Opioid Tolerance: What It Is, Why It Happens, and What You Can Do
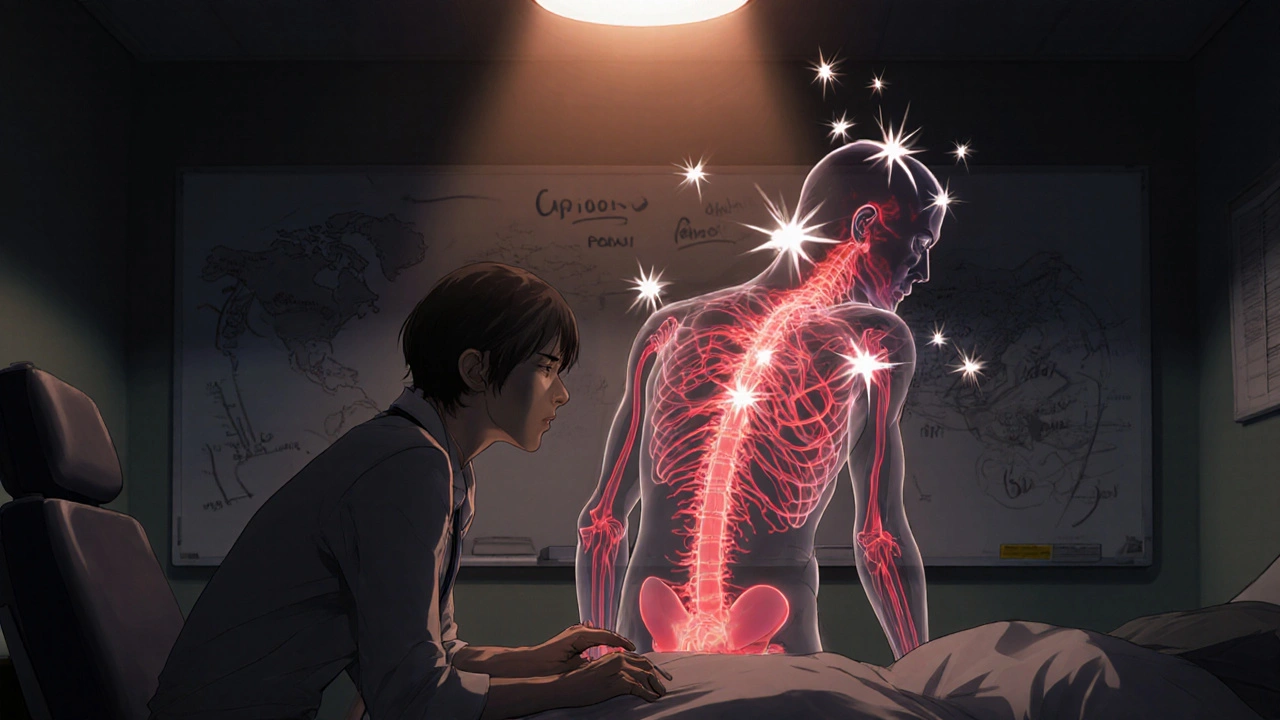
When your body gets used to opioids, you need higher doses to get the same relief—that’s opioid tolerance, a physiological adaptation where the brain and nervous system reduce responsiveness to opioid drugs over time. Also known as drug tolerance, it’s not the same as addiction, but it often goes hand-in-hand with it. This isn’t rare—it happens to people taking opioids for chronic pain, after surgery, or even for short-term injury recovery. If you’ve been on these meds for more than a few weeks, your body has likely started adjusting.
How does this happen? Opioids bind to receptors in your brain that control pain and pleasure. Over time, those receptors become less sensitive, so the same dose doesn’t work as well. Your body also starts producing fewer natural painkillers, like endorphins, because it’s relying on the drug. That’s why stopping suddenly can cause opioid withdrawal, a set of physical and emotional symptoms that occur when someone who has developed tolerance stops taking opioids. Symptoms include nausea, sweating, anxiety, muscle aches, and insomnia. It’s not usually life-threatening, but it’s intensely uncomfortable—and that’s why people keep taking the drug, even when they don’t need it for pain.
What about opioid dependence, a state where the body requires the drug to function normally, leading to withdrawal if stopped? Dependence is a normal result of long-term use, even when taken exactly as prescribed. It doesn’t mean you’re addicted—addiction involves compulsive use despite harm, cravings, and loss of control. But dependence makes quitting harder, and that’s where many people get stuck. The good news? Tolerance and dependence can be managed. Doctors can slowly lower your dose, switch you to a different medication, or add non-opioid pain treatments like physical therapy or nerve blocks. Some people benefit from medications like buprenorphine or methadone, which help stabilize the brain without the highs and lows of full opioids.
And here’s the thing: tolerance doesn’t mean your pain is getting worse. It just means your body has changed. Many people think they need more pills because their condition is deteriorating—but it’s often just their system adapting. That’s why it’s so important to talk to your doctor before making any changes. Don’t just increase your dose on your own. Don’t mix opioids with alcohol or sleep meds. And if you’ve been on them longer than a few months, ask about a taper plan.
Below, you’ll find real-world guides from people who’ve dealt with these issues—whether they’re managing chronic pain, reducing opioid use, or switching to safer alternatives. These aren’t theoretical articles. They’re practical, tested strategies from patients and clinicians who’ve been there. You’ll learn what works, what doesn’t, and how to avoid common traps.
Learn how to tell opioid-induced hyperalgesia apart from tolerance-key signs include spreading pain, allodynia, and worsening symptoms with higher doses. Don't miss this critical distinction in pain management.
Recent-posts
Categories
Tags
- online pharmacy
- side effects
- drug interactions
- generic drugs
- online pharmacy UK
- drug safety
- opioid side effects
- pill organizer
- Tadalafil
- arthritis medication
- buy medication online
- prescription medication
- quit smoking
- motion sickness
- Sildenafil
- Vardenafil
- ED medication alternatives
- biologics
- medication safety
- generic medication prices