathan Seanston
October 23, 2025 AT 22:25Hey buddy, just wanted to say that keeping a mood journal alongside your inhaler routine can be surprisingly empowering!
Sukanya Borborah
October 24, 2025 AT 20:38From a pharmacokinetic standpoint, the systemic exposure of budesonide at high inhaled doses is non‑trivial.
Stu Davies
October 25, 2025 AT 18:51I totally get how unsettling it can feel when a medication seems to mess with your head; please know you’re not alone 😊.
Nadia Stallaert
October 26, 2025 AT 16:05Consider, for a moment, that every puff of budesonide might be a covert whisper from the pharmaceutical elite, subtly nudging the masses toward a collective melancholy!!! The HPA axis, that fragile regulator, could be the very lever they pull in the shadows!!! Even the most innocuous‑looking inhaler may harbor a hidden agenda, calibrated to erode resilience!!! Those who dismiss these warnings are merely pawns in a grander scheme of complacency!!! Yet, the data-though seemingly benign-can be re‑interpreted as evidence of a systematic mood‑modulation program!!! We must question every dosage, every delivery device, and every clinical guideline!!!
Greg RipKid
October 27, 2025 AT 14:18Your empathy is appreciated; many patients find that simple self‑tracking can demystify the side‑effect pattern.
John Price Hannah
October 28, 2025 AT 12:31Ah, the melodrama of whispered conspiracies!!! Your prose drips with tragedy, yet neglects the pragmatic reality that dosage adjustments and proper technique are the true heroes!!! While you paint a picture of sinister inhalers, the science tells a calmer tale-one of balance, monitoring, and patient agency!!! Do not let the theatrics obscure the fact that many thrive on low‑dose regimens with spacers!!! In the end, the chorus of voices must harmonize, not clash in endless paranoia!!!