When you're taking an ACE inhibitor like lisinopril, your blood pressure is under control - but your body might be holding onto more potassium than you realize. This isn't just a theoretical concern. Every year, thousands of people on these common blood pressure meds end up in the hospital because their potassium levels climbed too high, often without warning. And the culprit? Sometimes, it's not a drug interaction at all - it's what they ate for breakfast.
How ACE Inhibitors Raise Potassium Levels
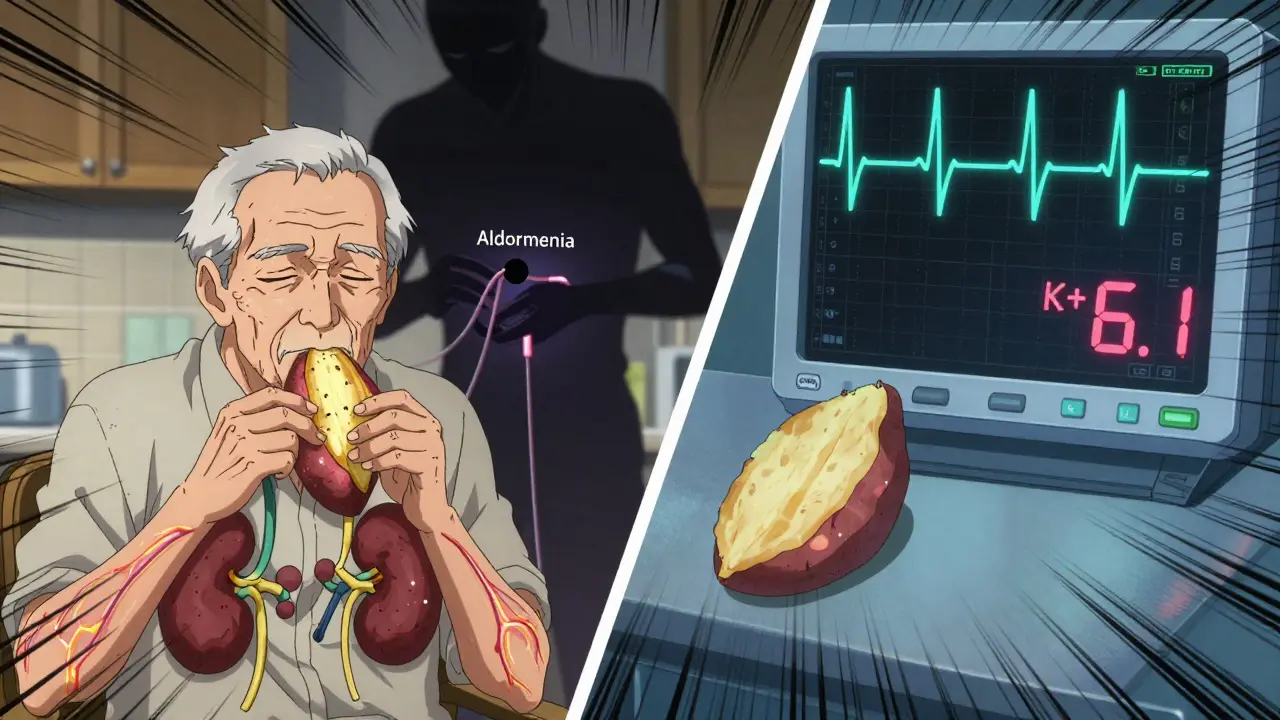
ACE inhibitors work by blocking a chemical in your body called angiotensin-converting enzyme. That sounds complicated, but here's the simple version: this enzyme normally tells your kidneys to get rid of sodium and water, and also to release a hormone called aldosterone. Aldosterone is the key player here - it tells your kidneys to dump potassium out in your urine. When ACE inhibitors shut that down, aldosterone drops. And when aldosterone drops, your kidneys stop flushing out potassium like they used to.
That means even if you eat the same amount of potassium as always, your body now holds onto more of it. For most people with healthy kidneys, this increase is small - maybe 0.5 to 1.0 mmol/L. But for someone with kidney disease, diabetes, or just older age? That number can jump 1.5 mmol/L or more. And when serum potassium hits above 5.0 mmol/L, you're in danger zone territory. Above 6.0? That's a medical emergency. Irregular heartbeat, muscle weakness, nausea - and in worst cases, cardiac arrest.
Which Foods Are the Real Culprits?
You don’t need to cut out all fruits and veggies. But some foods pack a serious potassium punch that can tip the scale when you're on an ACE inhibitor. Here’s what to watch for:
- Bananas - 326 mg per medium fruit. Two a day? That’s over 600 mg just from bananas.
- Avocados - 507 mg per 100 grams. One avocado can give you nearly half your daily limit.
- White and sweet potatoes - 379 mg and 670 mg per 100g, respectively. Baked potato with skin? That’s close to 1,000 mg.
- Tomatoes and tomato products - 193 mg per 100g, but most people eat a lot more than that. Tomato sauce, salsa, canned tomatoes? They add up fast.
- Dried fruits - apricots, raisins, prunes. A small handful can contain 300-500 mg.
- Salt substitutes - products like Nu-Salt or NoSalt replace sodium with potassium chloride. Just 1.25 grams can contain 525 mg of potassium. Many people think they’re being healthy by using these - they’re not.
- Coconut water - 1,500 mg per serving. Yes, it’s natural. Yes, it’s marketed as a health drink. And yes, it’s landed multiple patients in the ER on lisinopril.
Here’s the thing: if you’re eating three servings of high-potassium foods daily and taking your ACE inhibitor, you’re stacking risk. A single high-potassium meal can spike serum potassium by 0.3-0.8 mmol/L within a few hours. That’s enough to push someone on the edge over the line.
Who’s Most at Risk?
Not everyone on ACE inhibitors needs to panic. But some groups are far more vulnerable:
- People with chronic kidney disease (CKD) - If you’re in stage 3 or 4, your risk of hyperkalemia jumps to nearly 13% per year. That’s more than 10 times higher than someone with healthy kidneys.
- Diabetics - Diabetes damages the kidneys over time. Even if your blood tests look fine, your kidneys might not be handling potassium like they should. Risk is 3.2 times higher.
- Older adults - Kidney function naturally declines with age. Many seniors don’t even know they have mild CKD until they get a potassium test.
- Those on other potassium-raising drugs - If you’re also taking spironolactone, eplerenone, or trimethoprim, your risk skyrockets. Studies show a 300-400% increase in hyperkalemia when these are combined with ACE inhibitors.
And here’s the scary part: many people don’t feel symptoms until it’s too late. Muscle weakness? You blame it on getting older. Nausea? You think it’s a stomach bug. An irregular heartbeat? You chalk it up to stress. By the time you realize something’s wrong, you might already be in cardiac distress.
What the Experts Really Say
There’s a split in the medical community. Some doctors, like Dr. Alan Gradman, argue that dietary potassium alone rarely causes serious hyperkalemia in people with normal kidney function. Others, like Dr. Suzanne Oparil, warn that the cumulative effect - especially in older adults with hidden kidney issues - is dangerous and often ignored.
And then there’s the data that flips the script. A 2016 study in the Journal of the American College of Cardiology found that people on ACE inhibitors who ate 3,400-4,700 mg of potassium daily didn’t develop hyperkalemia - as long as their kidneys were working well. That suggests blanket restrictions might be outdated.
The real answer? It’s not one-size-fits-all. Your kidney function, your age, your other meds, your diet - all of it matters. A 65-year-old diabetic woman on lisinopril and a 45-year-old man with normal kidneys and no other conditions? They need completely different advice.
What Should You Actually Do?
Here’s the practical, no-nonsense plan:
- Get a baseline potassium test before starting an ACE inhibitor. And get retested 1-2 weeks after starting or changing your dose.
- Monitor regularly - Every 3-6 months if you’re stable with normal kidney function. Monthly if you have diabetes or CKD.
- Know your numbers - Normal potassium is 3.5-5.0 mmol/L. Anything above 5.0 needs attention. Above 6.0? Call your doctor immediately.
- Don’t panic over bananas - One banana a day is usually fine if your kidneys are healthy. But two bananas, plus tomato sauce on pasta, plus a handful of raisins, plus salt substitute? That’s asking for trouble.
- Avoid salt substitutes - Seriously. They’re not safer. They’re just potassium bombs.
- Space out your meals - Eating high-potassium foods 2 hours before or after your ACE inhibitor dose can reduce the peak spike by 25%. It’s a small change with real impact.
- Ask about alternatives - If you’re at high risk and keep struggling with potassium, talk to your doctor about ARBs (like losartan). They carry similar blood pressure benefits with slightly lower potassium risk.
And if you’re eating a lot of potatoes, tomatoes, or dried fruit? Don’t just cut them out - swap them. Try apples instead of bananas. Cucumber instead of avocado. White rice instead of sweet potato. You can still eat a healthy, colorful diet - you just need to be smart about it.
What’s New in 2026?
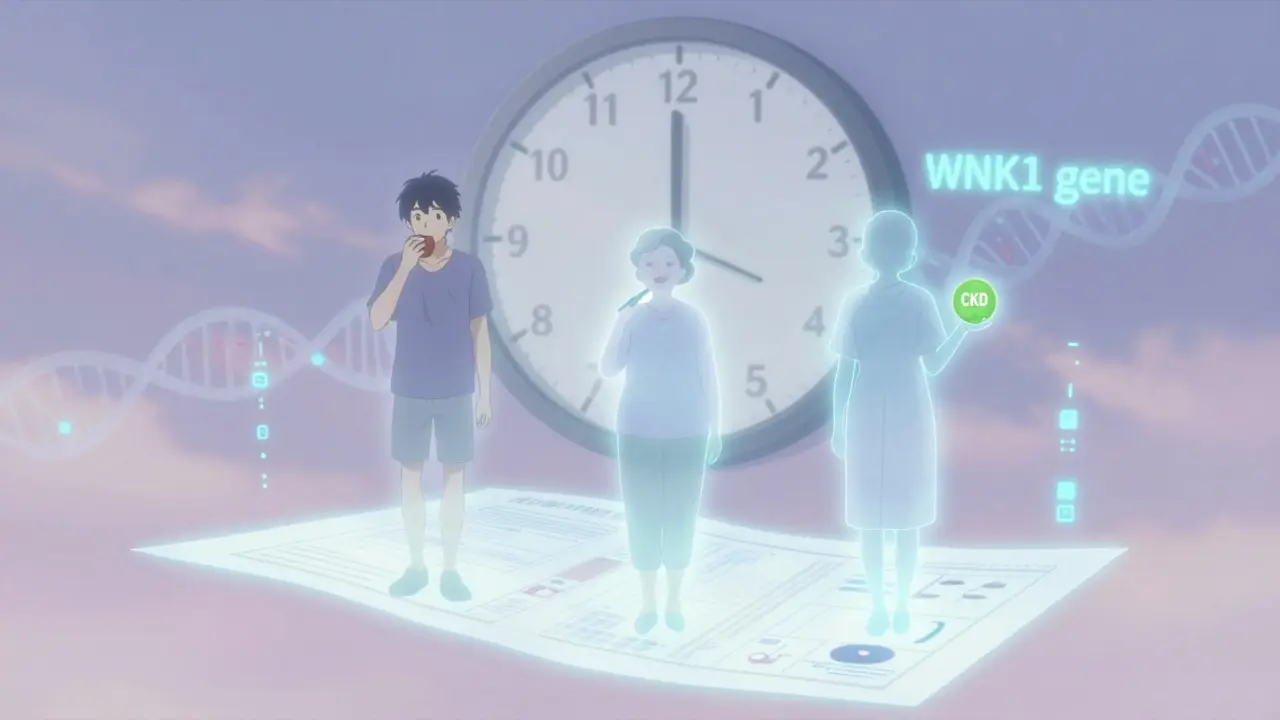
Science is moving past blanket warnings. In 2023, researchers found that a genetic variation in the WNK1 gene can identify people at 5 times higher risk for hyperkalemia on ACE inhibitors. That means in the near future, a simple genetic test could tell your doctor whether you’re one of the rare people who can safely eat avocados daily - or if you need to be extra careful.
There’s also a new drug called patiromer (Veltassa) that binds potassium in your gut and removes it from your body. It’s not a magic fix, but for people who need to stay on ACE inhibitors but keep getting high potassium, it’s a game-changer. Clinical trials show 89% of patients were able to continue their life-saving blood pressure meds without stopping.
The message now? Don’t fear potassium. Don’t avoid it completely. Just manage it - with testing, awareness, and smart choices.
Real Stories, Real Risks
One Reddit user, a nurse named CardioNurseRN, said she’s seen at least a dozen patients hospitalized after drinking coconut water daily while on lisinopril. Most were elderly, had no idea they had early kidney disease, and thought they were doing something healthy.
Another patient on Drugs.com said her potassium shot up to 5.8 after eating two bananas every morning. Her doctor had never mentioned the risk.
But here’s the flip side: a survey of over 1,200 people on ACE inhibitors found 68% had no issues with moderate potassium intake - under 2,000 mg per day. That’s the sweet spot for most people: enough to get nutrients, not enough to overload your kidneys.
The takeaway? Listen to your body. Know your numbers. Don’t assume you’re fine because you feel fine. And if you’re unsure? Get tested. It’s a simple blood test. It could save your life.
Can I still eat bananas if I take ACE inhibitors?
Yes - one banana a day is usually fine if your kidneys are healthy and your potassium levels are normal. But if you have kidney disease, diabetes, or are over 65, even one banana a day could add up. Talk to your doctor and get your levels checked before assuming it’s safe.
Is potassium always dangerous with ACE inhibitors?
No. Potassium is essential. The problem isn’t potassium itself - it’s your body holding onto too much of it because the medication reduces how much your kidneys can flush out. People with healthy kidneys can usually handle normal dietary potassium without issue. The risk is for those with kidney problems, older adults, or those on multiple medications that raise potassium.
How often should I get my potassium checked?
Before starting an ACE inhibitor, get a baseline test. Then, retest 1-2 weeks after starting or changing your dose. If your levels are normal and you have healthy kidneys, check every 3-6 months. If you have diabetes or chronic kidney disease, check monthly. Don’t wait until you feel sick - symptoms often appear too late.
What are the symptoms of high potassium?
High potassium often has no symptoms at first. When they do appear, they include muscle weakness, fatigue, tingling, nausea, irregular heartbeat, or palpitations. In severe cases (potassium above 6.0), you can develop life-threatening heart rhythm problems. If you’re on an ACE inhibitor and suddenly feel weak or your heart feels off, get checked immediately.
Should I stop eating vegetables if I’m on ACE inhibitors?
Absolutely not. Vegetables are full of nutrients that protect your heart and blood vessels. The goal isn’t to eliminate potassium - it’s to avoid extreme amounts and know your limits. Swap out the highest-potassium veggies (like potatoes and tomatoes) for lower ones (like cabbage, green beans, or bell peppers). You can still eat a colorful, healthy diet - just be mindful.
Are there alternatives to ACE inhibitors if potassium is a problem?
Yes. Angiotensin II receptor blockers (ARBs) like losartan or valsartan work similarly to ACE inhibitors but carry a slightly lower risk of hyperkalemia. They’re often used as alternatives if potassium becomes hard to manage. Your doctor can evaluate whether switching makes sense based on your health history and kidney function.







Charlotte Dacre
February 14, 2026 AT 18:26So let me get this straight - we’re telling people to avoid avocados because of a blood pressure med? Bro, I’m gonna need a new life plan. Next you’ll tell me to stop breathing because oxygen might ‘interact’ with my lisinopril. 😂
One banana a day? Cool. Two? ‘Danger zone.’ Three? ‘Cardiac arrest incoming.’ At this rate, I’m gonna have to start eating dirt like a caveman just to survive.
Also, coconut water? The same stuff that’s in every yoga studio and influencer’s morning routine? Yeah, it’s a ‘potassium bomb.’ So… is my $8 smoothie now a weapon of mass destruction? Thanks, healthcare industrial complex.
And don’t even get me started on salt substitutes. You mean to tell me the one thing I thought was helping me - swapping out sodium for ‘natural’ potassium - is actually the villain? I feel betrayed. By my own health choices.
Meanwhile, my 72-year-old aunt who eats three bananas, a whole avocado, and drinks coconut water daily is still hiking Machu Picchu. Her potassium? Normal. Her doctor? Confused. Her attitude? Unbothered. Maybe the real issue isn’t the food - it’s the fearmongering.
Let’s not turn nutrition into a minefield. People aren’t lab rats. We’re humans who like food. If you have healthy kidneys, stop panicking. If you don’t? Get tested. Don’t let a blog post turn your diet into a prison sentence.
Also, who decided ‘high potassium’ = bad? Potassium is literally the reason your heart doesn’t stop. Maybe we should stop treating it like a toxic villain and start treating it like the superhero it is.
TL;DR: One banana won’t kill you. Fear will.
Esha Pathak
February 16, 2026 AT 08:22Life is a river, and potassium is its current - sometimes gentle, sometimes fierce 🌊
We cling to pills like lifelines, yet forget the ocean within us. ACE inhibitors? They are not enemies. They are mirrors - reflecting the silent decay of our kidneys, the quiet rebellion of aging, the hidden fractures in our biology.
Avocados? Bananas? They are not the culprits. They are the messengers. They whisper: ‘You are not as young as you think. You are not as healthy as you believe.’
And yet… we rage at the fruit. We curse the coconut water. We banish the potato. But the real tragedy? We refuse to look inward.
When the body screams, we blame the menu. When the soul trembles, we reach for another pill. But healing is not subtraction. It is harmony.
Let the banana be. Let the avocado bloom. But let us also listen - to our kidneys, to our pulse, to the quiet voice beneath the noise.
Not all who eat high-potassium foods are doomed. Not all who fear them are wise.
Balance is the ancient art. Not fear. Not rules. Not labels.
Just… presence.
Mike Hammer
February 16, 2026 AT 14:46bro i just took lisinopril last week and i ate a whole bag of raisins yesterday and i’m still standing
also i drank coconut water after a workout and i didn’t die so… maybe the real danger is overthinking this?
my grandpa’s been on this med for 12 years and he eats sweet potatoes like they’re candy. he’s 81. still drives. still argues with the cable guy. his potassium? fine.
so like… if you got normal kidneys, chill. if you got kidney issues? get tested. don’t just go full doomscroll on every food blog.
also salt substitutes? yeah those are wild. i thought they were like, ‘healthy sodium’ but turns out they’re just potassium in disguise. who designed this system?
tl;dr: don’t be scared of food. be scared of ignoring your doctor.
Daniel Dover
February 18, 2026 AT 03:20One banana a day is fine. That’s all.
Chiruvella Pardha Krishna
February 20, 2026 AT 01:26The human body is not a machine with fixed thresholds. It is a symphony - and potassium is one note among many.
When we reduce health to numbers - 3.5 to 5.0 mmol/L - we forget that life is lived in gradients, not binary zones.
A diabetic with stage 3 CKD? Yes, caution is wise. But a healthy 45-year-old who eats a banana and a tomato salad? That is not a risk - it is a celebration of nourishment.
The fear of potassium is not medical. It is cultural. It is the fear of abundance. The fear of nature’s generosity.
We have been taught to distrust food. To count, to restrict, to fear.
But the truth? Your kidneys know what to do. Trust them. Test them. Do not imprison yourself in the diet of a spreadsheet.
Let the avocado grow. Let the banana ripen. Let the body breathe.
Joe Grushkin
February 21, 2026 AT 14:40So now we’re telling people they can’t eat fruit because of a drug? That’s not medicine. That’s corporate pharmacy conditioning.
Let me guess - the same people who told you to avoid saturated fat are now telling you to avoid potassium. Next they’ll say sunlight causes cancer.
Every single ‘health warning’ in modern medicine has been flipped within a decade. Remember eggs? Butter? Salt? Now they’re back. Because science isn’t dogma - it’s revision.
And coconut water? You’re telling me the same drink that athletes use to recover is a ‘potassium bomb’? That’s like saying water is dangerous because it’s wet.
Bottom line: if your doctor didn’t warn you, they’re incompetent. Don’t blame the banana. Blame the system.
Virginia Kimball
February 21, 2026 AT 15:55Y’all are overcomplicating this SO much 😊
One banana? Fine. Two? Maybe check in with your doc. Three? Yeah, maybe ease up.
But here’s the beautiful part - you can still eat ALL the veggies. Just swap out the super-high ones for lower ones. Like, have zucchini instead of sweet potato. Apples instead of prunes. Cucumber instead of avocado.
You don’t have to give up flavor or nutrition. You just need to be a little smart.
And if you’re worried? Get a simple blood test. It takes 5 minutes. It could save your life. No shame. No fear. Just care.
You’ve got this. And hey - if you’re reading this? You’re already doing better than most.
Kapil Verma
February 22, 2026 AT 08:11Western medicine is a scam. You people are being manipulated into fearing food because the pharmaceutical industry profits from your confusion.
Traditional Indian diets have lasted for millennia. We ate bananas, lentils, coconut, and salted vegetables - and our elders lived to 90+ without drugs.
Now you tell us to avoid potassium? That’s not health. That’s colonial mindset. You’re replacing ancient wisdom with lab tests and fear.
Do you know what real medicine is? It’s balance. It’s food as medicine. It’s not banning bananas because some lab number is ‘off’.
Stop listening to American doctors. Go back to your roots. Eat real food. Let your body heal itself.
And if you’re diabetic? That’s a lifestyle issue. Not a potassium issue.
Michael Page
February 22, 2026 AT 22:24There’s a difference between ‘risk’ and ‘inevitability.’
Most people on ACE inhibitors will never develop hyperkalemia. But for those who do, the consequences are severe - and often silent.
The problem isn’t the food. It’s the assumption that ‘if I feel fine, I’m fine.’
That’s the real danger. Not the avocado. Not the banana. The complacency.
Testing is free. It’s accessible. It’s non-invasive.
Why wouldn’t you do it?
Because it’s inconvenient? Because you don’t want to face it?
That’s the tragedy.
Mandeep Singh
February 23, 2026 AT 06:01Oh wow. So now we’re going full panic mode because of a few fruits? Let me tell you something - I’ve been on lisinopril for 7 years. I eat 2 avocados a week. I drink coconut water every Sunday. I eat sweet potatoes like they’re going out of style. My potassium? 4.2. Always has been.
Why? Because I get tested. Every 3 months. Like clockwork. Not because I’m scared. Because I’m responsible.
But you people? You read one article and suddenly you’re deleting your entire fruit basket. You’re turning healthy eating into a guilt trip.
Here’s the truth: the real problem isn’t potassium. It’s ignorance. It’s the refusal to get a simple blood test. It’s the belief that ‘if I don’t feel sick, I’m fine.’
Get tested. Don’t guess. Don’t fear. Don’t delete your groceries. Just… check.
And if you’re too lazy? Then maybe you shouldn’t be on the med in the first place.
Betty Kirby
February 25, 2026 AT 00:40Let’s be real - if you’re eating coconut water daily and don’t know your kidney function, you’re playing Russian roulette with your heart.
And don’t give me that ‘my grandpa did it’ nonsense. He’s 81. He’s still here. But how many others aren’t? How many died quietly in their sleep because no one thought to check?
There’s a reason hospitals see a spike in hyperkalemia cases in winter. It’s not cold weather. It’s holiday meals. Turkey. Potatoes. Tomato sauce. Bananas. Salt substitutes. Coconut water.
People aren’t dying because of bananas. They’re dying because they didn’t get a simple test.
Stop romanticizing ignorance.
Testing isn’t paranoia. It’s self-respect.
Josiah Demara
February 26, 2026 AT 05:54Let’s dissect this with surgical precision
The 2016 JACC study cited? It had selection bias. Healthy volunteers. No comorbidities. No age >65. No diabetes. So yes - of course they didn’t develop hyperkalemia. That’s like saying ‘I ran a marathon on a treadmill and didn’t die’ - so everyone should be able to.
The real population? Elderly. Diabetic. CKD. Polypharmacy. That’s where the deaths occur.
And yet we generalize. We say ‘bananas are fine’ because some 30-year-old athlete is fine.
That’s not science. That’s dangerous populism.
Also - patiromer? 89% success rate? That’s not a cure. That’s a band-aid on a hemorrhage. You’re still on the drug. You’re still at risk. You’re just paying $800/month to keep the system running.
Real solution? Don’t give the drug to people with high risk. Use ARBs. Or don’t prescribe it at all.
Stop blaming the fruit. Start blaming the protocol.
Kaye Alcaraz
February 28, 2026 AT 02:28Thank you for this comprehensive and clinically accurate overview.
The guidance provided is both evidence-based and compassionate.
Regular monitoring, individualized risk assessment, and patient education are the cornerstones of safe pharmacotherapy.
It is imperative that clinicians prioritize potassium testing prior to initiation and during ongoing management of ACE inhibitors - particularly in vulnerable populations.
Furthermore, dietary counseling should be framed not as restriction, but as empowerment - offering alternatives rather than elimination.
This is the model of care we must champion.
Sarah Barrett
March 1, 2026 AT 11:06Interesting how the narrative shifts from ‘avoid potassium’ to ‘manage potassium.’
That’s progress.
For years, patients were told to cut out entire food groups - only to later learn that moderation was the goal all along.
Now we’re moving toward precision: genetic markers, targeted testing, gut binders.
The future isn’t fear. It’s personalization.
One size no longer fits all.
And that’s a good thing.
Erica Banatao Darilag
March 2, 2026 AT 09:15i just wanted to say thank you for this post. i’ve been on lisinopril for 3 years and i didn’t know any of this. i’ve been eating bananas every morning and i thought it was healthy. now i’m going to get my potassium checked. i’m so glad i read this.
you’re helping people. really.
Charlotte Dacre
March 3, 2026 AT 11:58Wow. A nurse actually said she’s seen 12 people hospitalized over coconut water? That’s wild. I thought I was the only one who thought that stuff was a scam. Now I’m gonna stop buying it. Also - who markets coconut water as a ‘health drink’? That’s like selling sugar water in a fancy bottle and calling it ‘vitality.’
Also - why do doctors never tell you this stuff? I’ve been on lisinopril for 2 years. My doctor never mentioned potassium. Not once. Not even when I asked about my diet.
So… who’s responsible here? The patient? The doctor? The system?
Also - I just checked my fridge. I have 3 bananas. One avocado. A jar of tomato sauce. And a bottle of coconut water.
Guess I’m having a very boring breakfast tomorrow.
Josiah Demara
March 5, 2026 AT 00:53Exactly. Doctors don’t have time. They’re on a 10-minute clock. And they’re not trained in nutrition. They’re trained in pills.
So they prescribe the drug. And hope the patient doesn’t eat too much fruit.
That’s not healthcare. That’s negligence wrapped in a white coat.
And patients? They’re told to ‘eat healthy’ - without being told what ‘healthy’ means in this context.
We’re failing people. Systemically.