Opioid-Induced Vomiting: Causes, Management, and What to Do Next
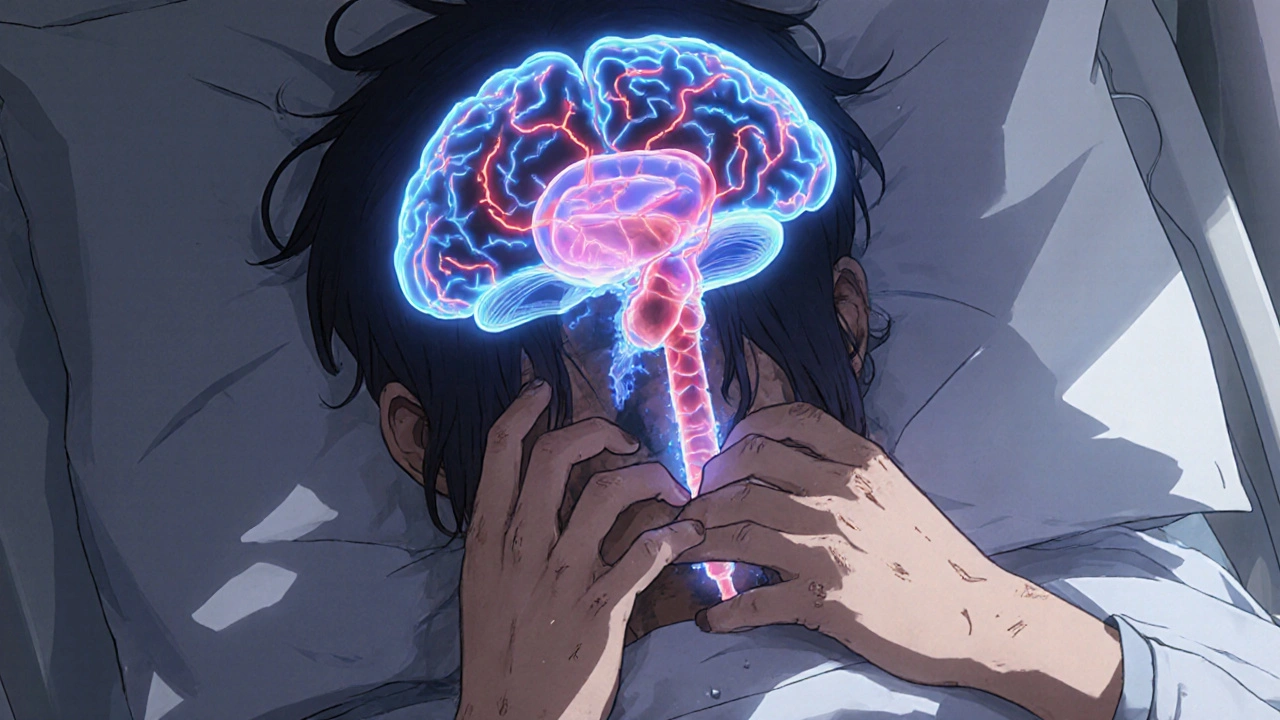
When you take opioids for pain, opioid-induced vomiting, a direct side effect caused by how opioids interact with the brain’s vomiting center. Also known as opioid-related nausea, it’s not a sign your body is rejecting the drug—it’s a built-in reaction that affects up to 40% of people starting treatment. This isn’t just discomfort. It can make you skip doses, reduce pain control, or even stop treatment entirely. And if you’re already dealing with chronic pain, adding nausea on top feels like a cruel twist.
Opioid tolerance, the body’s reduced response to a drug over time often gets confused with opioid-induced vomiting. But they’re different. Tolerance means you need higher doses to feel the same pain relief. Opioid-induced vomiting? That’s your brain’s chemoreceptor trigger zone being activated by the drug, even at low doses. You can have vomiting without tolerance—and tolerance without vomiting. Mixing them up leads to dangerous decisions, like increasing your dose just to stop nausea, which only makes things worse.
Then there’s antiemetic medications, drugs designed to block nausea and vomiting. These aren’t optional add-ons—they’re part of safe opioid therapy. Medications like ondansetron, metoclopramide, or even low-dose promethazine can cut vomiting by half. But they don’t work the same for everyone. Timing matters. Taking them 30 minutes before your opioid dose often works better than waiting until you’re already sick. And if you’re on long-term opioids, your doctor should check for other triggers: dehydration, constipation, or even other meds you’re taking that stack up on your stomach.
What’s missing in most conversations is that opioid-induced vomiting isn’t always about the drug itself. It’s also about your body’s rhythm. medication timing, when you take your pills in relation to meals, sleep, and daily cycles plays a bigger role than you think. Taking opioids on an empty stomach? Higher chance of nausea. Taking them after a light meal? Often smoother. It’s not magic—it’s biology. Your gut has its own clock, and opioids mess with it.
And here’s the thing: if you’re vomiting every time you take your opioid, you’re not weak. You’re not failing. You’re just someone who hasn’t been given the right tools. Many patients are told to "just push through"—but that’s not care, that’s neglect. The right antiemetic, the right timing, maybe even a switch to a different opioid like methadone or buprenorphine—those are real options. You don’t have to live with nausea just because you need pain relief.
The posts below dig into exactly this: how side effects like vomiting connect to broader issues like opioid tolerance, drug timing, and what actually works to fix them. You’ll find real-world advice from people who’ve been there, plus clear guidance on when to ask for help, what meds to request, and how to talk to your pharmacist about alternatives. No fluff. No guesswork. Just what to do next.
Opioid-induced nausea affects up to one-third of patients and often leads to treatment failure. Learn which antiemetics work, which are dangerous, and how to manage nausea safely without increasing overdose risk.
Recent-posts
Categories
Tags
- online pharmacy
- side effects
- drug interactions
- generic drugs
- online pharmacy UK
- drug safety
- opioid side effects
- pill organizer
- Tadalafil
- arthritis medication
- buy medication online
- prescription medication
- quit smoking
- motion sickness
- Sildenafil
- Vardenafil
- ED medication alternatives
- biologics
- medication safety
- generic medication prices