Why Ventolin Reliance Is a Red Flag: Understanding Its Limits
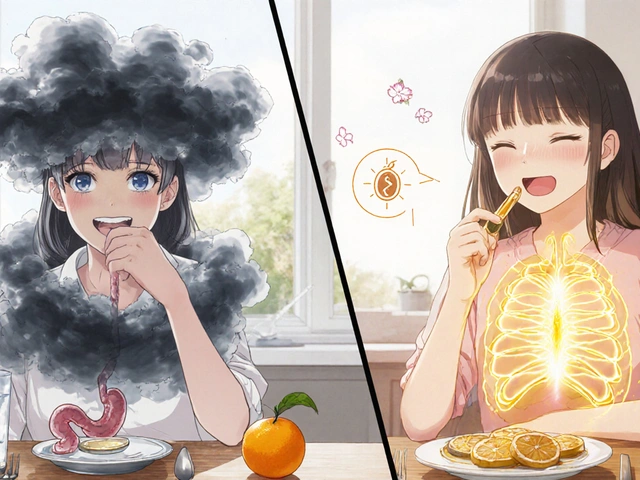
The world is obsessed with quick fixes. Just see how many people reach for their blue inhaler whenever their chest tightens. But living from puff to puff? That's not exactly an asthma management plan—it's just crisis control. The real story of Ventolin (that’s albuterol, for the science nerds or worried parents) is sort of like living with a fire extinguisher. Super helpful in an emergency, but if you keep needing it, you probably have bigger issues at home.
Doctors use a benchmark when discussing Ventolin: using your inhaler more than two days a week (outside of exercise) is a wake-up call. That’s not something the packaging says in big red letters, but it comes up a lot in clinics. Research published in the New England Journal of Medicine says people in the “frequent user” category run a higher risk for serious asthma attacks. And—this is not fun—overuse of Ventolin can even make asthma symptoms worse for some people by masking a poorly controlled disease.
So what’s the deal? Ventolin is not a preventative medicine. It relaxes airways, but it doesn't fix the inflammation underneath. Kind of like using ice to bring down a fever when you have the flu—nice, but missing the root cause. That’s why asthma guidelines (the GINA 2024 update is worth a scroll if you’re wonky) urge people to look beyond just “relief” and focus on long-term control. No one should feel held hostage by a rescue inhaler.
People get stuck in this loop for lots of reasons—panic, convenience, not seeing their doctor enough. Some even forget what normal breathing feels like. Quiz time: When did you last go a week without reaching for your inhaler? If that question makes you cringe, you’re not alone. But it’s exactly why experts are now pushing combination therapies to break this pattern.
The Power Duo: LABA and ICS Explained
Combination therapy sounds fancier than it is. It's about pairing meds that complement each other for better results. In asthma, two of the most powerful weapons are long-acting beta-agonists (LABA) and inhaled corticosteroids (ICS). The LABA acts like a long, slow muscle relaxer for your airways, keeping them open for hours—not just minutes. ICS, on the other hand, is like a peacekeeper, quelling the inflammation that keeps flaring up inside your lungs.
The reason this pair shows up everywhere in guidelines? Because the numbers don’t lie. Multiple clinical trials have shown that people using both LABA and ICS have way fewer asthma attacks and, crucially, less need for their albuterol rescue inhalers. For example, one study in Chest found that adding salmeterol (a common LABA) to fluticasone (a popular ICS) cut severe flare-ups by more than 30% after just three months.
Here’s what it looks like in daily life: Instead of feeling your breathing tighten and rushing for quick relief, you pop open your combination inhaler—commonly known by brand names like Symbicort or Advair—once in the morning and once at night. That’s it. Most people notice their symptoms get quieter, their sleep improves, and their energy stays steadier. And unless you’re in a dusty attic with Oliver the cat or powering through a tough spring allergy season, you start to forget where your rescue inhaler even is.
A handy way to remember how these work: LABA keeps the door open, ICS keeps the angry neighbors (i.e., inflammation) from setting your house on fire in the first place.
One warning—and doctors will drive this home—never use a LABA by itself for asthma. Alone, LABAs might actually increase asthma-related deaths (grim, but true). That’s why they’re always paired with ICS, so your airways stay both relaxed and calm, not just one or the other.
Sticking to your routine is key. If you only use the combo when you feel bad, you lose the full benefits. Treat it like brushing your teeth: not glamorous, but essential.
For those keeping score, here’s a cheat sheet of common LABA/ICS combos:
- Advair Diskus: fluticasone/salmeterol
- Symbicort: budesonide/formoterol
- Breo Ellipta: fluticasone/vilanterol
Asthma control gets a major upgrade with these combos. No Cape required.

The Next Generation: Biologics for Severe Asthma
For some folks, even combination inhalers just aren’t enough. When you’re still wheezing and your rescue inhaler is your shadow, it’s time for a new approach: biologics. If that word makes you picture sci-fi labs and vials, you’re not wrong—but these therapies are already changing lives in real clinics.
Biologics are a type of medication made from living cells. Unlike regular asthma meds that hit broad targets, biologics are more like a sniper, zeroing in on specific molecules that trigger severe asthma. You get them by injection, most often every 2-8 weeks (with a nurse’s help unless you’re brave enough for at-home shots).
The main players in the biologics world target parts of your immune system that go haywire in some types of asthma. Here are the top names doctors are talking about:
- Omalizumab (Xolair): blocks immunoglobulin E (IgE), key for people with allergic asthma.
- Mepolizumab (Nucala), Reslizumab (Cinqair), Benralizumab (Fasenra): shut down eosinophils, a type of white cell that stirs up airway inflammation.
- Dupilumab (Dupixent): hits a couple of signals (IL-4 and IL-13) that mess with your airways in “Type 2” inflammation.
In clinical practice, about 65-75% of patients using biologics for severe asthma experience a sharp drop—not just in symptoms, but in ER visits too. A major study in The Lancet found people on Benralizumab reduced their use of rescue inhalers by almost 60% over a year. Asthma attacks often drop by at least half, sometimes more. For my cousin—who is allergic to half the planet and owns three cats—biologics were the only therapy that got him off the constant cycle of steroids and misery.
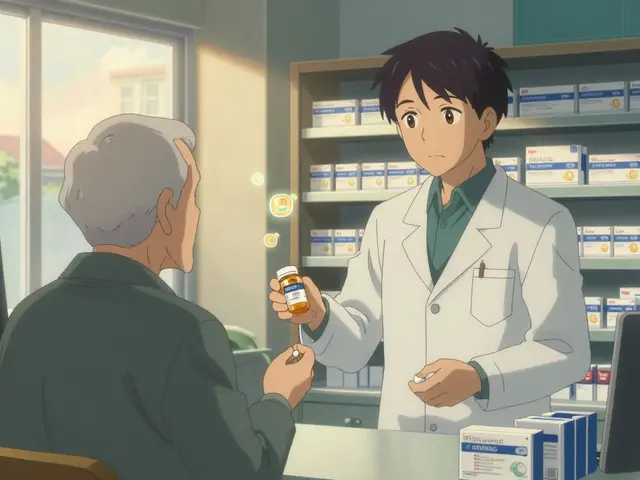
Biologics aren’t for everyone. They're expensive, require testing (mostly blood work to see what flavor of asthma you’ve got), and they work best in tough, hard-to-treat asthma, not mild cases. But if you’re tired of taking five different meds and still struggling, these are absolutely worth a discussion with your doctor.
Here’s what’s wild: dozens of new biologics are in the pipeline, promising more personalized care. Don't be surprised if your next asthma visit includes talk of genetic testing and new blood markers—science keeps raising the bar for asthma care.
Practical Ways to Break Rescue Inhaler Habits
Getting off the “blue puffer treadmill” takes more than fancy prescriptions—it’s about changing daily habits too. That sounds obvious, but it’s weirdly hard in real life. If you’re like most people, the emotional comfort of knowing Ventolin is tucked in your bag or nightstand can be tough to give up. It’s psychological as much as physical. How do you actually reduce your Ventolin dependence day to day?
- Stick to a Schedule: Use your controller inhaler at the same time every day—even if you feel fine. Set a phone alarm. It helps retrain your body and mind to expect steadier relief.
- Track Your Symptoms: Keep a diary (apps work too) and note when you need Ventolin. See if you spot patterns—maybe it’s always after cleaning Oliver’s litter box or during allergy season.
- Identify Triggers: Allergy-proof your space. Use HEPA filters, keep windows shut when pollen is high, and don’t go full Marie Kondo when dust is flying. Give your pets—and yourself—a bath more often during flare-up months.
- Work on Breathing: Asthma-specific breathing exercises (like Buteyko or even simple pursed-lip breathing) can help you manage mild shortness of breath, so you don’t reflexively reach for your inhaler at every twinge.
- Team Up with Your Doc: Have a clear asthma action plan. Know exactly when you should increase meds, call for help, or just ride it out.
If you’re still using your rescue inhaler more than twice a week, it’s not a “personal failing”—it’s a sign your current plan needs a tune-up. No one should have to live like you’re always one skipped puff away from trouble.

Exploring Alternatives and the Future of Asthma Control
It’s tempting to believe there’s only one way to manage asthma, especially if “the blue inhaler” was the only option for years. But new research, fresh guidelines, and dozens of new medications are turning that into old news. If you’re curious about your other options, there’s a great roundup of Ventolin alternatives that covers some non-albuterol choices on the market. Some of these are available as combination inhalers, while others work through entirely different mechanisms.
There’s genuine excitement about






Jimmy Gammell
July 17, 2025 AT 22:19Hey, this is such a timely post! 😃 For many of us who have been relying on Ventolin for quick relief, hearing about combination therapies sounds like a game changer. It’s so cool that LABA and ICS together can reduce the constant need for that immediate puff. I’ve seen some friends struggle with the overuse of quick-relief inhalers, and a better long-term strategy would be fantastic.
What I really appreciate is the part about biologics because I didn’t know they could help control asthma better. I’m wondering how accessible those are, especially here where sometimes medications are hard to get. Thanks for sharing practical tips too—it makes me feel like managing asthma can be less stressful with the right info.
Anyone else tried switching from just Ventolin to a combo therapy? Would love to hear experiences! 😊
fred warner
July 20, 2025 AT 06:16This article is spot on! The quick-relief inhalers like Ventolin are great in emergencies, but they're not a cure or a solution for long-term control. Combination therapies including LABA (Long-Acting Beta Agonists) and ICS (Inhaled Corticosteroids) have been proven to stabilize asthma symptoms significantly. The fact that biologics are introduced as an option marks an exciting era in treatment, especially for severe asthma cases.
The key takeaway here is that we need to move away from the quick-fix mentality and look at asthma management holistically. Also, it's exciting how real patients are sharing their success stories with these new treatments – very encouraging stuff!
I'd recommend anyone struggling with this to start a conversation with their healthcare provider about these options. It might be the difference between constant symptoms and real quality of life improvements.
Veronica Mayfair
July 21, 2025 AT 06:18Omg, this article speaks my language! 🙌 I feel like I've been chained to my Ventolin inhaler for years, always worried if I had enough when heading out. Learning about how combination treatments and biologics offer better long-term control gives me hope. It's so important to break free from that "quick fix" cycle because it can be exhausting and worrying.
Real-life stories in articles like this really help to motivate me to chat with my doc about trying a combination approach. I've been so scared about starting new treatments, but seeing that others have found success actually vibes with me emotionally. 💪
Plus, that mix of LABA and ICS sounds like a powerful duo—anyone know if biologics have any big side effects? Thanks for this info, seriously needed it. 🙂✨
Rahul Kr
July 26, 2025 AT 03:40Interesting stuff here. I appreciate the calm approach in talking about new therapies rather than excitement for quick fixes. Combination therapies like LABA and ICS have been around and are well studied which gives a comforting sense of safety.
Biologics as a long-term option is intriguing but probably expensive in many places. Accessibility is a key factor; not everyone can afford such treatments, and that might limit options. Also, it’s important that patients understand the practicalities, like adherence, correct inhaler technique, and potential side effects.
Any of you here have thoughts on how these new options are being received in different healthcare systems? Would love a global perspective on this.
Anthony Coppedge
July 28, 2025 AT 15:40This is a well-needed conversation! Over-reliance on fast-acting inhalers like Ventolin can mask the underlying inflammation that really needs treatment. That's why the role of ICS in combination therapy is crucial—it addresses inflammation rather than just relieving symptoms.
Adding LABA helps maintain smoother air flow over time, avoiding those sudden asthma flare-ups. And biologics? They represent a newer frontier targeting specific immune pathways. They’re not a first line, but for some people, they’re a significant breakthrough.
It’s essential, however, that patients stick to prescribed therapies and don’t overuse rescue inhalers. Education on this topic can’t be emphasized enough. This post is a good step to getting the word out.
Joshua Logronio
July 30, 2025 AT 18:13Not to throw a wrench in the conversation, but sometimes I wonder about the pharmaceutical industry’s motives behind pushing expensive biologics and combo therapies. Are they really about patient care or mostly profit? 🤔
That being said, I do get that newer treatments can help folks breathe better. I’m just always cautious about blindly trusting new drugs without questioning the system behind them. Have any of you looked into the financial side or clinical trial data closely?
Still, better options are needed, especially beyond constant Ventolin use, but we should stay vigilant about all factors involved.
Suzanne Podany
August 3, 2025 AT 04:26It's wonderful to see this kind of discussion happening! Asthma care is evolving and inclusion in these conversations is key to spreading awareness. Combination therapies indeed offer a more balanced approach to asthma control, and the use of biologics, while newer, has been a life-changing option for many, especially those with severe asthma.
Access and affordability remain challenges but knowledge-sharing empowers patients to advocate for themselves. Encouraging patients to discuss all options, including lifestyle management and avoidance strategies, is equally important.
Let's keep this positive momentum going. Every breath matters!
Steve Ellis
August 9, 2025 AT 11:33This post really hits home for me. I struggled for years with uncontrolled asthma simply because I relied too much on my Ventolin inhaler. It gave immediate relief, sure, but it never stopped episodes from coming back. Switching to a combination therapy was a literal breath of fresh air — I can't stress enough how much easier everyday life has become.
Biologics came into the picture when I hit a severe state, and I was skeptical, but my doctor explained how they target what causes the inflammation. Getting off that rollercoaster of symptoms felt like reclaiming my freedom. If anyone is reading this and feeling trapped by their current asthma situation, please know there are better paths out there.
Lindsey Bollig
August 12, 2025 AT 14:00Great article! Managing asthma long-term is all about consistent control rather than short bursts of relief. I always tell my patients to never view Ventolin as the primary means of control but as an emergency aid. Combination therapies like LABA and ICS have a solid evidence base and are recommended in guidelines worldwide.
Biologics, while promising, should be reserved for those who don’t get control from standard treatments due to cost and availability. Patients must work closely with their healthcare team to find the right approach tailored to their condition and lifestyle.
If you’re considering switching your asthma management plan, discuss it thoroughly with your doctor first.
Daniel Buchanan
August 14, 2025 AT 16:00This is a really crucial conversation. People with asthma often don't realize that relying on Ventolin frequently can mean that their underlying inflammation isn't being treated properly. Combination therapies with ICS and LABA address this issue effectively. Moreover, biologics represent a precision medicine approach that can be a game changer for severe asthma patients.
But I want to add that lifestyle factors and trigger avoidance still play a big role.
Has anyone seen improvement simply by combining medical treatment with reducing environmental triggers? Just throwing ideas out there.
Dipak Pawar
August 16, 2025 AT 12:26Expanding on what others have shared here, the integration of combination therapy and biologics marks a remarkable advance in respiratory pharmacology. The pathophysiological basis underlying asthma involves chronic airway inflammation, bronchial hyperresponsiveness, and airway remodeling. Long-acting beta-agonists synergize with inhaled corticosteroids to suppress these processes, reducing exacerbations.
Biologics, such as monoclonal antibodies, selectively target immune mediators like IgE or IL-5, tailoring treatment to specific asthma phenotypes. While clinical efficacy is well-documented, socioeconomic and logistic barriers hinder widespread uptake, calling for a multidisciplinary approach involving policy makers, clinicians, and patient advocates.
Further, longitudinal data collection is essential to map real-world outcomes and optimize protocols moving forward.
Anthony Coppedge
August 16, 2025 AT 22:19Thanks for the great discussions here, everyone. To add a bit on adherence and technique - many patients have difficulties using inhalers properly, which can compromise treatment effectiveness. It’s vital to ensure patients are trained and supported.
Regarding biological drugs, I’d recommend looking into their mechanism and clinical trial profiles to allay fears and understand risks and benefits better. And yes, discussing financial implications is necessary too, as previously mentioned.
Ultimately, treatment plans must be as personalized as possible, based on severity, triggers, comorbidities, and patient preferences.