No one wants a bacterial infection hanging around longer than it has to. But getting rid of it isn’t just about taking antibiotics—you also need to play by some rules if you want that little white pill to work its magic. Ever wondered why your doctor insists you take ampicillin at certain times, away from meals, or what you should do if you blank on a dose? This isn’t just busywork; it actually changes whether you feel better fast or end up grumbling about your health for weeks.
Why Precise Timing Matters with Ampicillin
Imagine this: you take your dose a little late or with a burger and fries, not thinking much about it. What’s the big deal, right? Turns out, timing really does matter for ampicillin. It belongs to a group of antibiotics called penicillins, which break down stubborn bacteria that make us sick. Here’s the catch—the amount of ampicillin in your blood goes up and down depending on when and how you take it.
Ampicillin works best when it keeps a steady beat in your bloodstream. That’s why doctors often ask you to spread your doses evenly over the day, usually every 6 hours for adults (yeah, that includes waking up in the middle of the night sometimes). If you take it after a large meal, as tempting as it might be when your stomach’s rumbling, much less of the antibiotic makes it into your system. That’s because food can actually trap the medicine, stopping your body from grabbing onto it.
The golden rule with ampicillin—take it on an empty stomach. That means an hour before you eat, or two hours after. This is not your doctor being a stickler. There’s proof: one study found the concentration of ampicillin in the blood was up to 50% less when taken with food. That’s like giving bacteria a chance to regroup. So, set those reminders, use your phone alarms, or even a simple sticky note by your breakfast bowl—every hour counts for that infection-fighting power.
Kids and older adults, by the way, might need a slightly different rhythm in dosing to match their body’s speed at processing the medicine. This is exactly why you should never count on someone else’s prescription or dosing plan, even if they’re about your size and age.
Ampicillin and Food: What You Should (and Shouldn’t) Eat
If you’re thinking, “I’ll just wash down my ampicillin with a quick snack,” hold up! Ampicillin is a little picky. Fatty foods, dairy, and even something as harmless as orange juice can block it from being absorbed properly. Why? The molecules in certain foods, especially dairy, latch onto the antibiotic and drag it into your gut, where it can’t actually fight your infection anymore. The result? Lower levels of medicine in your system and possibly a longer recovery time.
You don’t have to starve, but keep things simple—just water with your pill. If you sometimes wake up starving, it can help to plan your doses around natural appetite lulls. Many people take their medicine first thing in the morning and just before bed when they’re less likely to want a full meal right away. This makes timing much easier to stick to day after day.
Don’t worry about missing out on nutrients for a few hours—this isn’t forever. Most ampicillin courses last from 7 to 14 days. Keep a glass of water nearby as a reminder. Drink plenty of fluids during your course to help your kidneys flush out both the infection and the medicine.
Caffeine, by the way, isn’t directly harmful with ampicillin but strong coffee on an empty stomach can irritate some people’s stomach linings when mixed with antibiotics—so watch for tummy troubles if you’re sensitive.

Missed Dose Protocols: What to Do If You Forget
Life gets chaotic and missing a dose can sneak up on anyone. What happens if you realize you forgot a pill? First: don’t panic, and don’t double up to "make up for it." Taking two doses at once can spike side effects and doesn’t actually supercharge your recovery.
The best move is simple: if it’s only been a couple of hours since you were supposed to take it, go ahead and take the missed dose as soon as you remember. But if it’s almost time for your next scheduled pill, just skip the missed one and get back on track. Consistency is more helpful than playing catch-up when it comes to antibiotics.
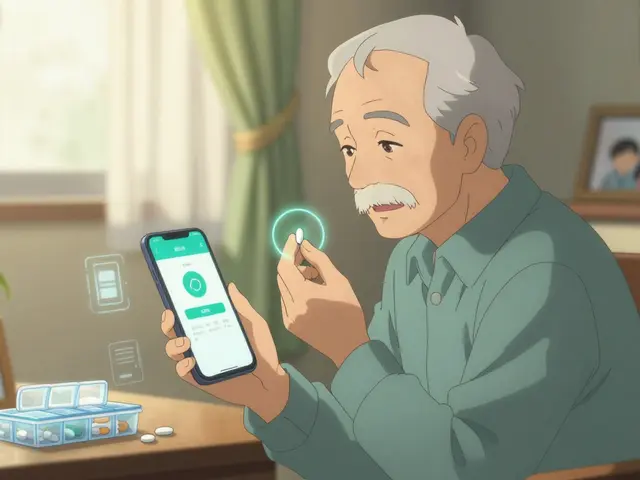
It can help to use a medicine tracker app or chart. Lots of people find that keeping a small log—just writing down each dose in your notes app or on the fridge—makes all the difference.
- Never double dose: Taking two pills won’t erase the missed dose and can increase side effects like diarrhea, nausea, or skin rashes.
- If you keep missing doses or find the timing hard, check with your doctor. They can sometimes adjust the schedule or suggest ways to make it easier.
- Stick out the full course: Stopping early (even if you feel better) is one of the top reasons bacterial infections come back stronger. Bacteria are smart—give them an inch, they’ll take a mile.
If you have trouble remembering because of a busy schedule or a lot of pills to manage, talk to your pharmacist. They’ve got clever tricks—like weekly pill organizers or timer caps—that can save you a lot of hassle.
Troubleshooting Side Effects and Getting the Best Results
Even when you do everything right, sometimes side effects show up. Nausea, mild diarrhea, or a little rash are the most common, and they often go away when your course is finished. But if you get hives, trouble breathing, or your face and lips start to swell, it could be an allergy—don’t wait around, get medical help fast.
Here’s a quick stats table so you know what’s typical and what’s not:
| Side Effect | How Common? | What to Do |
|---|---|---|
| Mild stomach upset | ~15% | Usually self-limited, take with a glass of water |
| Diarrhea | ~10% | Stay hydrated, call doctor if severe or bloody |
| Rash (non-allergic) | ~8% | Monitor; if mild, continue medication |
| Allergic reaction (hives/swelling) | ~1-2% | Immediate medical attention needed |
Good bacteria in your gut might take a hit during your antibiotic course. Including simple, probiotic foods like yogurt (just not within two hours of your pill), kefir, or specific probiotic capsules (ask your pharmacist first) can help balance things out. This isn’t a surefire way to dodge stomach problems, but it’s a trick that’s often suggested for people prone to digestive issues.
And here’s a pro-tip for anyone worried about ampicillin and birth control: ampicillin’s effect on most hormonal contraceptives isn’t as big a risk as older advice suggested, but certain antibiotics can make birth control less reliable. If avoiding pregnancy is crucial, a backup (condoms, for example) can put your mind at ease during your course and for a week after.
If you need more info about proper Ampicillin dosage and side effects, that’s a great resource to double-check what you might expect or anything odd you notice.
- Finish all your medicine—even if you feel 100%.
- Store your pills according to the label. Some liquid forms need a fridge; others don’t.
- Don’t share leftover pills. What works for you might not be right for someone else, and letting ampicillin loose on the wrong bacteria can actually help them learn to outsmart the drug next time.
- Keep your doctor in the loop if you have any bad reactions, or if you’re not feeling better halfway through your course.
This is about more than getting rid of a cough or fever for now. Ampicillin is still one of the workhorses of modern medicine, but antibiotic resistance is a real thing. Every time we use antibiotics properly, we help make sure they’ll work for all of us in the future. So, next time you reach for your prescription, give a nod to the science—and stick to the plan.







Ada Xie
July 23, 2025 AT 21:06The guidance provided adheres to established pharmacokinetic principles, delineating the necessity of maintaining plasma concentrations within the therapeutic window. It correctly advises administration on an empty stomach to avert the known diminution of bioavailability associated with concurrent alimentary intake. Moreover, the recommendation to space doses evenly aligns with the half‑life of ampicillin, thereby mitigating the risk of sub‑therapeutic troughs. In sum, the article exemplifies precise, evidence‑based instruction.
Stephanie Cheney
August 5, 2025 AT 15:20Great summary! Staying consistent with those timing cues can feel challenging, but setting a simple alarm or keeping the pill bottle beside your coffee maker often does the trick. Remember, each dose you get right brings you one step closer to a full recovery, so celebrate those small wins.
Georgia Kille
August 18, 2025 AT 08:53👍 Keep it simple: water + pill, alarm + note. 😊
Jeremy Schopper
August 31, 2025 AT 02:26Adhering to the prescribed schedule for ampicillin is not merely a matter of convenience, it is a critical component of antimicrobial stewardship. The pharmacodynamic targets for beta‑lactam antibiotics demand that serum concentrations exceed the minimum inhibitory concentration for a sufficient portion of the dosing interval. Missing or delaying doses compromises this exposure. Consequently, bacterial eradication may be incomplete. This can lead to the selection of resistant subpopulations. Those resistant organisms undermine future therapeutic options. Clinicians therefore emphasize evenly spaced dosing, typically every six hours for most adults. Pediatric and geriatric patients may require adjustments based on renal function and volume of distribution. The article rightly points out that food, especially high‑fat meals and calcium‑rich products, can bind the drug and reduce absorption. Taking the medication with a full glass of water on an empty stomach is advisable. If a dose is missed, the recommended approach is to take it as soon as remembered provided there is still ample time before the next scheduled dose. Otherwise, the dose should be skipped to avoid double‑dosing. Employing tools such as medication reminders, pill organizers, or smartphone applications can greatly reduce the likelihood of missed doses. Moreover, patients should be counseled on the importance of completing the full course, even if symptoms resolve early. Premature discontinuation is a well‑documented driver of relapse and resistance. Finally, any adverse reactions such as severe rash, hives, or respiratory distress warrant immediate medical attention.
liza kemala dewi
September 12, 2025 AT 20:00While the empirical data underscore the mechanistic necessity of maintaining plasma drug concentrations above the pathogen's minimal inhibitory threshold, it is equally worthwhile to contemplate the broader epistemological implications of patient adherence; the act of following a dosing schedule becomes, in a subtle sense, an embodiment of the social contract between individual health agency and collective microbial ecology, wherein each compliant dose contributes to the attenuation of evolutionary pressures that drive resistance; consequently, the seemingly mundane ritual of timing a pill may be reframed as a participatory gesture within a larger biopolitical framework, reminding us that personal health decisions reverberate through communal well‑being; such a perspective invites a more nuanced appreciation of the ethical dimensions inherent in pharmacotherapy, encouraging both clinicians and patients to engage in reflective dialogue about the responsibilities entwined with antibiotic stewardship.
Jay Jonas
September 25, 2025 AT 13:33Man, I totally get it-missin a dose feels like you’re messin up the whole battle against those nasty bugs, but don’t freak out; just grab the pill when you remember and keep movin forward. The whole thing is kinda like a drama, you know? One missed line ain’t the end of the show.
Liam Warren
October 8, 2025 AT 07:06In clinical parlance, what you're describing aligns with the concept of pharmacokinetic adherence-a key determinant of AUC/MIC ratios that drive bactericidal activity. Leveraging digital adherence technologies, such as smart pill bottles or EMR‑integrated alerts, can operationalize real‑time compliance metrics, thereby optimizing therapeutic outcomes.
Brian Koehler
October 21, 2025 AT 00:40Bravo for tackling the nitty‑gritty of ampicillin timing! Your checklist reads like a master‑class in antibiotic choreography, and the vivid analogies make the science dance in the reader’s mind. Keep sprinkling that creative flair-it turns a routine medical memo into a compelling narrative.