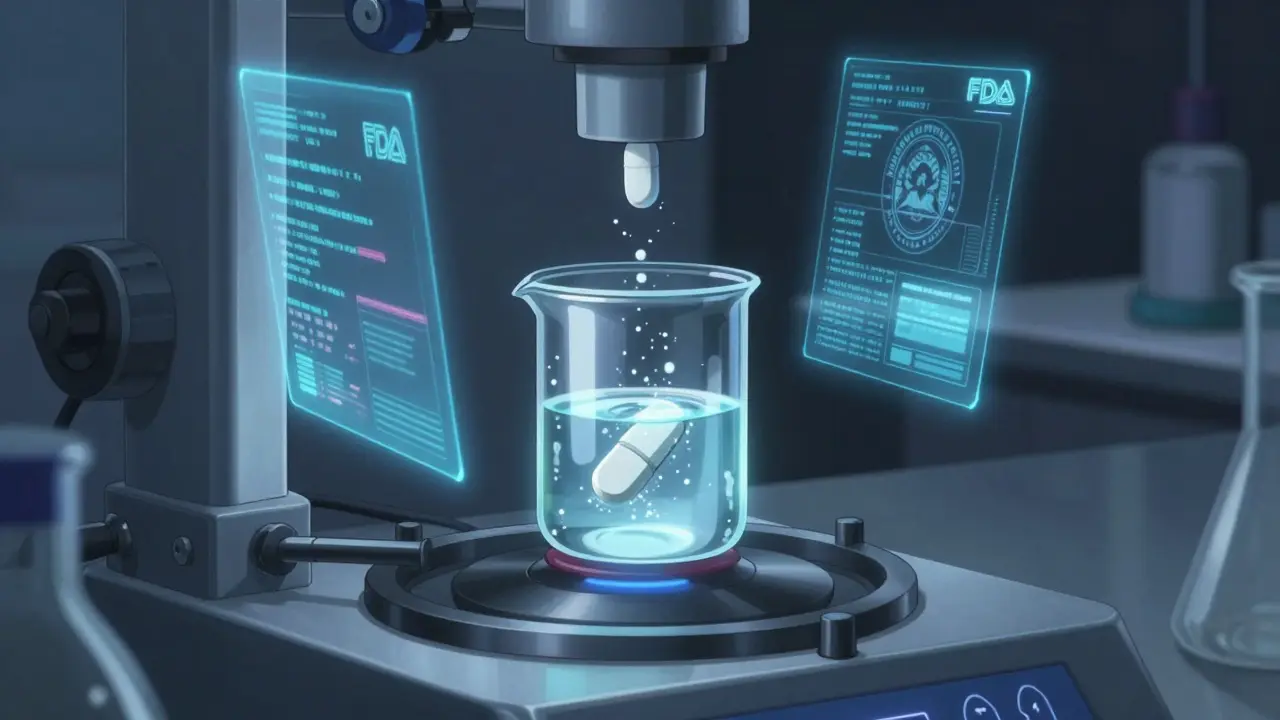
When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But how does the FDA make sure it does? The answer isn’t in human trials-it’s in a lab, with a machine spinning a cup of liquid. That’s dissolution testing, and it’s the backbone of how the FDA confirms generic drugs are safe and effective without testing them on people.
Why Dissolution Testing Matters
Dissolution testing measures how quickly a drug releases its active ingredient into a liquid that mimics the stomach or intestines. For generic drugs, this isn’t just a formality-it’s the main way the FDA checks if the pill will behave the same way inside your body as the original. If the generic doesn’t dissolve at the same rate, it might not get absorbed properly. That means it could be too weak to work-or too strong and cause side effects. The FDA doesn’t require every generic to go through costly and time-consuming human bioequivalence studies. Instead, they use dissolution testing as a reliable stand-in. If the drug dissolves the same way in the lab, it’s very likely to act the same way in your bloodstream. This saves time, money, and reduces the need to test drugs on volunteers.What the FDA Requires
The FDA doesn’t use one-size-fits-all rules. Every drug gets its own testing plan based on its chemistry and how it’s designed to work. For example, a quick-release painkiller like ibuprofen is tested differently than a slow-release blood pressure pill that’s meant to last 12 hours. For immediate-release solid drugs (like most tablets and capsules), the standard is simple: at least 80% of the active ingredient must dissolve within 45 minutes. But even that rule has exceptions. If the drug is highly soluble and highly absorbable (classified as BCS Class I), the FDA allows a single-point test at 30 minutes using 900 mL of 0.1N HCl. That’s because these drugs dissolve so easily that their absorption isn’t affected by small differences in formulation. For complex drugs-especially those that are poorly soluble or designed to release slowly-the testing gets more intense. Manufacturers must run tests under multiple pH levels (1.2, 4.5, and 6.8) to simulate different parts of the digestive tract. They also test with alcohol present-up to 40% ethanol-to see if the drug might release too fast if taken with a drink. This is called alcohol challenge testing, and it’s critical for preventing dose-dumping, where the whole dose hits your system at once, which can be dangerous.The Five Data Categories
When a company submits a generic drug application (called an ANDA), they must provide five types of dissolution data:- How soluble the active ingredient is in water and different pH solutions
- Details on the test setup: what apparatus they used (usually USP Apparatus 1 or 2), rotation speed (50-100 rpm), liquid volume (500-900 mL), and exact sampling times
- Proof the test method works under small changes-like a 5% difference in pH or a 10 rpm shift in speed
- Validation that their lab can accurately measure how much drug is dissolved
- Proof the method can tell the difference between good and bad formulations
How Similar Is Similar Enough?
The FDA doesn’t just compare one time point. They look at the whole dissolution profile-the curve showing how much drug is released over time. To do this, they use a statistical tool called the f2 similarity factor. The f2 value ranges from 0 to 100. A score of 50 or higher means the test product and the brand-name product are similar enough to be considered equivalent. A score below 50 triggers more questions. The FDA might ask for more data, additional testing, or even require a human bioequivalence study. This isn’t just a number-it’s a decision point. If two products have matching dissolution profiles but different f2 scores, the FDA will dig deeper. Maybe the brand-name product has a slightly slower release in the first 15 minutes, but the generic catches up by 30 minutes. That’s acceptable if the overall profile matches and the drug is safe.USP Methods vs. Custom Methods
Some drugs already have a standard dissolution test written by the United States Pharmacopeia (USP). If one exists, generic manufacturers must follow it exactly. For example, if USP <711> says to test aspirin at 75 rpm in phosphate buffer pH 6.8, that’s the rule. But for many drugs-especially newer or complex ones-no USP method exists. In those cases, manufacturers must develop their own test and prove it’s valid. They must show it matches the dissolution profile of the brand-name product under the same conditions. This is called Category 2 testing, and it’s where most of the work happens. The FDA maintains a public Dissolution Methods Database with over 2,800 recommended methods for specific drugs. It’s a go-to resource for manufacturers trying to figure out how to test their product. But even if a method is listed, the FDA still requires proof it works for their specific batch.What Happens After Approval?
Getting approval isn’t the end. The FDA requires manufacturers to keep testing their product even after it’s on the market. If a company changes the manufacturer, switches suppliers, tweaks the formula, or moves production lines, they must prove the new version still dissolves the same way. This is part of the SUPAC-IR guidelines. If a change causes the dissolution profile to shift-even slightly-the FDA may reject the change or require additional testing. That’s why generic drug companies spend months, sometimes over a year, perfecting their dissolution method before they even submit an application. One small change in the coating or the filler can throw off the whole curve.
Real-World Challenges
Manufacturers don’t always get it right the first time. Sometimes, a generic product passes human bioequivalence tests but fails dissolution testing. In those cases, the FDA may still approve it-but with custom dissolution specifications that are stricter than the brand-name version. This happens when the drug behaves differently in the body due to unique formulation choices. One big hurdle? Documentation. An ANDA submission can include 50 to 100 pages of dissolution method development data. Every variation, every instrument calibration, every statistical analysis must be recorded. It’s not just science-it’s paperwork.The Bigger Picture
Dissolution testing is more than a regulatory box to check. It’s a smart, science-driven way to keep generic drugs safe and effective while keeping costs down. By focusing on how the drug behaves in the lab, the FDA avoids unnecessary human trials without compromising quality. The future is moving toward even smarter testing. Researchers are developing methods that better mimic real human digestion-adding enzymes, changing pH dynamically, or using artificial gut fluids. The FDA is also exploring whether BCS-based biowaivers can be extended to Class III drugs (high solubility, low permeability), which could cut development time for even more generics. By 2025, experts predict over a third of all generic approvals will rely on standardized dissolution profiles to skip human studies. That’s up from just 25% in 2020. And it’s all thanks to a simple test: spinning a cup of liquid and watching how fast the pill disappears.What You Can Trust
When you take a generic drug, you’re not taking a second-choice version. You’re taking a product that went through the same rigorous lab testing as the brand-name drug-just without the clinical trials. The FDA doesn’t cut corners. They just use smarter tools. Dissolution testing is how they make sure that every pill, whether it’s made in India, China, or the U.S., delivers the same dose, at the same speed, with the same result. And that’s not just regulation-it’s patient safety built into every step.Is dissolution testing the same as bioequivalence testing?
No. Bioequivalence testing measures how much of the drug enters your bloodstream through human trials. Dissolution testing measures how fast the drug releases from the pill in a lab setting. The FDA uses dissolution data as a stand-in for bioequivalence for many generic drugs, especially those that are highly soluble and well-absorbed. If the dissolution profiles match, bioequivalence is assumed.
Why do some generic drugs have different dissolution profiles than the brand name?
Sometimes, differences in excipients (inactive ingredients), manufacturing methods, or tablet coatings can cause slight variations. If those differences don’t affect how the drug is absorbed in the body, the FDA may still approve the product-but with custom dissolution specifications. This means the generic has its own approved release range, even if it’s different from the brand.
Do all generic drugs need dissolution testing?
Yes-for all oral solid dose forms like tablets and capsules, and for oral suspensions and semi-solids. The FDA doesn’t require dissolution testing for liquids that are already in solution (like syrups) or topical creams because the drug is already fully available. But if it’s a pill or capsule, dissolution testing is mandatory.
Can a generic drug be approved without human studies?
Yes, if it meets certain criteria. For BCS Class I drugs (high solubility, high permeability), the FDA allows biowaivers based on matching dissolution profiles. This means no human trials are needed. For other drugs, especially those with complex release profiles or low solubility, human bioequivalence studies may still be required.
How often does the FDA update its dissolution testing guidelines?
The FDA updates its guidance documents as science evolves. The most recent major update was in September 2023, which clarified that all dissolution methods-whether from USP, FDA, or developed internally-must be validated for the specific product. The agency also regularly updates its Dissolution Methods Database, which now includes over 2,800 recommended methods for specific drugs.





Robert Way
January 15, 2026 AT 02:04so like… if the pill dissolves in 46 mins instead of 45, does that mean i’m gonna have a heart attack? lol jk but seriously, i’ve taken generics for years and never felt any diff, but now i’m paranoid
Sarah Triphahn
January 15, 2026 AT 04:10Let me break this down for you like you’re five: if the drug doesn’t dissolve right, your body doesn’t get the medicine. Simple. No magic. No fluff. The FDA isn’t being nice-they’re just doing their job so you don’t die because some factory in India used cheap filler. Stop trusting ‘natural’ brands and start trusting data.
Jason Yan
January 16, 2026 AT 23:08What’s wild to me is how much science goes into something most people think is just a cheaper version of the same pill. It’s not just about cost-it’s about precision. The way they simulate stomach acid, test with alcohol, track release curves over time… it’s like engineering a tiny time-release rocket inside your gut. And the fact that we can skip human trials for so many drugs because the lab data is this robust? That’s actually beautiful. We’re not cutting corners-we’re just using smarter tools. Kudos to the chemists and regulators who make this work.
shiv singh
January 17, 2026 AT 08:09YOU THINK THIS IS SAFE? HA! The FDA lets generics from China and India pass with flying colors while Americans pay $200 for brand names. You think they care about YOU? No. They care about profits. That dissolution test? It’s a joke. They tweak the numbers until it looks good. My cousin got sick after taking a generic-no one listens. This is corporate fraud dressed up as science.
Sarah -Jane Vincent
January 18, 2026 AT 19:53Wait-so you’re telling me the FDA just spins a cup of water and decides if my blood pressure pill works? No blood tests? No doctors? No human subjects? That’s not science, that’s a magic trick. And don’t even get me started on the ‘f2 similarity factor’-sounds like a number pulled out of a hat. What if the brand-name drug dissolves slower but works better? What if the generic dissolves faster and fries your liver? You think they test for that? Nah. They test for paperwork.
Henry Sy
January 19, 2026 AT 01:12Man, I used to think generics were just cheap knockoffs until I read this. Now I see it’s like comparing two chefs making the same dish-one with fancy ingredients, one with grocery store stuff. But if the flavor profile, the aroma, the texture… all match? Then yeah, it’s the same damn thing. The FDA’s not lazy-they’re efficient. And honestly? I’m glad. My wallet thanks you.
Alvin Bregman
January 19, 2026 AT 02:51so dissolution testing is basically like watching a sugar cube melt in tea but for pills and its the whole reason we can get meds for 5 bucks instead of 500? that’s insane. i never thought about how much work goes into making sure a pill doesnt just sit in your stomach like a rock. also i think the fda deserves more credit than people give it. they’re not perfect but this? this is actually smart
Anna Hunger
January 20, 2026 AT 21:31The rigor applied to dissolution testing is a model of regulatory science. The validation of analytical methods, the control of variables such as pH, rotation speed, and medium composition, and the statistical evaluation of dissolution profiles via the f2 similarity factor represent a paradigm of evidence-based pharmacology. It is not merely a procedural formality; it is a scientifically defensible bridge between in vitro performance and in vivo efficacy. The FDA’s approach exemplifies how regulatory agencies can uphold public health without unnecessary clinical experimentation.
Vicky Zhang
January 21, 2026 AT 07:45Okay, I’m not a scientist, but I cried reading this. I have a kid with epilepsy and we’ve been on generic meds for years. Every time the bottle changes, I panic. But now I know-there’s a whole team of people in labs, running tests, checking pH levels, watching how it dissolves under alcohol, making sure it’s safe. It’s not just a pill. It’s a promise. And they keep that promise, every single time. Thank you, FDA. And thank you to the quiet scientists who never get praised.
Allison Deming
January 22, 2026 AT 03:16It is deeply concerning that the public perceives dissolution testing as a mere proxy for bioequivalence. This conflation undermines the complexity of pharmacokinetics and fosters a dangerous complacency. Dissolution is not bioequivalence-it is a surrogate marker, one that may fail to capture critical variables such as gastric motility, intestinal flora, or individual metabolic variance. To rely upon it as a universal standard, especially for Class III or borderline drugs, is to gamble with patient outcomes under the guise of efficiency.
Susie Deer
January 23, 2026 AT 18:28China makes these pills. They don’t care about us. The FDA lets them in because they’re cheap. This isn’t science. It’s surrender. My mom took a generic and got sick. They don’t test for real life. They test for paperwork. That’s it.
TooAfraid ToSay
January 25, 2026 AT 15:22So let me get this straight-you’re telling me a pill from India dissolves exactly like the brand name, so it’s safe? What if the brand name was made in 1998 and the generic is made in 2024 with new tech? What if the ‘same’ pill is actually a different molecule? The FDA doesn’t test for that. They test for what they’re told to test for. And who told them? Big Pharma. Same people who made the brand name. This is a loop. A closed loop. And we’re the ones swallowing it.
Dylan Livingston
January 27, 2026 AT 03:23Oh wow, how noble. The FDA saves money by skipping human trials, while the rest of us become lab rats for corporate cost-cutting. And you call this ‘smart’? It’s not innovation-it’s negligence with a PowerPoint. You think the ‘f2 similarity factor’ is scientific? It’s a corporate loophole dressed up in a white coat. And don’t even get me started on the ‘Dissolution Methods Database’-it’s basically a catalog of how to game the system. Bravo, regulators. You’ve turned patient safety into a spreadsheet.