DRESS Syndrome Risk Calculator
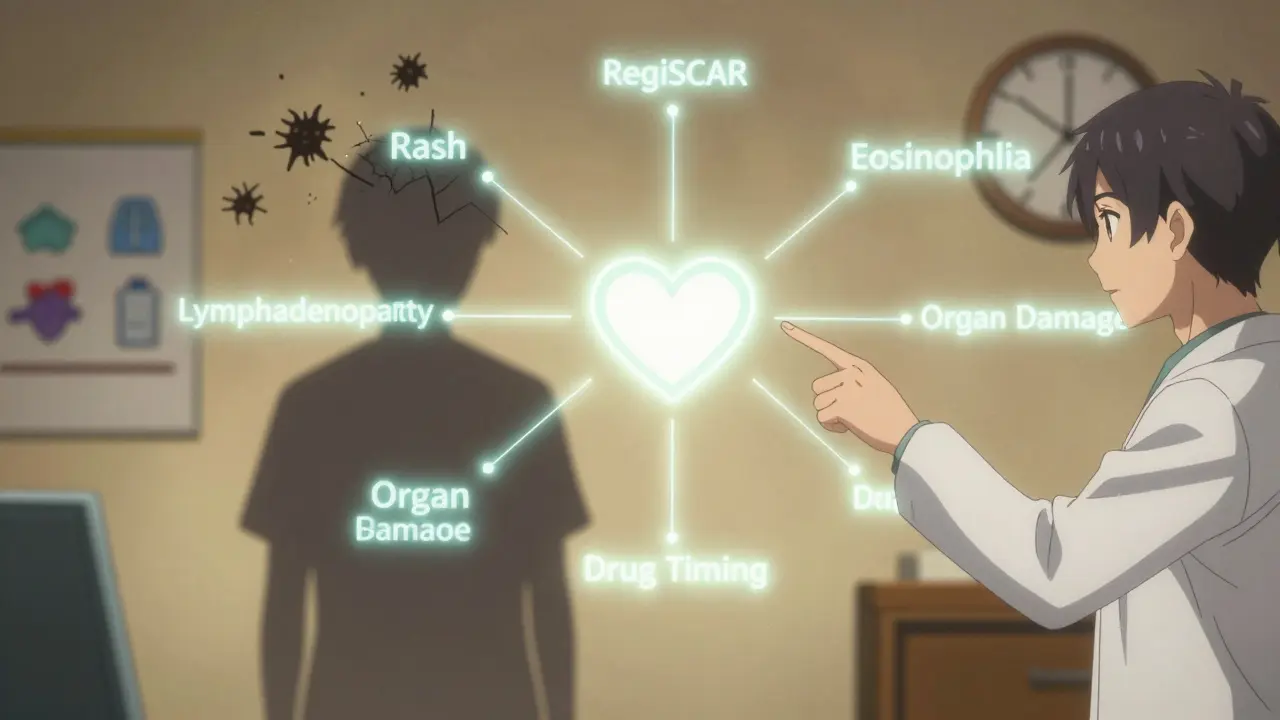
RegiSCAR Score Calculator
This tool calculates your RegiSCAR score based on clinical criteria to assess likelihood of DRESS syndrome. Important: This is not a diagnosis tool. If you suspect DRESS, stop the medication immediately and seek emergency care.
When a medication you’ve been taking for weeks suddenly triggers a full-body crisis, it’s not just a rash - it’s a red flag screaming for attention. DRESS syndrome is one of the most dangerous drug reactions doctors rarely see but must recognize immediately. It doesn’t strike overnight. It creeps in. Fever. Swelling. A spreading rash. Then, your liver starts failing. Your kidneys struggle. Your blood turns into a battlefield of rogue immune cells. And if you’re not diagnosed within days, the chance of dying rises sharply.
What Exactly Is DRESS Syndrome?
DRESS stands for Drug Reaction with Eosinophilia and Systemic Symptoms. It’s also called DIHS - Drug-Induced Hypersensitivity Syndrome. This isn’t a simple allergy. It’s a full-body immune meltdown triggered by certain medications. The reaction doesn’t happen right away. It usually shows up 2 to 8 weeks after you start the drug. That delay is why so many patients get misdiagnosed. Doctors see a fever and rash and think: flu. Allergies. A virus. But it’s not. It’s your immune system attacking your own organs because of a drug.
First identified in the 1950s with phenytoin, DRESS was formally named in 1996. Since then, studies have shown it kills about 10% of people who get it. That’s higher than many infections. And it’s not rare. About 1 in every 1,000 to 10,000 people on high-risk drugs develop it. For some, it’s a one-time nightmare. For others, it leaves lasting damage - kidney failure, thyroid disease, even autoimmune disorders years later.
The Classic Signs: More Than Just a Rash
Most people with DRESS get three things together: fever, rash, and swollen lymph nodes. But the real danger is what happens inside.
- Rash: Starts on the face and upper body - flat, red spots that spread like wildfire. Within days, it covers 80-90% of your skin. It’s not itchy like hives. It’s deep, angry, and persistent.
- Fever: Always above 38.5°C (101.3°F). Often the first sign. Not a 102°F cold - this is a steady, high fever that won’t break.
- Eosinophilia: Your blood tests show more than 1,500 eosinophils per microliter. These are white blood cells that normally fight parasites. In DRESS, they go haywire and attack your organs.
- Lymphadenopathy: Swollen glands in your neck, armpits, or groin. Not just tender - visibly enlarged.
- Organ damage: 90% of cases involve internal organs. Liver? 77% of patients have ALT levels over 300 IU/L. Kidneys? 14% show signs of failure. Lungs? Heart? Pancreas? All can be hit.
Facial swelling? Happens in 68% of cases. Cracked, dry lips? 52%. But unlike Stevens-Johnson Syndrome, severe mouth or eye sores are rare. That’s a key difference.
What Drugs Cause DRESS?
It’s not just any pill. Certain drugs have a known link. And if you have a specific gene, your risk skyrockets.
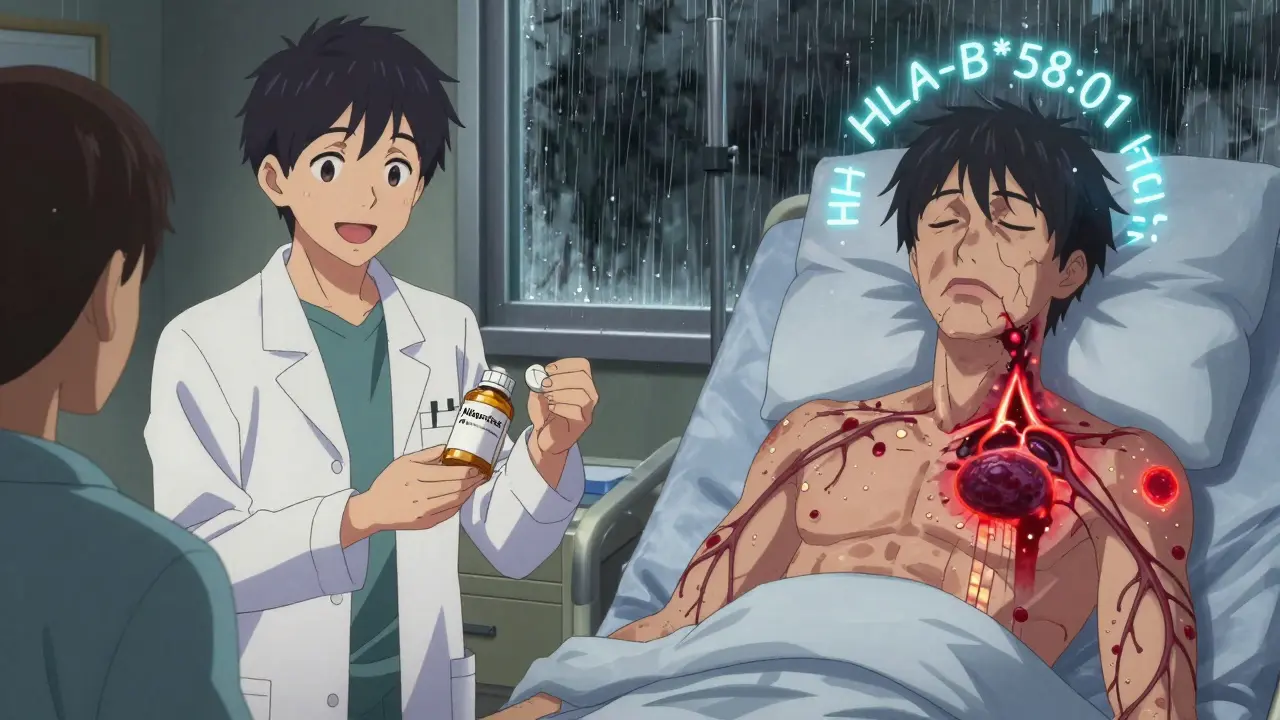
- Allopurinol (for gout): Causes 28% of all DRESS cases. If you carry the HLA-B*58:01 gene, your risk is 100 times higher. Taiwan now screens everyone before prescribing - and cut DRESS cases by 80%.
- Anticonvulsants: Carbamazepine, phenytoin, lamotrigine. 24% of cases. HLA-A*31:01 increases risk for carbamazepine.
- Antibiotics: Especially minocycline, vancomycin, sulfonamides. 20% of cases.
- Others: Dapsone, abacavir, nevirapine, and even some newer cancer drugs like checkpoint inhibitors.
Here’s the hard truth: if you’re on one of these drugs and develop a rash after 3 weeks, stop assuming it’s harmless. The longer you wait, the higher the chance of permanent organ damage or death.
Why Diagnosis Is So Hard - and So Critical
Most patients see their doctor 2-5 times before getting the right diagnosis. One Reddit user wrote: “Went to the ER three times. First time: ‘It’s a virus.’ Second: ‘Allergy.’ Third: ‘DRESS. You’re lucky you’re still alive.’”
The problem? DRESS mimics viral infections - especially when HHV-6 (a common herpes virus) reactivates in 60-80% of cases. Your body thinks it’s fighting a virus. But the trigger? A drug you took weeks ago.
The gold standard for diagnosis is the RegiSCAR scoring system. It looks at:
- Time between drug start and symptoms (2-8 weeks)
- Fever
- Rash type
- Eosinophilia
- Lymph node swelling
- Organ involvement
- Exclusion of other causes
- Response to drug withdrawal
With this system, doctors get 80% sensitivity and 97% specificity. That means it’s accurate almost every time - if used.
Yet a 2021 study found only 38% of primary care doctors could correctly identify DRESS criteria. Academic dermatologists? 89%. That gap kills people.
What Happens If You Don’t Act Fast?
Delay = danger.
One patient in the UK developed DRESS from carbamazepine. He was sent home three times with “viral illness.” On day 22, his kidneys failed. He needed dialysis. He never fully recovered. That’s not rare.
Without treatment, DRESS can lead to:
- Acute liver failure
- Renal shutdown
- Myocarditis (heart inflammation)
- Pneumonitis (lung damage)
- Chronic autoimmune thyroiditis
- Permanent organ scarring
And yes - 10% of people die. Most from sepsis, liver failure, or uncontrolled inflammation.
How Is It Treated?
Step one: Stop the drug. Immediately. No exceptions. Even if you think it’s helping you. Even if your doctor says “wait and see.”
Step two: Go to the hospital. DRESS is not an outpatient condition. You need monitoring. Blood tests. Organ support.
Step three: Corticosteroids. Prednisone is the go-to. Starting within 72 hours of diagnosis improves survival by 60-70%. The dose is high at first - often 1 mg per kg of body weight. Then it’s tapered slowly over 3 to 6 months. Too fast? The reaction comes back.
Step four: Supportive care. IV fluids, liver support, kidney monitoring. Some patients need ICU care if liver enzymes hit over 1,000 IU/L or creatinine exceeds 2.0 mg/dL.
There’s no magic cure. No FDA-approved drug just for DRESS. But steroids, when timed right, save lives.
The Future: Screening and Prevention
The biggest breakthrough? Prevention.
In Taiwan, since 2012, every patient prescribed allopurinol gets tested for HLA-B*58:01. If positive? They get a different drug. Result? An 80% drop in DRESS cases.
On March 1, 2023, the FDA approved the first point-of-care test for HLA-B*58:01. Results in under an hour. You can now screen before you even take the first pill.
Experts predict that within five years, HLA screening will be standard for all high-risk drugs. That could cut DRESS cases by 60-70%.
Meanwhile, new research is testing steroid-sparing treatments - like IVIG and mycophenolate - to reduce long-term steroid side effects. A global registry launched in September 2023 is tracking outcomes to improve care.
What Should You Do?
If you’re on one of these drugs - allopurinol, carbamazepine, lamotrigine, vancomycin, sulfonamides - and you develop:
- A rash after 3+ weeks
- Fever that won’t go away
- Swollen lymph nodes
- Unexplained fatigue or nausea
Stop the drug. Go to the ER. Demand a complete blood count with differential and liver enzymes.
If your doctor says, “It’s probably just a virus,” ask: “Could this be DRESS?” Show them the RegiSCAR criteria. Bring a printout. Most have never seen it. But you can save your life by asking.
DRESS isn’t common. But it’s deadly. And it’s preventable. Knowledge isn’t just power - it’s your next heartbeat.