If you’re a man over 60 with an enlarged prostate and your doctor just prescribed an anticholinergic for an overactive bladder, stop and think. This isn’t just another medication tweak-it could land you in the ER with a painfully full bladder you can’t empty. That’s not rare. It’s predictable. And it’s happening to thousands of men every year.
What Anticholinergics Do to Your Bladder
Anticholinergics like oxybutynin, tolterodine, solifenacin, and darifenacin work by quieting the bladder muscle. They block acetylcholine, the chemical that tells your bladder to contract. For someone with an overactive bladder-where the bladder squeezes too often, too hard, or without warning-this can reduce urgency and leakage. That sounds good. But here’s the catch: these drugs don’t know the difference between a healthy bladder and one already struggling. In men with benign prostatic hyperplasia (BPH), the prostate presses on the urethra. The bladder has to work harder just to push urine out. Over time, the bladder muscle thickens and becomes overworked. Now, add an anticholinergic on top. It doesn’t just reduce unwanted contractions-it weakens the very contractions you need to empty your bladder. It’s like turning down the engine in a car that’s already climbing a steep hill. The result? Urinary retention.Why Prostate Enlargement Makes This Worse
BPH isn’t just about a swollen gland. It’s about a system under stress. The bladder is already at its limit. Studies show that men with BPH have a 2.3 times higher risk of acute urinary retention when taking anticholinergics compared to those not taking them. That’s not a small increase. That’s a red flag. The American Urological Association (AUA) guidelines from 2018 are clear: don’t use anticholinergics in men with moderate to severe lower urinary tract symptoms or a prostate larger than 30 grams. Why? Because the data doesn’t lie. A 2008 review in PubMed found that up to 10% of all urinary retention cases are caused by medications-and anticholinergics are the top offenders. Real-world evidence backs this up. The FDA’s adverse event database recorded 1,247 cases of urinary retention linked to anticholinergics between 2018 and 2022. Over 60% of those cases were in men over 65 with diagnosed BPH. One Reddit user, sharing his experience under the username u/BPHWarrior, wrote: “After Detrol, I ended up in the ER with a 1,200 ml bladder. I now have a catheter and might need surgery.” That’s not an outlier. It’s a pattern.The Numbers Don’t Add Up
Let’s talk benefit versus risk. The Cochrane Collaboration analyzed 51 trials with over 6,700 patients. They found anticholinergics reduced incontinence episodes by about one per 48 hours compared to placebo. That’s a modest gain. For every seven men treated, only one saw a noticeable improvement. Meanwhile, side effects are common: dry mouth (30-60%), constipation (15-30%), blurred vision (5-10%), and trouble urinating (8-15%). In older men, memory fog and confusion are increasingly recognized. The FDA warned about this in 2012 and updated the warning in 2019. And yet, many doctors still prescribe these drugs without checking prostate size or bladder function first. The American Geriatrics Society’s Beers Criteria-used by hospitals and nursing homes across the U.S. and UK-lists anticholinergics as potentially inappropriate for older adults with BPH or urinary retention. Shockingly, 40% of nursing home residents with these conditions are still getting them. Why? Because the problem isn’t always the drug. It’s the lack of screening.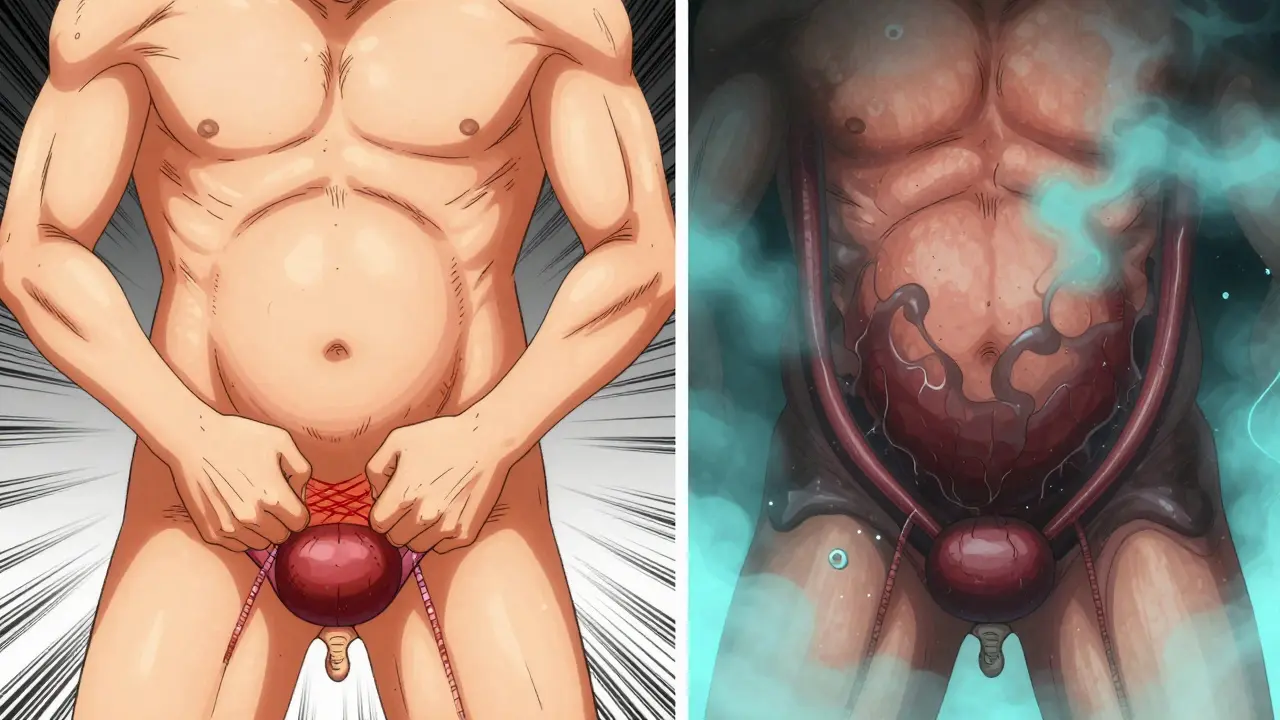
What Should You Do Instead?
There are safer, more effective options for men with BPH and overactive bladder symptoms. Alpha-blockers like tamsulosin (Flomax) and alfuzosin (Uroxatral) relax the muscles around the prostate and bladder neck. They don’t weaken the bladder. In fact, studies show that men with BPH who get an alpha-blocker right after catheter insertion are 30-50% more likely to urinate successfully within a few days than those who don’t. 5-alpha reductase inhibitors like finasteride (Proscar) and dutasteride (Avodart) shrink the prostate over time. It takes months to work, but long-term use cuts the risk of acute urinary retention by half. These aren’t quick fixes, but they’re the right fix for the root problem. And then there’s mirabegron (Myrbetriq) and vibegron (Gemtesa). These are beta-3 agonists. Instead of blocking bladder contractions, they gently stimulate the bladder to relax and hold more urine. No anticholinergic effect. No risk of retention. A 2022 study in European Urology found only a 4% retention rate with mirabegron in men with mild BPH-compared to 18% with anticholinergics. Vibegron got FDA approval in 2020 specifically for patients who can’t tolerate anticholinergics.When Is It Still Okay to Use Them?
Some experts argue there’s a narrow window. Dr. Kenneth Kobashi from Virginia Mason Franciscan Health says that in men with mild BPH, low-dose solifenacin can be used under close monitoring. A 2017 study showed a 12% retention rate in this group-much lower than the 28% seen in unselected patients. But “close monitoring” means more than a quick check-in. It means:- A digital rectal exam to measure prostate size
- Uroflowmetry to check peak urine flow (under 10 mL/s = high risk)
- Post-void residual measurement before starting the drug
- Monthly follow-ups to check for rising residual urine
- Immediate stop if urine flow drops or retention symptoms appear

What Happens If You Develop Retention?
Acute urinary retention is a medical emergency. Your bladder fills beyond capacity-sometimes over 1,500 mL. You feel pressure, pain, bloating, and can’t pee. Left untreated, it can damage your kidneys. The standard fix? Immediate catheterization. A thin tube is inserted through the urethra to drain the bladder. Studies show 85-90% of cases are resolved this way. No need to drain slowly. Empty it all at once. The risk of complications from rapid emptying is low. But catheterization isn’t the end. Without treatment, 70% of men will have another episode within a week. That’s why guidelines say: start an alpha-blocker like tamsulosin the moment the catheter goes in. This gives your bladder the best shot at recovering and voiding on its own.The Bottom Line
Anticholinergics aren’t evil. They help some people. But for men with prostate issues, the risks far outweigh the rewards. The benefit is small. The danger is real. And the alternatives are better. If you’re on one of these drugs and have BPH, ask your doctor:- Have you checked my prostate size?
- Have you measured my urine flow or post-void residual?
- Are you aware of the 2.3x higher risk of retention with these drugs?
- Have you considered mirabegron or an alpha-blocker instead?
Can anticholinergics cause urinary retention in men with BPH?
Yes. Anticholinergics reduce bladder contractions, which can make it impossible for men with an enlarged prostate to empty their bladder fully. This leads to urinary retention. Studies show men with BPH who take these drugs have a 2.3 times higher risk of acute retention compared to those who don’t.
What are the safest alternatives to anticholinergics for overactive bladder with BPH?
Alpha-blockers like tamsulosin (Flomax) and alfuzosin (Uroxatral) are first-line options-they relax the prostate and bladder neck without weakening bladder contractions. 5-alpha reductase inhibitors like finasteride shrink the prostate over time. Beta-3 agonists like mirabegron (Myrbetriq) and vibegron (Gemtesa) relax the bladder muscle without blocking acetylcholine, making them much safer for men with BPH.
How do doctors check if someone is at risk for retention before prescribing anticholinergics?
A proper evaluation includes a digital rectal exam to assess prostate size, uroflowmetry to measure urine flow speed (under 10 mL/s is high risk), and a post-void residual test to see how much urine is left after urinating. If any of these show signs of obstruction, anticholinergics should be avoided.
What should I do if I suddenly can’t urinate while taking an anticholinergic?
Seek emergency care immediately. Inability to urinate with a full bladder is a medical emergency. You’ll need a catheter to drain your bladder. Do not wait. Delaying can lead to bladder damage or kidney problems. Tell the medical team you’re on an anticholinergic-this helps them act faster.
Are anticholinergics ever safe for men with prostate issues?
Only in rare cases-men with very mild BPH, no significant obstruction, and strong bladder contractions-might they be tried under strict monitoring. This includes monthly flow tests and residual urine checks. But even then, safer alternatives like beta-3 agonists are preferred. Most experts now consider anticholinergics contraindicated in this group.
Why do some doctors still prescribe anticholinergics to men with BPH?
Many doctors aren’t aware of the updated guidelines or assume the patient’s symptoms are purely overactive bladder without checking for obstruction. Others may not have access to simple tests like uroflowmetry. Patient pressure to treat urgency quickly can also lead to shortcuts. But the risks are too high to ignore.
Is there a trend toward stopping anticholinergic use in men with BPH?
Yes. The European Association of Urology’s 2023 guidelines state anticholinergics should be avoided in men with prostate enlargement. Market analysis predicts a 35% drop in prescriptions for men over 65 with BPH by 2028. Safer drugs like vibegron and mirabegron are replacing them, and awareness of retention risks is growing among clinicians.






Swapneel Mehta
December 20, 2025 AT 17:01This is one of those posts that makes you realize how much we take our bodies for granted. I had no idea anticholinergics could do this kind of damage to men with BPH. My uncle went through exactly what you described-ended up with a catheter after being prescribed oxybutynin. No one warned him. It’s terrifying how common this is and how little awareness exists.
Stacey Smith
December 21, 2025 AT 21:20Doctors are lazy. They prescribe pills instead of thinking. This is why America’s healthcare system is broken.
Ben Warren
December 23, 2025 AT 19:58It is imperative to underscore that the pharmacological inhibition of cholinergic neurotransmission in the context of preexisting lower urinary tract obstruction constitutes a clinically significant iatrogenic risk. The American Urological Association guidelines are unequivocal in their contraindication, yet the persistence of off-label prescribing reflects a systemic failure in continuing medical education and evidence-based practice adoption. The Cochrane meta-analysis demonstrates marginal benefit, while the FDA adverse event database reveals a disturbing prevalence of iatrogenic urinary retention-particularly in geriatric male populations with documented prostatic enlargement. It is not merely a matter of caution; it is a moral imperative to cease this practice immediately.
Hannah Taylor
December 23, 2025 AT 21:22wait… so the pharma companies know this but still push these drugs? i bet they’re paying docs to ignore the warnings. and dont even get me started on the FDA being asleep at the wheel. they let this stuff through just so they can make more money. its all a scam. my cousin got catheterized after taking detrol and now she’s on a ‘special list’-like they’re tracking people who got hurt. who’s behind this?
Jason Silva
December 25, 2025 AT 00:20THIS IS WHY WE NEED TO BAN ANTICHOLINERGICS FOR OLD GUYS 😡
My dad almost died from this. They gave him oxybutynin like it was candy. Now he’s got a catheter and a new lease on life-but he’s scared to trust doctors again. 🚨 If you’re on one of these, STOP. Talk to your urologist. Beta-3 agonists exist for a reason. 🙏
mukesh matav
December 25, 2025 AT 17:23I’ve seen this in my village back in India. Elderly men are given pills without tests. No ultrasound, no flow rate, nothing. They just say ‘take this for frequent urination.’ Many end up in hospital with bloated bellies. We need better education here too.
Michael Ochieng
December 25, 2025 AT 22:02As someone who works in global health, I’ve seen this exact issue in rural clinics across Africa and Southeast Asia. The same drugs, same ignorance. It’s not just an American problem-it’s a global failure of primary care. We need simple screening tools, not just fancy guidelines no one follows.
John Hay
December 26, 2025 AT 17:23I’m a nurse. I’ve seen this too many times. Patients come in with retention after being on these meds for weeks. We catheterize them, then they ask why they can’t pee anymore. We have to explain it’s the drug. They’re always shocked. No one ever told them. This needs to be on every prescription label.
Jon Paramore
December 27, 2025 AT 16:50Uroflowmetry <10 mL/s = high risk. PVR >150 mL = contraindication. Beta-3 agonists have <5% retention in BPH vs 18% for anticholinergics. Alpha-blockers reduce post-catheter retention by 40%. Mirabegron is first-line now per EAU 2023. Stop prescribing like it’s 2010.
Cameron Hoover
December 28, 2025 AT 08:55I read this and cried. Not because I’m emotional-but because I know how many men are suffering silently. My grandfather was one of them. He never complained about not being able to pee. He just sat there, sweating, waiting for it to happen. He didn’t know it was the medicine. We didn’t either. This post? It’s a lifeline.
Teya Derksen Friesen
December 28, 2025 AT 12:01It is profoundly concerning that clinical inertia persists in the face of robust, evidence-based guidelines. The European Association of Urology’s 2023 position statement is unequivocal: anticholinergics are contraindicated in men with benign prostatic hyperplasia. The continued dissemination of these agents without mandatory pre-treatment urodynamic evaluation represents a systemic breach of the standard of care. It is not merely negligence-it is a violation of the Hippocratic oath.