Pediatric Sedation: Safe Practices, Common Drugs, and What Parents Need to Know
When a child needs a procedure like an MRI, dental work, or a fracture repair, pediatric sedation, the use of medication to calm a child during medical procedures without putting them fully to sleep. Also known as conscious sedation, it’s a routine but carefully controlled part of pediatric care. Unlike general anesthesia, which stops breathing and requires a ventilator, pediatric sedation keeps the child responsive but relaxed—enough to stay still, but not so deep that it’s dangerous. This balance is why it’s one of the most common, yet most misunderstood, interventions in children’s medicine.
Doctors use specific drugs like midazolam, a fast-acting benzodiazepine used to reduce anxiety and cause mild memory loss, or ketamine, a dissociative anesthetic that provides pain relief and sedation without suppressing breathing. These aren’t chosen randomly. The decision depends on the child’s age, weight, medical history, and the procedure’s length. For example, a 3-year-old getting a head CT might get oral midazolam, while a 7-year-old needing a long dental procedure might get IV ketamine. The goal isn’t to knock them out—it’s to make them comfortable enough to cooperate without risking their airway or heart rate.
Parents often worry about side effects. The most common? Nausea, drowsiness, or odd behavior after waking up. Rare but serious risks include breathing problems or allergic reactions—which is why sedation is never done alone. A trained provider monitors oxygen levels, heart rate, and breathing the whole time. The American Academy of Pediatrics and the American Society of Anesthesiologists both require that someone with advanced life support training be present during every pediatric sedation. If your child has asthma, a history of sleep apnea, or a recent cold, tell the team. Those details change the drug choice and safety plan.
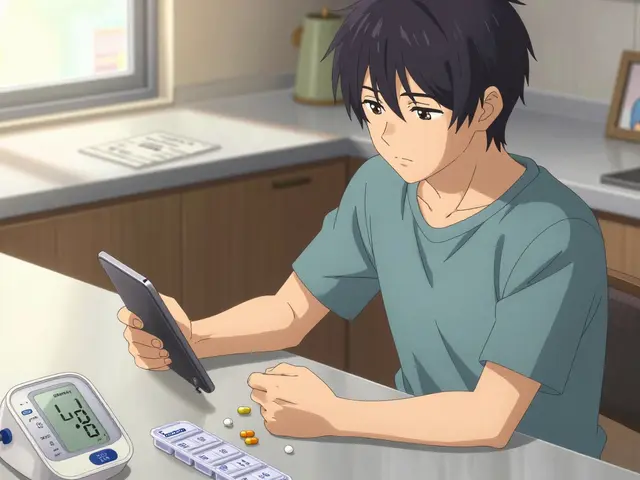
There’s also a growing focus on non-pharmacological methods, techniques like distraction, parental presence, and child life specialists that reduce the need for drugs. Many hospitals now combine these with low-dose sedation to cut side effects. For example, letting a child hold a tablet with a favorite game during an IV start can cut anxiety—and the amount of sedative needed—by half.
What you won’t find in most hospital brochures? The truth about how often sedation is misused. Some clinics push it for minor procedures that don’t need it. Others skip proper fasting rules because they’re busy. That’s why knowing what to ask matters. Before your child is sedated, ask: What drug will be used? How will they be monitored? What happens if they vomit? Who’s in charge if something goes wrong? These aren’t overcautious questions—they’re essential.
Below, you’ll find real-world insights from parents and providers on how pediatric sedation works in practice. From what to expect after the procedure, to how to handle nausea, to when to push back on a doctor’s recommendation—you’ll find clear, no-fluff answers based on actual cases and clinical guidelines.
Learn how to safely prepare your child for surgery with proper fasting rules, pre-op medications like midazolam, and what to do if your child has asthma, epilepsy, or autism. Evidence-based tips from leading children’s hospitals.
Recent-posts
Categories
Tags
- online pharmacy
- side effects
- drug interactions
- generic drugs
- online pharmacy UK
- drug safety
- opioid side effects
- pill organizer
- Tadalafil
- arthritis medication
- buy medication online
- prescription medication
- quit smoking
- motion sickness
- Sildenafil
- Vardenafil
- ED medication alternatives
- biologics
- medication safety
- generic medication prices